Blood
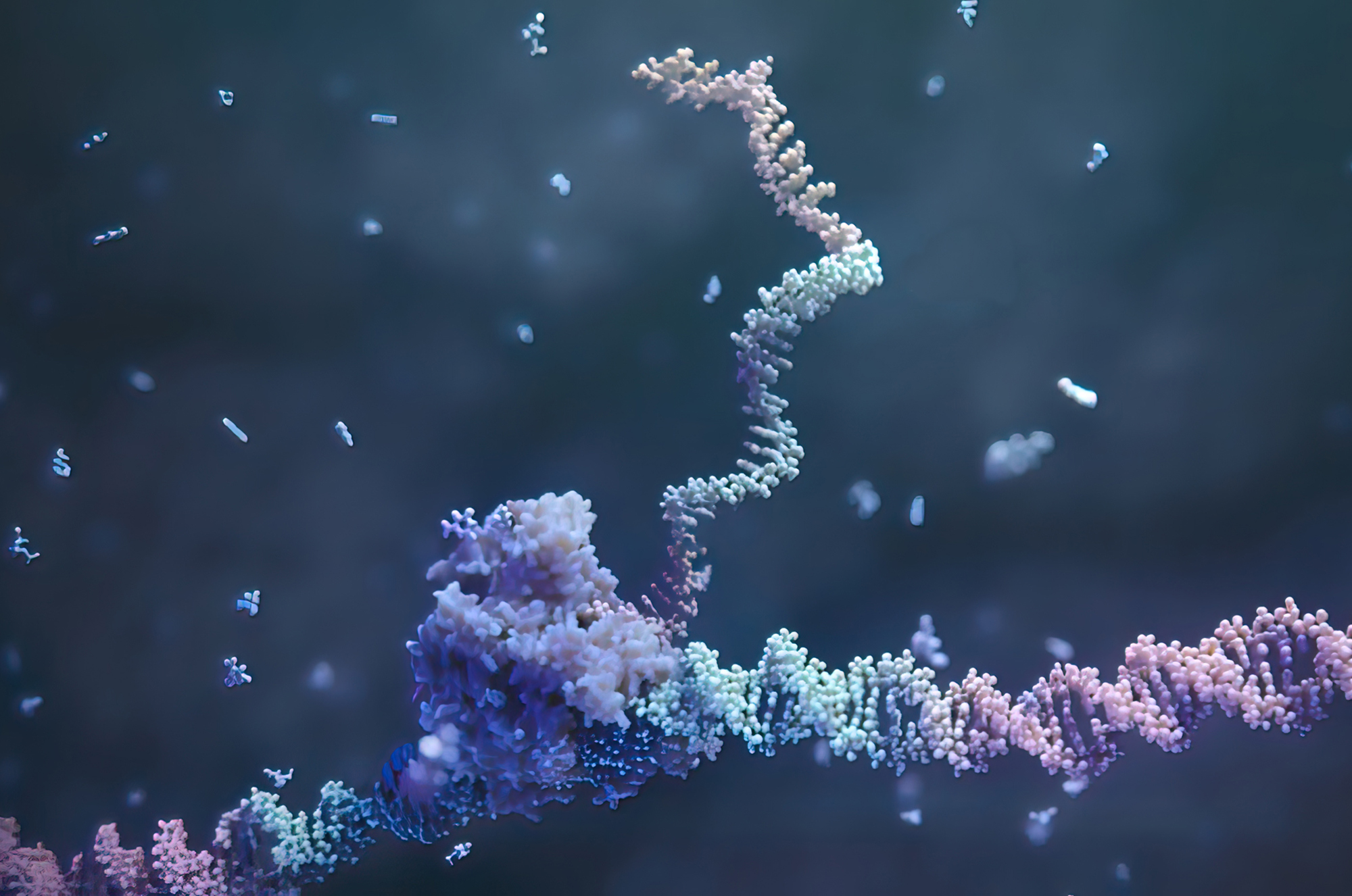
‘In vivo’ RNA-based gene editing model for blood disorders developed
In a step forward in the development of genetic medicines, researchers at the Perelman School of Medicine and Children’s Hospital of Philadelphia (CHOP) have developed a proof-of-concept model for delivering gene editing tools to treat blood disorders, allowing for the modification of diseased blood cells directly within the body. If translated into the clinic, this approach could expand access and reduce the cost of gene therapies for blood disorders, many of which currently require patients receive chemotherapy and a stem cell transplant. The findings are published in the journal Science.
“Targeted delivery of mRNA-encoded therapeutics to specific tissues and cell types will have an immense impact on the way diseases will be treated with nucleic acids in the future,” says senior author Hamideh Parhiz, a research assistant professor of infectious diseases at Penn. “In our study, we are providing a cell-specific targeted lipid nanoparticle encapsulating mRNA therapeutics/editors as a platform technology that can be used for in vivo cellular reprogramming in many diseases in need of a precisely targeted gene therapy modality. Here, we combined the targeted platform with advances in mRNA therapeutics and RNA-based genomic editing tools to provide a new way of controlling hematopoietic stem cell fate and correcting genetic defects. A targeted mRNA-encoded genomic editing methodology could lead to controlled expression, high editing efficacy, and potentially safer in vivo genomic modification compared to currently available technologies.”
Hematopoietic stem cells (HSCs) reside in the bone marrow, where they divide throughout life to produce all cells within the blood and immune system. In patients with non-malignant hematopoietic disorders like sickle cell disease and immunodeficiency disorders, these blood cells don’t function correctly because they carry a genetic mutation.
For these patients, there are currently two avenues for potentially curative treatments, both of which involve a bone marrow transplant: a stem cell transplant with HSCs from a healthy donor, or gene therapy in which the patient’s own HSCs are modified outside of the body and transplanted back in. The former approach comes with the risk of graft versus host disease, given that the HSCs come from a donor, and both processes involve a conditioning regimen of chemotherapy or radiation to eliminate the patient’s diseased HSCs and prepare them to receive the new cells. These conditioning procedures come with significant toxic side effects, underscoring the need to investigate less-toxic approaches.
“Right now, if you want to treat hematologic diseases like sickle cell disease and beta thalassemia with gene therapy, patients must receive conditioning treatments like chemotherapy to make space for the new, corrected blood cells, which is both expensive and comes with risks,” says co-senior author Stefano Rivella, Kwame Ohene-Frempong Chair on Sickle Cell Anemia and Professor of Pediatrics at CHOP. “In our paper, we have shown that it is possible to replace diseased blood cells with corrected ones directly within the body in a ‘one-and-done’ therapy, eliminating the need for myeloablative conditioning treatments and streamlining the delivery of these potentially life-changing treatments. This is a big step forward in how we think about treating genetic diseases and could expand the access of gene therapies to patients who need them most.”
Read more at Penn Medicine News.