Infection
Biomarkers distinguish pediatric musculoskeletal infections from similar conditions
1. In a prospective cohort study, white blood cell (WBC) count, absolute neutrophil count (ANC), C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), and procalcitonin (PCT) were elevated in pediatric patients with a musculoskeletal infection.
2. WBC count, ANC, CRP, ESR, and PCT were distinguished musculoskeletal infections from Lyme arthritis and other types of inflammatory arthritis.
Evidence Rating Level: 2 (Good)
Study Rundown: Bacterial musculoskeletal infections (MSKI) are serious conditions that require rapid recognition and treatment. Distinguishing between bacterial MSKIs and similar joint disorders may require inaccessible or invasive diagnostic measures. This prospective cohort study of 1423 children sought to examine whether several biomarkers can be used to differentiate a MSKI from Lyme arthritis and other forms of inflammatory arthritis. White blood cell count (WBC), absolute neutrophil count (ANC), C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), and procalcitonin (PCT) were assessed in children with mono-arthritis. 82 of these patients had a MSKI; 25 had septic arthritis alone, 44 had osteomyelitis alone, 5 had both septic arthritis and osteomyelitis, and 3 had osteomyelitis and pyomyositis. 405 patients had Lyme arthritis and 936 had other inflammatory arthritis. Receiver operating characteristics (ROC) curves were generated for each biomarker to determine their test performance through area under the curve (AUC) comparison to the AUC for WBC count, since this is a validated component of MSKI clinical decision-making rules. Each of the assessed biomarkers was significantly elevated in patients with bacterial MSKI compared to patients without a bacterial MSKI, although interquartile ranges overlapped for WBC, ANC, ESR, and PCT. ROC analysis was conducted to determine optimal cut-points for each biomarker. PCT was 98.6% specific for MSKI at the literature cut-point, while ANC was 93.2% specific at the literature cut-point. The other biomarkers had varying specificities and sensitivities at the cut-points. This study suggests that even in Lyme-endemic regions, the tested biomarkers may distinguish between bacterial MSKI and non-bacterial MSKI. Due to the varying accuracy in each individual biomarker, including multiple biomarkers in clinical decision-making is advised.
Click to read the study in Pediatrics
Relevant Reading: Serum procalcitonin is a sensitive and specific marker in the diagnosis of septic arthritis and acute osteomyelitis
In-Depth [prospective cohort]: Blood samples from 1423 children with mono-arthritis across 8 hospitals in Lyme-endemic areas were obtained and analyzed for WBC count, ANC, CRP, ESR, and PCT levels. 907 (63.7%) of patients were male. 82 (5.8%) of patients had a MSKI, 405 (28.5%) had Lyme arthritis, and 936 (65.8%) had other inflammatory arthritis. The difference between each biomarker in the MSKI and non-MSKI groups were computed. For WBC, the difference was 1.8 (95% CI 0.5-3.1) k cells/μL. For ANC the difference was 2.4 (95% CI 1.3-3.6) k cells/μL, 4.40 (95% CI 3.43-5.37) mg/dl, and 28 (95% CI 23-33) mm/h for CRP and ESR respectively. The difference for PCT was 0.13 (0.05-0.21) ng/dl, with all differences having statistical significance. Using the AUC data generated from the ROC curves, biomarker test performance was assessed, with cut-points empirically derived from the experimental model, and from the existing literature. Empirically derived cut points were often lower than literature cut points. At the literature cut point of 0.50 ng/mL, PCT had a 98.6% specificity and positive likelihood ratio of 18.0 (95% CI 8.6-37.4). ANC had a 93.2% specificity at the literature cut point of 10.0 k cells/μL, translating to a positive likelihood ratio of 4.3 (95% CI 2.9-6.4). CRP had a specificity of 72.3% at the literature cut point of 2.00 mg/dL, translating to a positive likelihood ratio of 3.0 (95% CI 2.6-3.4). CRP also had the highest sensitivity at 82.5%. Negative likelihood ratios were relatively similar for all biomarkers, despite profound differences in sensitivity.
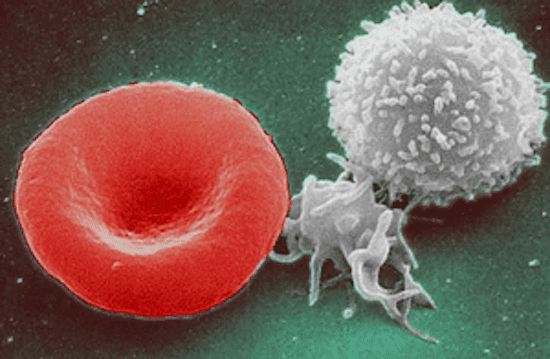
Image: PD
©2023 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.