Blood
Umbilical cord white blood cells developed to advance cancer treatment
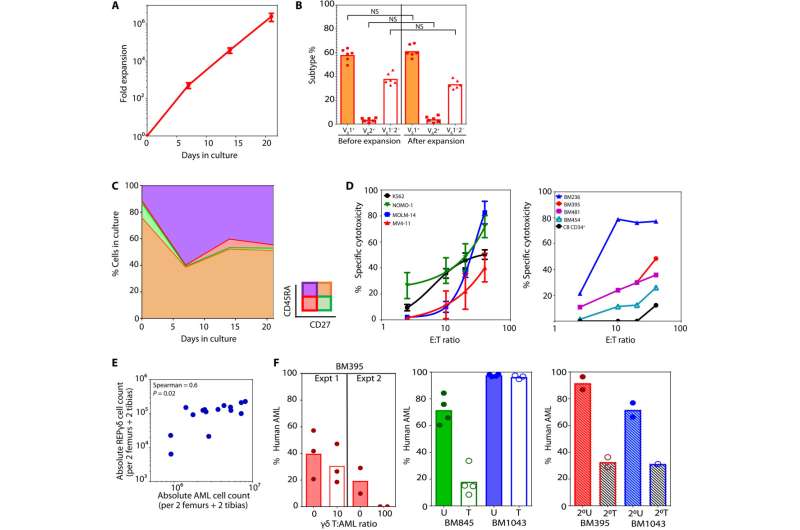
A team led by researchers from Department of Hematology and Department of Molecular Pathology, Singapore General Hospital (SGH) have developed a platform to harness and enhance the innate ability of white blood cells from umbilical cord blood to treat various types of solid and blood cancers. The platform performed well in pre-clinical studies and will be put to further test in a phase 1 clinical trial as early as 2024 for leukemia and lymphoma treatment.
The findings of this study are published in the journal Science Advances.
The white blood cells, known as gamma delta T-cells (GDT), have antiviral and antitumor properties. These cells keep a look out for signs of biological stress like cancerous or infected cells in the body and are one of the first lines of defense against disease.
GDT-cells can also be found in the blood of an adult. Pre-clinical studies, however, have reported that a specific sub-type of GDT-cells is more powerful against cancer cells and are found in greater numbers in umbilical cord blood as compared to GDT-cells in adults.
“Most initial efforts have been focused on exploring the use of gamma delta T-cells in adults as cancer treatment. Unfortunately, response rates in early clinical trials were generally low and treatment efficacies were sub-optimal. This was why we decided to turn our attention to umbilical cord blood instead,” said Assistant Professor Alice Cheung, Junior Principal Investigator, Department of Hematology, SGH, the senior author of the study.
Using umbilical cord blood samples from the Singapore Cord Blood Bank, the team developed processes for multiplying the number of GDT-cells in the samples. Cord blood cells are like newborn cells and the team postulates that these umbilical cord blood derived GDT-cells may have an extended lifespan that can potentially prevent or delay cancer relapses.
“Umbilical cord blood-derived GDT are akin to young warriors, potentially having longer lasting effects and being more adaptable to take on additional functions. However, they are currently under-utilized, with the main concern that there may not be enough of these T-cells for clinical application, but our study has shown that it is potentially feasible,” said Professor Goh Yeow Tee, Senior Consultant, Department of Hematology, SGH, and an author of the study.
More information:
Jeremy Wee Kiat Ng et al, Cord blood–derived V δ 2 + and V δ 2 − T cells acquire differential cell state compositions upon in vitro expansion, Science Advances (2023). DOI: 10.1126/sciadv.adf3120
SingHealth
Citation:
Umbilical cord white blood cells developed to advance cancer treatment (2023, July 27)
retrieved 27 July 2023
from https://medicalxpress.com/news/2023-07-umbilical-cord-white-blood-cells.html
This document is subject to copyright. Apart from any fair dealing for the purpose of private study or research, no
part may be reproduced without the written permission. The content is provided for information purposes only.