Cardiovascular
Decision support tools do not reduce disparities in cardiovascular care
August 11, 2023
2 min read
Source/Disclosures
Disclosures:
Roberts reports no relevant financial disclosures. Please see the study for all other authors’ relevant financial disclosures.
Key takeaways:
- BP control and cholesterol management metrics were higher for white patients compared with those for Black patients.
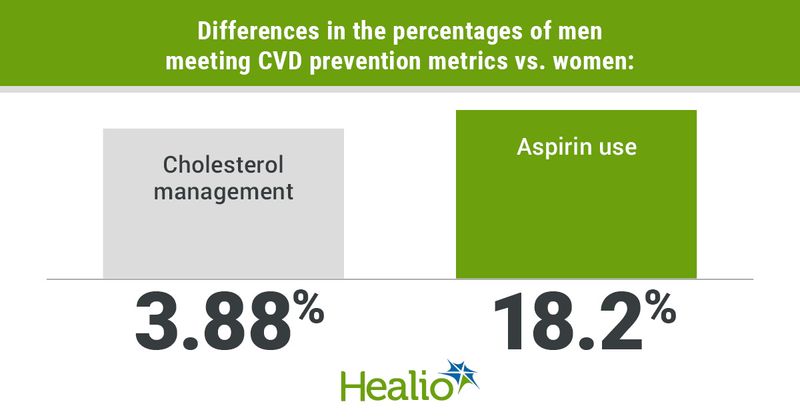
- In addition, cholesterol management and aspirin use were higher in men vs. women.
Clinical decision support tools were not associated with reductions in racial, ethnic and gender disparities in CVD prevention metrics among primary care practices, according to researchers.
“Electronic health record (EHR) prompts, standing orders, and clinical registries are clinical decision support (CDS) tools, which typically function as strategies to improve patient outcomes,” Madeline R. Roberts, PhD, MPH, research director at The Epidemiology Monitor, and colleagues wrote in JAMA Network Open. “Less is known about their effect on disparities in delivering guideline-concordant care within primary care.”
Data derived from: Roberts M, et al. JAMA Netw Open. 2023;doi:10.1001/jamanetworkopen.2023.26905.
They added that research is needed “to clarify whether use of CDS tools reduces disparities in care delivery among smaller independent practices, which provide most primary care nationally.”
“These clinics often lack resources to implement evidence-based practices,” they wrote.
The researchers hypothesized that the CDS tools, being automated and evidence based, would be associated with race, ethnic and gender disparity reductions in the “ABCS” quality metrics for CVD secondary prevention and management:
- aspirin use for at-risk individuals aged 40 to 49 years;
- BP control for hypertension;
- cholesterol management; and
- smoking cessation counseling.
To prove their theory, Roberts and colleagues used 2015 to 2016 survey- and EHR-based data from EvidenceNOW, an Agency for Healthcare Research and Quality-funded initiative directed at improving cardiovascular preventive care in small primary care practices.
With these data, the researchers evaluated practice-level estimates of disparities between Black and white patients and between male and female patients for each of the four quality metrics.
Overall, the analysis included data from 576 primary care practices. Among them, 26% had one clinician and 50.3% were clinician owned.
Roberts and colleagues found that BP control (difference = 5.16%; 95% CI,4.29-6.02) and cholesterol management (difference =1.49%; 95% CI,0.04-2.93) metrics were higher for white patients compared with those for Black patients.
In addition, metrics for cholesterol management (difference = 3.88%; 95% CI,3.14-4.63) and aspirin use (difference = 4.36%; 95% CI,3.34-5.38) were also higher for men compared with those for women. However, BP control (difference = –1.8%; 95% CI,–2.32 to –1.28) and smoking cessation counseling (difference = –1.67%; 95% CI,–2.38 to –0.95) metrics were higher for women compared with those for men.
The researchers noted that practices using CDS tools had small and insignificant disparities, but the tools did not reduce disparities in any metrics except for smoking counseling.
“The CDS tools have received little attention for their potential to reduce disparities among smaller primary care practices where most U.S. health care happens,” they wrote. “Our hypothesis was not supported, possibly because having registries or prompts may not equate with consistent use, or because even if a practice uses CDS tools, Black patients may have additional access barriers to care.”
The study was limited because of the lack of individual patient information like comorbidities, patient risk levels and social determinants of health, according to the researchers. Additionally, Roberts and colleagues were unable to determine how practices used the CDS tools.
Although the researchers pointed out that CDS implementation may increase appointment times and cognitive loads for physicians; however, “customizing prompts can improve clinician experience.”
“The quadruple aim includes clinician well-being, necessitating CDS implementation that supports rather than encumbers clinicians; evidence shows this is possible,” they wrote.