Cardiovascular
Long-Term Adverse Cardiovascular Events in STEMI Patients
Introduction
Cardiovascular diseases are the leading cause of death worldwide, with ischemic heart disease being the most common type.1 ST-segment elevation myocardial infarction (STEMI) is the most serious manifestation of ischemic heart disease. Based on the national registries of the European Society of Cardiology) countries, the incidence rate of STEMI in other European countries ranged from 43 to 144 per 100000 per year in 2015, and in-hospital mortality rates for patients with STEMI varied between 4% and 12%, while the 1-year mortality among patients with STEMI in angiography registries was approximately 10%.2 Reducing the high morbidity and mortality of STEMI and improving patient prognosis remains a major global challenge.2,3 The age of onset of STEMI has progressively decreased and it is crucial to reduce the economic burden of the disease and improve the quality of life and prognosis of patients through early and accurate diagnosis, rapid and effective treatment, and accurate prediction of prognosis.4 Accurate identification of the clinical features of patients with STEMI with adverse cardiovascular events after hospital discharge may contribute to the screening of high-risk patients, development of individualized treatments, optimization of post-discharge management, and improvement in clinical prognosis.5
Previous studies have shown that the immunoinflammatory response plays an important role in the pathogenesis of myocardial infarction (MI) and is also closely related to clinical prognosis.6–9 Serum inflammatory markers such as lymphocytes, neutrophils, monocytes, and platelets, infiltrate atherosclerotic lesions and initiate cytokine cascade reactions leading to the onset and progression of coronary lesions.10,11 Blood tests, including lymphocyte, neutrophil, monocyte, and platelet counts, are economical and rapid tests for routine use in clinical practice. A growing number of studies have confirmed that serum immune-inflammatory markers, including the systemic immune-inflammation index (SII), systemic inflammatory response index (SIRI), and pan-immune-inflammation-value (PIV), have good predictive value for long-term adverse cardiovascular events after percutaneous coronary intervention (PCI) in patients with acute coronary syndrome or STEMI.12–14 However, previous studies focused only on the predictive efficacy of the single value of these markers on emergency admission rather than the dynamic fluctuations of these markers at or between different time points.
This study investigated whether repeated measurements of SII, SIRI, and PIV serum markers calculated at different time points, as well as dynamic fluctuations of these markers over time, aided the accurate identification of major adverse cardiovascular events (MACEs) after hospital discharge in high-risk patients with STEMI. We also explored the incremental value of repeated serum marker measurements compared to a single measurement on emergency admission for the improvement of long-term prognosis, optimization of post-discharge management, improvement of quality of life, and increase in life expectancy of patients with STEMI.
Materials and Methods
Study Design and Patients
This retrospective study examined the data of patients admitted with chest discomfort or other symptoms of myocardial ischemia to the emergency department of No. 904 Hospital of Joint Logistics Support Force of People’s Liberation Army of China between January 2016 and January 2020. The patients were divided into a STEMI group (n = 524) who underwent successful emergency primary PCI in the emergency department and a control group (n = 138) that underwent elective coronary artery angiography (CAG) examination in the cardiovascular department of the hospital excluding acute myocardial infarction (AMI). These patients were defined as non-AMI.
STEMI was diagnosed according to the fourth universal definition of MI (2018).15 The inclusion criteria were as follows: (1) typical symptoms of chest pain lasting more than 10 min; (2) changes on electrocardiography (ECG) during emergency admission consisting of ≥ 1 mm ST-segment elevation in ≥ 2 contiguous leads or in leads V2-V3 (≥ 1.5 mm in women, ≥ 2.5 mm in men < 40 years old, ≥ 2 mm in men < 40 years old) without bundle branch block or left ventricular hypertrophy; and (3) repeat ECG within a short period from admission in patients without the above ECG changes during the emergency admission, to reduce the rate of missed STEMI.
The following exclusion criteria for patients with STEMI applied: (1) pain-to-balloon (P2B) interval > 12 h; (2) absence of clinical data (routine blood tests and baseline data on emergency admission); (3) loss to follow-up within 1 year after discharge; (4) previous history of coronary artery stenting or bypass grafting for MI; (5) history of coronary stenting for unstable angina; (6) combined renal insufficiency, hematologic disorders, malignancy, and chronic or acute inflammatory diseases; and (7) death during hospitalization.
