Cardiovascular
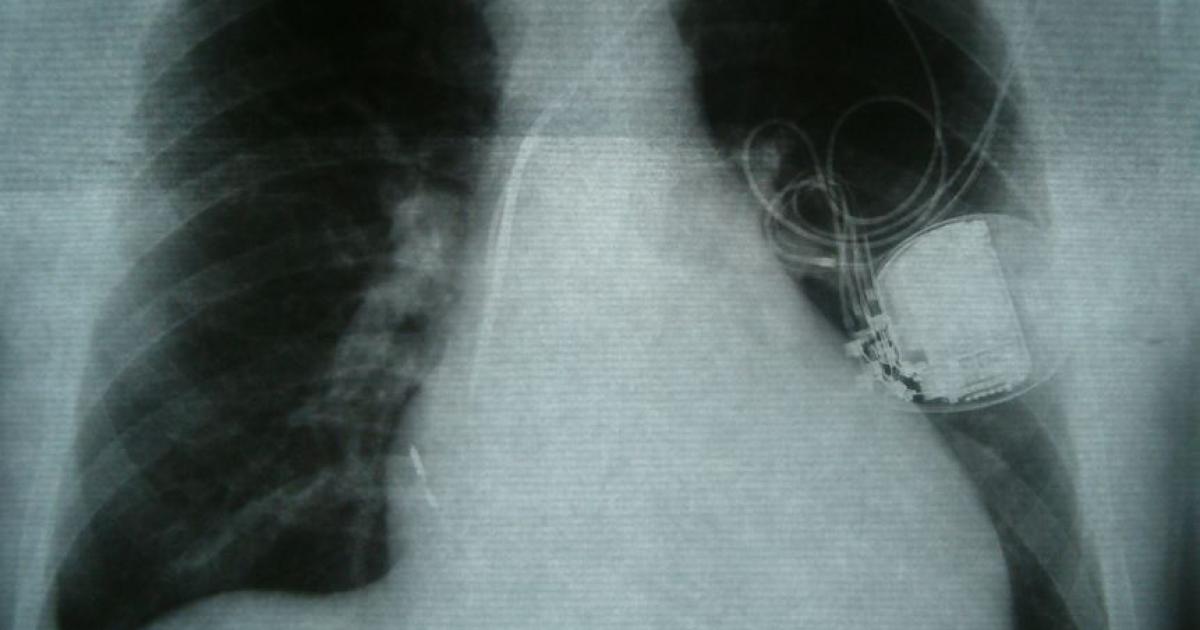
Permanent pacemakers after TAVR: Tracking the impact of modern self-expanding valves
Overall, PPI was required for 11.3% of TAVR patients within 30 days. This includes 8.8% of the 1,090 patients treated with the Acurate neo, 7.7% of the 665 patients treated with the Acurate neo2, 15.2% of the 1,312 patients treated with the Evolut Pro and 10.4% of the 144 patients treated with the Evolut Pro+.
PPI was more common among men than women. In addition, TAVR patients presenting with diabetes mellitus, right bundle branch block, a New York Heart Association functional class of III or IV or a history of coronary artery bypass graft all faced an increased risk of PPI. The same was also true for cases a lower depth of valve implantation.
Focusing on short-term outcomes, the authors found identified no significant differences when it came to all-cause mortality or cardiovascular mortality after 30 days. Also, left ventricular (LV) dysfunction, rehospitalization for valve-related symptoms and longer lengths of stay, however, were all more common among patients who would eventually require PPI.
A full year after TAVR, all-cause mortality and the combined outcome of all-cause mortality and cardiovascular-related rehospitalization were “significantly higher” among patients who required a PPI than those who did not.
“Careful THV selection and implantation seem crucial in patients at risk for new PPI, and alternative therapeutic options such as cardiac resynchronization therapy may be relevant in patients with LV dysfunction needing PPI after TAVR,” the authors concluded.
Read the full analysis here.