Cancer and neoplasms
Robotic surgery linked to longer survival vs. chemoradiation for oropharyngeal cancer
July 18, 2023
2 min read
Source/Disclosures
Published by:
Disclosures:
Amin reports no relevant financial disclosures. Please see the study for all other authors’ relevant financial disclosures.
Key takeaways:
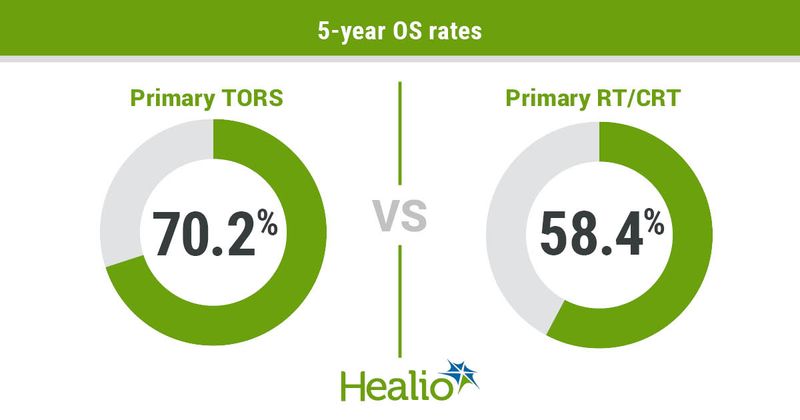
- Patients who received transoral robotic surgery had a higher 5-year OS rate.
- Patients who received radiation therapy and/or chemoradiation had a higher risk for gastrostomy tube dependence.
Primary transoral robotic surgery appeared associated with greater risk for short-term dysphagia compared with primary radiotherapy or chemoradiotherapy among patients with T1-T2 oropharyngeal squamous cell carcinoma, study results showed.
However, patients who received radiotherapy or chemoradiotherapy had a higher likelihood of gastrostomy tube dependence for several years after treatment and shorter OS than those who underwent surgery, according to the findings, published in JAMA Otolaryngology-Head & Neck Surgery.
Background and methodology
Limited data exists to illustrate differences in functional and survival outcomes of patients with oropharyngeal squamous cell carcinoma who receive either primary transoral robotic surgery (TORS) or primary radiation therapy and/or chemoradiation therapy, according to researchers.
“Utilizing TORS as a tool to de-escalate adjuvant therapy has been successful in decreasing toxic effects in patients with low-to-intermediate-risk disease who met acceptable progression-free survival thresholds,” Dev R. Amin, MD, resident physician at Thomas Jefferson University Hospital, and colleagues wrote. “Controversy remains regarding survival and functional outcomes between primary TORS plus adjuvant therapy and primary [chemoradiotherapy] in the definitive and de-escalated settings given the paucity of data from high-powered [randomized controlled trials].”
Researchers conducted a national, multicenter cohort study comparing 5-year functional and survival outcomes in patients with T1-T2 oropharyngeal squamous cell carcinoma who received either primary TORS or primary radiation therapy and/or chemoradiation therapy. They obtained data from a global health network on patients treated between 2002 and 2022.
A total of 726 patients met inclusion criteria after propensity matching, including 363 (mean age, 68.5 years; 86% white; 79% men) in the TORS cohort and 363 (mean age, 68.8 years; 88% white; 79% men) in the radiation therapy and/or chemoradiation therapy cohort.
Researchers measured functional outcomes, including dysphagia, gastrostomy tube dependence and tracheostomy dependence, at 6 months, 1 year, 3 years, 5 years and more than 5 years after treatment. The also compared 5-year OS between the groups.
Results
Primary TORS appeared associated with a clinically meaningful increased risk of dysphagia at both 6 months (OR = 1.37; 95% CI, 1.01-1.84) and 1 year (OR = 1.71; 95% CI, 1.22-2.39) after treatment compared with primary radiation therapy and/or chemoradiation therapy.
Patients who received surgery had a lower likelihood of gastrostomy tube dependence at 6 months (OR = 0.46; 95% CI, 0.21-1) and 5 years posttreatment (risk difference, 0.05; 95% CI, 0.07 to 0.02).
Researchers found no clinically meaningful differences in overall rates of tracheostomy dependence between the groups (OR = 0.97; 95% CI, 0.51-1.82).
Patients unmatched for cancer stage or HPV status who received primary radiation therapy and/or chemoradiation had a lower 5-year OS rate than patients who received primary surgery (58.4% vs. 70.2%; HR = 0.56; 95% CI, 0.4-0.79).
Next steps
Further studies should evaluate the effect of both treatment options based on HPV status, according to researchers.
“The current study sample comprised patients with both HPV-mediated and HPV-negative [oropharyngeal squamous cell carcinoma], as reflected by the reduced 5-year survival rates,” researchers wrote. “The results favoring TORS for [oropharyngeal squamous cell carcinoma] management are likely skewed by the nonradiosensitive HPV-negative [oropharyngeal squamous cell carcinoma] population. More randomized clinical trials are required to elucidate survival rates in patients with HPV-mediated vs. HPV-negative [oropharyngeal squamous cell carcinoma] treated with TORS vs. [radiation therapy and/or chemoradiation].”