The exclusion criteria for non-AMI patients were as follows: (1) absence of clinical data; (2) previous history of coronary artery stenting or bypass grafting for MI; (3) history of coronary stenting for unstable angina; and (4) combined renal insufficiency, hematologic disorders, malignancy, and various chronic or acute inflammatory diseases.
The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of No. 904 Hospital of Joint Logistics Support Force of the People’s Liberation Army of China, which waived the requirement for informed consent due to the retrospective nature of the study.
Data Collection
Patient demographic characteristics, clinical information (age, sex, history of hypertension, history of diabetes, history of smoking, body mass index, Killip classification on admission, P2B duration, and hospitalization duration); post-discharge medications (beta-receptor blockers, angiotensin-converting enzyme inhibitors/angiotensin-receptor blockers, and calcium channel blockers); indicators of myocardial injury (peak creatine kinase-MB and peak troponin I [TnI]); blood biochemical indicators (hemoglobin, albumin, total cholesterol, triglycerides, high-density lipoprotein cholesterol, low-density lipoprotein cholesterol, C-reactive protein [CRP], lipoprotein a, serum uric acid, and serum creatinine); indicators of coagulation system function (fibrinogen and d-dimer); and routine blood indicators (neutrophil, monocyte, lymphocyte, and platelet counts) were collected by a cardiovascular physician who was blinded to the above information.
Patients with STEMI were transferred to the intensive care unit after emergency primary PCI. Bedside Doppler echocardiography was performed within 48 h, and the left ventricular ejection fraction (LVEF) and left ventricular end-diastolic diameter were recorded for each patient. Peripheral vascular artery ultrasonography was performed before discharge, and the presence of carotid artery calcification was recorded.
All patients with STEMI were treated with oral aspirin enteric-coated tablets (300 mg) and ticagrelor (180 mg) before PCI. The emergency primary PCI was performed by two surgeons who were qualified to perform cardiovascular intervention. The following information was recorded: CAG-related parameters such as the number of diseased vessels (coronary stenosis ≥ 50%),16 site of MI (left main stem, left anterior descending, left circumflex branch, right coronary artery), stent length and internal diameter, and coronary flow in the infarcted coronary artery after emergency primary PCI (no-reflow group: thrombolysis in Myocardial Infarction [TIMI] grade ≤ 2; normal-flow group: TIMI grade 3 after percutaneous transluminal coronary angioplasty or stent implantation),17 and severity of coronary artery diseases evaluated by the Gensini score.18 Any disagreement between the two surgeons over these assessments was resolved by discussion with a third surgeon specializing in cardiovascular intervention. Long-term antiplatelet therapy with aspirin enteric tablets and ticagrelor was prescribed for all patients with STEMI without any contraindications at discharge.
SII, SIRI, and PIV were calculated at four time points: (1) T1, at emergency admission; (2) T2: 6–12 h after emergency primary PCI (median time, 12 [IQR, 10–12] hours); (3) T3: 12–48 h after PCI (median time, 22 [IQR, 20–36] hours); and (4) T4, at discharge. SII was calculated as follows: (neutrophil count [109/L] × platelet count [109/L]/lymphocyte count [109/L]). SIRI was calculated as follows: (neutrophil count [109/L] × monocyte count [109/L]/lymphocyte count [109/L]). PIV was calculated as: (neutrophil count [109/L] × platelet count [109/L] × monocyte count [109/L]/lymphocyte count [109/L]).
Definition and Follow-Up of Major Adverse Cardiovascular Events
For patients with STEMI who underwent emergency primary PCI, MACEs that occurred within 1 year after discharge, including all-cause death, recurrent MI, stent reimplantation for unstable angina, and heart failure, were recorded. Post-discharge follow-up data were collected by reviewing the inpatient and outpatient electronic records. For patients with STEMI who did not return to our hospital within 1 year after discharge, endpoint events were obtained by contacting the patients or their immediate family members by telephone.
