Infection
Study shows how NSAIDs exacerbate C. difficile infections
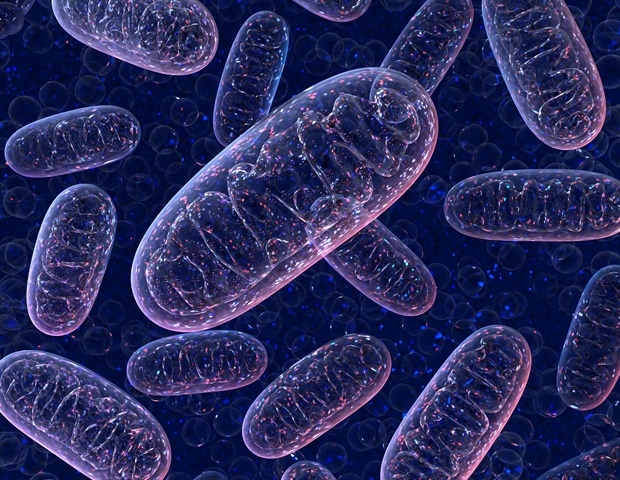
Why do nonsteroidal anti-inflammatory drugs (NSAIDs) exacerbate gastrointestinal infections by Clostridioides difficile, the leading cause of antibiotic-associated diarrhea worldwide? In a new paper published in Science Advances, researchers at Children’s Hospital of Philadelphia (CHOP) have begun to answer that question, showing that NSAIDs disrupt the mitochondria of cells lining the colon, sensitizing them to damage by pathogenic toxins.
Clostridioides difficile, often referred to as C. difficile or C. diff, is a bacterium that leads to a wide range of symptoms, from mild diarrhea to complex infection and death. The factors that influence this wide spectrum of clinical outcomes remain largely unclear, but emerging evidence suggests that factors like diet and pharmaceutical drugs influence both susceptibility to infection and disease progression. However, researchers still know very little about how these factors impact the course of C. difficile infection.
Prior studies have shown that NSAIDs like indomethacin, aspirin, and naproxen negatively affect the gut, both in patients with C. difficile infection and other conditions like inflammatory bowel disease (IBD). Long-term NSAID use can lead to stomach ulcers and intestinal injuries, like bleeding and perforation of the intestinal tissue. Researchers hypothesize this is due to the effects of NSAIDs on cyclooxygenase (COX) enzymes; a process that helps reduce inflammation and pain but also impairs mucosal function in the upper gastrointestinal tract. However, NSAIDs also have off-target effects and have been shown to affect cellular mitochondria by uncoupling cellular mitochondrial functions, but researchers had not explored the mechanism or impact of these off-target effects when it comes to C. difficile infection.
To define these effects, the researchers, led by graduate student Joshua Soto Ocaña, used in vitro and mouse models of C. difficile infection to test how permeable colonic epithelial cells are in the presence of the NSAID indomethacin. The researchers observed that both indomethacin and a C. difficile toxins increased epithelial cell barrier permeability and inflammatory cell death. They also found that the effect was additive: the combined effect on cell permeability of both toxins and indomethacin was increased compared to each independently, suggesting NSAIDs and C. difficile work synergistically to increase the virulence of this pathogen.
Surprisingly, the researchers found that NSAIDs exacerbate C. difficile infection independent of COX inhibition and instead through off-target effects on mitochondria. They did so by treating colonic epithelial cells with a precursor molecule that is similar in structure to indomethacin but lacks the ability to inhibit the COX enzyme. Not only did they find that this NSAID-like molecule induced cell death, but they also found that adding selective COX inhibitors did not increase cell death, demonstrating that COX enzyme inhibition is not required to induce epithelial cell damage during C. difficile infection and that, instead, this damage occurs through off-target effects of NSAIDs.
To test the role of off-target effects during C. difficile infection, the researchers used mice pretreated either with indomethacin or the NSAID-precursor molecule. When exposed to C. difficile, both groups of mice showed equal enhancement in disease severity and mortality compared to untreated control mice infected with C. difficile only. The researchers also observed a similar effect in mice who were pretreated with the NSAID aspirin. To further define the specific mechanisms driving these off-target effects of NSAIDs, researchers looked at mitochondrial functions in colonic epithelial cells in vitro and in mice. They observed that the combination of NSAIDs and C. difficile toxins increased damage to colonic epithelial cell mitochondria and disrupted several important mitochondrial functions.
Our work further demonstrates the clinical importance of NSAIDs in patients with C. diff infection and sheds light on why the combination of these two may be so detrimental. Our mechanistic findings are a starting point for further research that aims to understand the impact of mitochondrial functions during C. diff infection. These data could also inform how NSAID-mediated mitochondrial uncoupling affects other diseases, such as small intestinal injury, IBD, and colorectal cancer.”
Joseph P. Zackular, PhD, Senior Author, Investigator and Assistant Professor of Pathology and Laboratory Medicine at Children’s Hospital of Philadelphia
Children’s Hospital of Philadelphia
Soto-Ocaña, J., et al. (2023) Nonsteroidal anti-inflammatory drugs sensitize epithelial cells to Clostridioides difficile toxin–mediated mitochondrial damage. Science Advances. doi.org/10.1126/sciadv.adh5552.