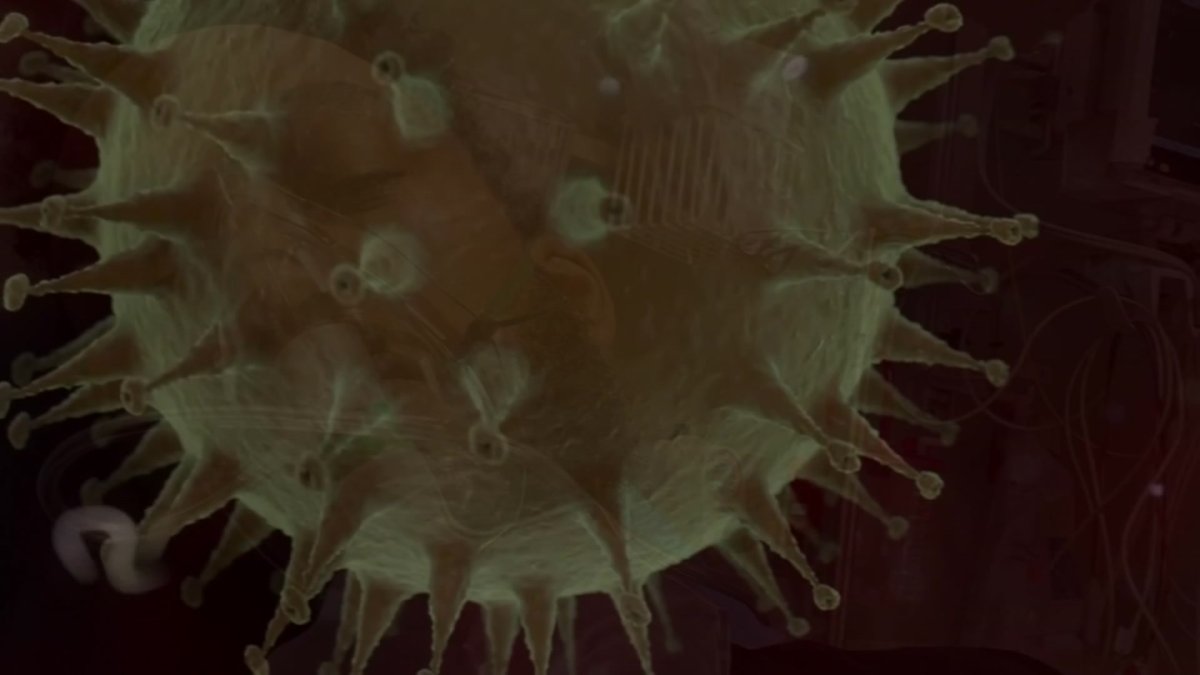
Infection
Here are what symptoms to watch for as EG.5, the new dominant COVID variant, spreads
Following a rise in COVID cases and hospitalizations across the country this summer, as well as a “mini-surge” in the Chicago area, questions have surfaced about what precipitated the uptick and whether it can be traced to a specific variant.
The EG.5 omicron subvariant, also commonly known as Eris, accounted for the largest number of U.S. COVID infections compared to any other strain, according to the latest data from the Centers for Disease Control and Prevention. From a nearly two-week period beginning on July 23 and ending on Aug. 5, EG.5 was responsible for more than 17% of all U.S. COVID cases, a jump of 5% compared to two weeks earlier.
In response to a rise in cases globally, the World Health Organization on Wednesday classified EG.5 as a variant of interest. A descendant of the XBB sublineage XBB.1.9.2, EG.5 has one additional spike mutation, allowing to evade immunity easier than others.
While first detected in February 2023, the WHO added EG. 5 to its list of variants under monitoring on July 19.
When it comes to symptoms, they appear to largely mirror those experienced with other COVID infections.
“EG.5 has been detected in the U.S. recently, but the data we have gleaned from the global circulation of the virus has shown that its symptoms are the same as other variants,” Andrew Pekosz, a professor in Molecular Microbiology and Immunology with the John Hopkins Bloomberg School of Public Health, said in an article. “Its disease potential appears to be exactly the same as other variants’ as well.”
People who contract COVID may exhibit a wide range of symptoms, including the common ones listed below, as defined by the CDC:
In an email to NBC Chicago on Thursday, a CDC spokesperson said guidance and information on the agency’s website hadn’t changed — despite the emergence of new strains.
When compared to other XBB variants, EG.5 is likely more transmissible, Dr. Sharon Nachman, chief of the division of pediatric infectious diseases at Stony Brook Children’s Hospital, told TODAY.com. However, it’s unclear why that is the case.
“”If it was equally transmissible, then we wouldn’t see it gaining strength number-wise compared to some of the other variants,” said Nachman, adding that EG.5 quickly pushed out other XBB variants in the U.S., which were dominant earlier this summer.
EG.5 has shown increased prevalence, growth and immune escape properties, but it doesn’t appear to be more severe than others, as stated in a recent WHO report.
“It’s been quite a long time since boosters were provided for COVID, and those boosters did have a relatively low uptake rate in the population,” Pekosz said. “That, combined with the fact that the XBB variants look different to your immune system from the [variants used in] previous COVID vaccines.”
But if you’re due for a COVID shot, you might want to consider getting the new booster once it rolls out in the fall.
While the booster won’t be specifically designed to target EG.5, the basis for the new vaccine will be the XBB variants, which are closely associated to EG.5.
“There should be a nice match between that vaccine and the EG.5 variant, as well as the other XBB variants that are circulating right now,” Pekosz said.