Statistical Analysis
The statistical analysis was performed using SPSS (version 26.0; SPSS Inc., Chicago, IL, USA), GraphPad Prism 9, and MedCalc. The normality of the data was examined using Kolmogorov–Smirnov test (sample size ≥ 50) and Shapiro–Wilk test (sample size < 50). Normally distributed continuous variables are expressed as mean ± standard deviation, and Student’s t-test was used to compare intergroup differences. Skewed continuous variables are expressed as median (interquartile [IQR]), while the Mann–Whitney U-test was used to compare intergroup differences. Categorical variables are expressed as frequency (percentage), while the chi-squared test or Fisher’s exact test was used to compare intergroup differences. Repeated-measures analysis of variance or Friedman test was used to compare multiple (n ≥ 3) measurements of the same indicator. Post-hoc tests were used to compare groups, and adjusted P values were recorded using the Bonferroni method. Univariate Cox regression analysis was used to determine the risk factors for MACEs after emergency primary PCI in patients with STEMI; variables with values of P < 0.05 were included in the multivariate Cox regression analysis model using the forward likelihood ratio method considering the potential collinearity between SII, SIRI, and PIV as well as their dynamic fluctuations at different time points. Spearman correlation analysis was used to assess correlations between the variables. The receiver operating characteristic (ROC) curve was used to evaluate the SII, SIRI, and PIV values as well as their dynamic fluctuations at different time points in predicting the prognosis of patients with STEMI after emergency primary PCI. The optimal threshold, sensitivity, specificity, hazard ratio (HR), and 95% confidence interval (CI) were calculated. De–Long test was used to compare the difference in predictive efficacy. The patients were divided into two groups based on the optimal thresholds of SII, SIRI, PIV, and their dynamic fluctuations at different time points. The Kaplan–Meier method was used to compare the non-MACE survival rates between groups, and survival curves were plotted. All comparisons were two-tailed and P-value < 0.05 was considered statistically significant.
Results
Basic Information on STEMI versus Control Group
Based on the inclusion and exclusion criteria, 468 patients with STEMI and 122 patients with non-AMI were included in this study. A flow diagram depicts the experimental plan (Figure 1). In the STEMI group, routine blood test results at four time points (T1–T4) were available for 42 patients (32 men, 10 women; median age, 63 [IQR, 55–69] years), while routine blood test results at three time points (T1, T2, T4) were available for 216 patients (181 men, 35 women; mean age, 63 [IQR, 51–69] years). The control group included 70 men and 52 women with a median age of 59 (IQR, 52–67) years. The comparison of clinical data between the control group and the STEMI group (n = 42) is shown in Table 1.
|
Table 1 Comparison of Baseline Characteristics and Laboratory Parameters Between Patients with Non Acute Myocardial Infarction Patients (Non-AMI) and ST-Segment Elevation Myocardial Infarction (STEMI) at Admission |
 |
Figure 1 Study flow chart. 468 patients were diagnosed with ST-segment elevation acute myocardial infarction on admission. (A). 42 patients who also had routine blood tests on admission, 6–12 h after PCI, 24–48 h after PCI, and at discharge were screened; (B). A total of 216 patients with both routine blood tests on admission, 12 h after PCI, and at discharge were screened. Abbreviation: PCI, percutaneous coronary intervention. |
Dynamic Fluctuations of Total White Blood Cell Counts in the STEMI Group
For the 42 patients with STEMI who underwent routine blood tests at four time points, the dynamic fluctuations of total blood cell counts were analyzed. As shown in Figure 2, the neutrophil count peaked at T2, the monocyte count peaked at T3, the platelet count peaked at T2, and the lowest lymphocyte count was recorded at T2.
