Infection
Progress Toward Hepatitis B Control and Elimination …
Results
Immunization Activities
By 2014, all 47 countries in AFR had introduced HepB3 infant vaccination (Table 1). By December 2021, 14 (30%) countries provided HepB-BD, eight (57%) of which were in the West subregion.¶¶ Although 10 countries had introduced HepB-BD before 2016, only four (Benin, Côte d’Ivoire, Equatorial Guinea, and Senegal) introduced HepB-BD during 2016–2021. During this period, regional HepB3 coverage ranged from 75% in 2019 to 71% in 2021. Eighteen (38%) countries reached ≥90% HepB3 coverage in 2016; this number peaked at 20 (43%) in 2018; by 2021, the number of countries with ≥90% HepB3 coverage had declined to 16 (34%); nine of these countries were in the East and South subregions. Regional HepB-BD coverage increased from 10% in 2016 to 17% in 2021. During 2016–2021, Algeria and Cabo Verde reached HepB-BD coverage of ≥90%, and Namibia and Senegal achieved ≥50% coverage.
HBsAg Seroprevalence Surveys
Because most chronic HBV infections (particularly those among young children) are asymptomatic, the impact of hepatitis B vaccination is usually measured by HBsAg seroprevalence among children born after the introduction of HepB, usually those aged ≤5 years*** (3,6). During 2016–2021, HBsAg seroprevalence surveys among children were conducted at national or regional levels in eight (17%) countries. Among children of various age ranges surveyed in Ethiopia, Mauritania, Rwanda, Sierra Leone, Uganda, and Zambia, HBsAg seroprevalence was ≤2%. Prevalence among children aged ≤5 years measured in the Democratic Republic of the Congo, Ethiopia, Mauritania, Nigeria, and Sierra Leone ranged from 0.7% (Mauritania) to 4.5% (Nigeria) (Table 2). No country achieved ≤0.1% HBsAg seroprevalence among children. Modeling studies estimated a HBsAg seroprevalence of 2.5% (95% CI = 1.7–4.0) among children aged ≤5 years in AFR, accounting for more than two thirds (4.3 million, approximately 69%) of all infected children worldwide (1).
HBsAg seroprevalence among women of reproductive age or pregnant women provides an estimate of the risk for MTCT of HBV. Data from population-based HBsAg surveys among women of reproductive age or from screening of pregnant women available from 11 countries showed HBsAg seroprevalences ranging from 1.2% (Rwanda) to 9.8% (Sierra Leone) (Table 2).
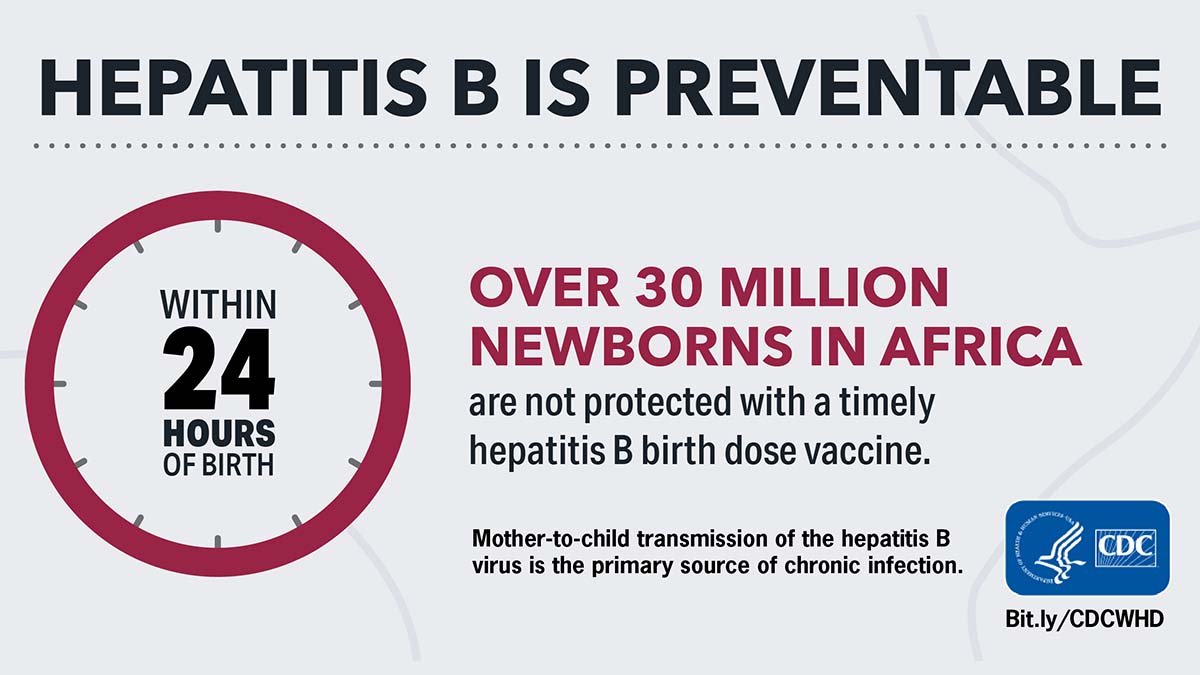
Elimination of Mother-to-Child Transmission of HBV
By December 2021, although 21 (45%) AFR countries had developed a plan for EMTCT of HIV, syphilis, and HBV, only six countries††† reported having implemented the EMTCT guidelines for routine HBsAg testing of pregnant women, provision of antiviral medications to eligible (HBsAg-seropositive) women,§§§ and administration of HepB-BD to newborns. As of December 2021, ≥90% of pregnant women in 29 (62%) AFR countries had at least one antenatal care visit (Table 3). Data from the most recent nationwide surveys showed that in 37 (79%) countries, approximately one half of women gave birth in health care facilities, and in 23 (49%) countries, ≥80% of women delivered in a health facility (Table 1). To acknowledge progress toward EMTCT of HBV in countries with high endemicity, WHO developed a certification mechanism for the path to elimination of MTCT of HBV, using three tiers (bronze, silver, and gold) indicating increasing levels of progress¶¶¶ (6). Based on HepB immunization interventions in 2021, Botswana might be eligible for the bronze tier, three countries (Namibia, Sao Tome and Principe, and Senegal) might be eligible for the silver tier, and two countries (Algeria and Cabo Verde) might be eligible for the gold tier certification (Table 1) (Table 3).