Cardiovascular
AI Analysis Will Predict Future Disease from Bone Density Scans
Researchers have used machine learning to assess bone density scans for calcification in the aorta, the body’s main artery. They say their method could be used to predict future cardiovascular and other disease, even before symptoms appear.
Just as calcification, or the deposit of calcium, on the inner wall of blood vessels in the heart can be problematic, so can calcification of the aorta, the largest artery in the body. Exiting the heart, it branches upward to supply blood to the brain and arms and extends down to the abdomen, where it splits into smaller arteries that supply each leg.
Abdominal aortic calcification (AAC), calcification in the section of the aorta that runs through the abdomen, can predict the development of cardiovascular diseases such as heart attack and stroke and determine mortality risk. Previous studies have also found that it’s also a reliable marker for late-life dementia. AAC is visible on bone density scans typically used to detect osteoporosis in the lumbar vertebrae, but a highly trained professional is required to analyze these images, which takes time.
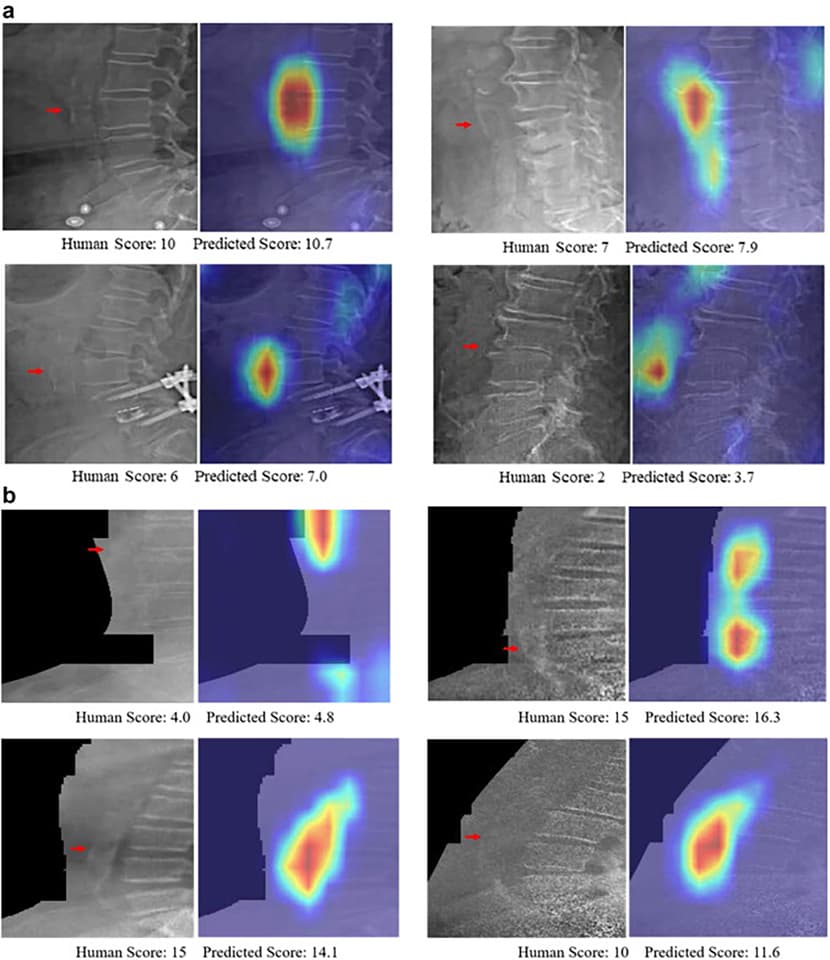
AAC is commonly quantified by trained imaging specialists using a 24-point scoring system, AAC-24. A score of zero represents no calcification, and a score of 24 represents the most severe degree of AAC. Now, researchers from Edith Cowan University in Australia have turned to machine learning to speed up the calcification assessment and scoring process.
The researchers input 5,012 spinal images, taken by four different models of bone density machines, into their machine learning model. Though other algorithms have been developed to assess AAC from these types of images, the researchers say this study is the biggest and the first to be tested in a real-world setting using images taken from routine bone density testing.
They then assessed the model’s performance in accurately classifying images into low, moderate and high categories of calcification based on their AAC-24 score. To check for accuracy, the machine-learning-based AAC scores were compared with scores given by human specialists. The specialist and the software arrived at the same determination 80% of the time. Three percent of people with high AAC scores were incorrectly diagnosed as having low scores by the software.
Sharif et al./Edith Cowan University
“This is notable as these are the individuals with the greatest extent of disease and highest risk of fatal and nonfatal cardiovascular events and all-cause mortality,” Lewis said. “Whilst there is still work to do to improve the software’s accuracy compared to human readings, these results are from our version 1.0 algorithm, and we already have improved the results substantially with our more recent versions.”
The researchers say their machine-learning algorithm can analyze bone density scans at a rate of roughly 60,000 images per day. It’s a vast improvement when you consider that it takes the average specialist between five and 15 minutes to analyze a single image.
“Since these images and automated scores can be rapidly and easily acquired at the time of bone density testing, this may lead to new approaches in the future for early cardiovascular disease detection and disease monitoring during routine clinical practice,” said Joshua Lewis, corresponding author of the study.
And the researchers say their screening method could be used to screen for diseases before symptoms arise.
“Automated assessment of the presence and extent of AAC with similar accuracies to imaging specialists provides the possibility of large-scale screening for cardiovascular disease and other conditions – even before someone has any symptoms,” said Lewis. “This will allow people at risk to make the necessary lifestyle changes far earlier and put them in a better place to be healthier in their later years.”
The study was published in the journal eBioMedicine.
Source: Edith Cowan University