 |
Figure 2 Trajectory of dynamic change in white blood cell count from admission to discharge in patients with ST-segment elevation acute myocardial infarction. (A). Trajectories of white blood cell counts in 42 patients with ST-segment elevation myocardial infarction during admission, 6–12 hours after PCI, 24–48 hours after PCI, and at discharge; (B). Trajectories of white blood cell counts in 216 patients with ST-segment elevation myocardial infarction during admission, 12 hours after PCI, and at discharge. (N, number of patients with white blood cells determinations; #Mean ± SD; *Median (interquartile range)). Abbreviation: PCI, percutaneous coronary intervention. |
Serum Inflammatory Indicators of STEMI versus Control Groups at Four Time Points
The dynamic fluctuations of serum inflammatory indicators for the 42 patients with STEMI who underwent routine blood tests at four time points are shown in Table 2 and Figure 3. The SII values at T1 were significantly higher in patients with STEMI than in those of the control group on admission (P < 0.001); these were also significantly higher in patients with STEMI at T2 than at T1 (P = 0.006), T3 (P < 0.001), and T4 (P < 0.001). In addition, SIRI values were significantly higher in patients with STEMI at T1 than in those of the control group on admission (P < 0.001); these were also significantly higher in patients with STEMI at T2 than at T1 (P = 0.002), T3 (P = 0.003), and T4 (P < 0.001). The PIV was significantly higher in STEMI patients at T1 than in those of the control group on admission (P < 0.001); it was also significantly higher in STEMI patients at T2 than at T1 (P = 0.001), T3 (P = 0.032), and T4 (P < 0.001). Based on the above, it could be inferred that serum inflammatory indicators (SII, SIRI, and PIV) were higher in patients with STEMI at T1 than in controls on admission and peaked at T2 in patients with STEMI.
 |
Table 2 Dynamic Trajectories of SII, SIRI, and PIV from Admission to Discharge in Patients with STEMI |
|
Figure 3 Trajectory of the dynamic changes of inflammatory markers SII, SIRI, and PIV from admission to discharge in patients with ST-segment elevation myocardial infarction. Trajectory of SII (A), SIRI (B), and PIV (C) dynamics in 42 patients with ST-segment elevation myocardial infarction (Mann–Whitney U-test P < 0.05, Friedman test and Bonferroni post hoc test adjusted P < 0.05). Box-and-whisker plot showing dynamic change trends for SII (D), SIRI (E), and PIV(F) in 216 patients with ST-segment elevation myocardial infarction (Friedman test and Bonferroni post hoc test adjusted P < 0.05). Boxes indicate 25–75% interquartile range; horizontal lines in boxes, median width; whiskers, 10–90% range; dots, detected outliers that reside outside the whisker range. Bolded values indicate higher levels of inflammatory markers SII, SIRI, and PIV in patients with STEMI at admission compared to the non acute myocardial infarction (control group). In patients with STEMI, the expression levels of inflammatory markers SII, SIRI, and PIV were higher 6–12 or 12 hours after PCI compared to admission and discharge. Abbreviations: SII, systemic immune-inflammation index; SIRI, systemic inflammation response index; PIV, pan-immune-inflammation value, PCI, percutaneous coronary intervention. |
Serum Inflammatory Indicators Profiles at Three Time Points in Patients with STEMI
For the 216 patients who underwent routine blood tests at the three time points, the median timing for routine blood tests at T2 was 12 h after emergency primary PCI. Therefore, the dynamic fluctuations in serum inflammatory indicators in patients with STEMI at different time points after admission were further validated (Figure 2, Table 2, and Figure 3). The SII values at T2 in patients with STEMI were higher than those at T1 (P < 0.001) and T4 (P < 0.001). In addition, the SIRI values at T2 in patients with STEMI were higher than those at T1 (P < 0.001) and T4 (P < 0.001). The PIV in patients with STEMI was higher at T2 than at T1 (P < 0.001) and T4 (P < 0.001).
MACEs Among STEMI Patients
The long-term follow-up of the 216 patients with STEMI after discharge identified a total of 85 (39.35%) patients with MACEs within 1 year after discharge, including 14 (16.47%) with all-cause mortality, 18 (21.18%) with acute recurrence of MI, 27 (31.76%) with stent reimplantation for unstable angina, 21 (24.71%) with heart failure, 2 (2.35%) with acute MI combined with heart failure, and 3 (3.53%) with stent reimplantation for unstable angina combined with heart failure (Table 3).
 |
Table 3 Clinical Outcomes at 1-Year Follow-Up After PCI for ST-Segment Elevation Myocardial Infarction (STEMI) |
Clinical Information of MACE versus Non-MACE Groups
We further explored the value of serum inflammatory markers (SII, SIRI, and PIV) measured at different time points and dynamic marker fluctuations between the time points for predicting the prognosis of patients with STEMI.
The 216 patients with STEMI were divided into MACE and non-MACE groups based on the occurrence of MACEs within 1 year of discharge. The clinical information of the MACE and non-MACE groups, including clinical characteristics, medication history, laboratory test and examination results, CAG-related parameters, serum inflammatory indicator values, and dynamic fluctuations in these values at different time points, are presented in Table 4 and Figure 4.
|
Table 4 Basic Clinical Characteristics Between MACEs Groups and Non-MACEs Groups in Patients with STEMI |
|
Figure 4 Differential values of the inflammatory markers SII, SIRI, and PIV between the major cardiovascular adverse events (MACEs) and non-MACEs groups at different time points and between different time points (Mann–Whitney U-test P < 0.05). (A). Differential values of SII between MACEs and non-MACEs groups; (B). Differential values of SIRI between MACEs and non-MACEs groups; (C). Differential values of PIV between MACEs and non-MACEs groups; (D). Differential values of SII changes between MACEs and non-MACEs groups; (E). Differential values of SIRI changes between MACEs and non-MACEs groups; (F). Differential values of PIV changes between MACEs and non-MACEs groups. Abbreviations: SII, systemic immune-inflammation index; SIRI, systemic inflammation response index; PIV, pan-immune-inflammation value. |
A higher percentage of patients with a Killip class ≥ II on admission, ≥ 2 diseased vessels, and no-reflow as well as a longer hospitalization duration was detected in the MACE than in the non-MACE group. In addition, the following parameters were higher in patients in the MACE than in those in the non-MACE group: peak TnI, CRP, fibronectin, d-dimer, and lipoprotein a levels; stent length; Gensini score; SII, SIRI, and PIV values at T1, T2, and T4; and dynamic fluctuations of SIRI and PIV serum levels between T2 and T1. However, the LVEF and the fluctuations of SII, SIRI, and PIV between T4 and T2 were lower for patients in the MACE than for those in the non-MACE group.
Results of Univariable and Multivariable Cox Regression
Variables with values of P < 0.05 in the comparison of the MACE and non-MACE groups were included in the univariable Cox regression analysis. After the adjustment for confounders, the multivariable Cox regression analysis revealed that a Killip class ≥ II on admission (HR, 1.859; 95% CI, 1.169–2.957; P = 0.009), total stent length (HR, 1.016; 95% CI, 1.003–1.029; P = 0.019), SIRI values at T2 (HR, 1.079; 95% CI, 1.050–1.108; P < 0.001), and the Gensini score (HR, 1.014; 95% CI, 1.007–1.022; P < 0.001) were independent risk factors for poor long-term prognosis in patients with STEMI after PCI (Table 5).
|
Table 5 Univariate and Multivariable Cox Proportional Hazard Regression Analysis of MACEs Occurrence Within 1 Year of Hospital Discharge in Patients with ST-Segment Elevation Myocardial Infarction (STEMI) After PCI |
Correlation Between Serum Inflammatory Indicators Values and Clinical Information
Correlation analysis showed that SIRI values at T2 were positively correlated with the Gensini score (r = 0.206, P = 0.002). SIRI values at T2 were negatively correlated with LVEF (r = −0.274, P < 0.001). SIRI values at T2 were significantly higher in patients with STEMI with a Killip class ≥ II than in those with Killip class I (P = 0.002); these were also significantly higher in patients with STEMI with no-reflow after PCI than in those with normal blood flow after PCI (P < 0.001) (Table 6).
|
Table 6 Correlation Between General Clinical Characteristics, Angiographic Characteristics and SIRI in Patients with ST-Segment Elevation Myocardial Infarction (STEMI) |
Assessment of Predictive Efficacy of Serum Inflammatory Indicators Using ROC Curve
As shown in Table 7, in patients with STEMI, the predictive value of SII at T2 (area under the curve [AUC], 0.678; 95% CI, 0.611–0.739) for poor long-term prognosis after PCI was not significantly different from that at T1 (AUC, 0.627; 95% CI, 0.559–0.692; P = 0.275) or T4 (AUC, 0.650; 95% CI, 0.583–0.714; P = 0.540). However, SII values in patients with STEMI at T2 were superior in predicting poor long-term prognosis than dynamic changes in SII values between T4 and T2 (AUC, 0.678; 95% CI, 0.611–0.739 vs AUC, 0.586; 95% CI, 0.517–0.652; P < 0.001).
|
Table 7 The Optimal Cut-off Value and Area Under the Receiver Operating Characteristic Curve (ROC) of Inflammatory Markers SII, SIRI and PIV and Their Dynamically Fluctuating Changes Between Each Time Point to Predict the Occurrence of Major Adverse Cardiac Events (MACEs) Within 1 Year of Discharge in Patients with ST-Segment Elevation Myocardial Infarction (STEMI) After PCI |
In patients with STEMI, SIRI values at T2 (AUC, 0.764; 95% CI, 0.701–0.819) were superior in predicting poor long-term prognosis than SIRI values at T1 (AUC, 0.647; 95% CI, 0.579–0.711; P = 0.007), T4 (AUC, 0.642; 95% CI, 0.574–0.706; P = 0.005) and dynamic changes in SIRI values between T2 and T1 (AUC, 0.667; 95% CI, 0.599–0.729; P = 0.002) and between T4 and T2 (AUC, 0.708; 95% CI, 0.643–0.768; P = 0.003). The best SIRI cutoff value at T2 for predicting long-term prognosis in patients with STEMI was 4.15 (95% CI, 0.701–0.819), with a sensitivity of 77.65% and a specificity of 62.60% (Figure 5).
 |
Figure 5 Receiver operating characteristic (ROC) curves. (A). ROC curve for SIRI at 12 hours after PCI to predict the major cardiovascular adverse events (MACEs); (B). ROC curve for PIV at 12 hours after PCI to predict the MACEs. Abbreviations: SIRI, systemic inflammation response index; PIV, pan-immune-inflammation value. |
The PIV calculated at T2 (AUC, 0.738; 95% CI, 0.674–0.796) was superior to the PIV calculated at T1 (AUC, 0.640; 95% CI, 0.573–0.704; P = 0.016), T4 (AUC, 0.642; 95% CI, 0.574–0.706; P = 0.024), and to dynamic PIV fluctuations between T2 and T1 (AUC, 0.670; 95% CI, 0.603–0.732; P = 0.032) and between T4 and T2 (AUC, 0.669; 95% CI, 0.602–0.731; P = 0.002) for predicting long-term poor prognosis in patients with STEMI. The cutoff value for PIV at T2 to predict long-term prognosis in patients with STEMI was 622.71 (95% CI, 0.674–0.796) for long-term prognosis, with a sensitivity of 84.71% and a specificity of 49.62% (Figure 5).
Further comparative analysis revealed that SIRI values at T2 (AUC, 0.764; 95% CI, 0.701–0.819]) were superior to SII values at T1 (AUC, 0.627; 95% CI, 0.559–0.692; P = 0.002), T2 (AUC, 0.678; 95% CI, 0.611–0.739; P = 0.003), and T4 (AUC, 0.650; 95% CI, 0.583–0.714; P = 0.014) for predicting long-term poor prognosis in patients with STEMI. The PIV at T2 (AUC, 0.738; 95% CI, 0.674–0.739) was superior to SII values at T1 (AUC, 0.627; 95% CI, 0.559–0.692; P = 0.010), T2 (AUC, 0.678; 95% CI, 0.611–0.739; P = 0.005), and T4 (AUC, 0.650; 95% CI, 0.583–0.714; P = 0.043) in predicting poor long-term prognosis in patients with STEMI. SIRI and PIV at T2 did not have significantly different ability to predict poor long-term prognosis in patients with STEMI (AUC, 0.764; 95% CI, 0.701–0.819 vs AUC, 0.738; 95% CI, 0.674–0.796; P = 0.157).
Kaplan–Meier survival analysis of STEMI patients
The Kaplan–Meier survival analysis showed that patients with STEMI with a SIRI value < 4.15 at T2 had greater long-term event-free survival after PCI than those with a SIRI value ≥ 4.15 at T2 (log-rank, P < 0.001; Figure 6). Patients with STEMI with a PIV < 622.71 at T2 had greater long-term event-free survival after PCI than those with a PIV ≥ 622.71 at T2 (log-rank, P < 0.001; Figure 6). Patients with STEMI with a SIRI value < 4.15 at T2 had a lower long-term mortality rate (log-rank, P = 0.027; Figure 7A), incidence of MI (log-rank, P = 0.003; Figure 7B), incidence of heart failure (log-rank, P < 0.001; Figure 7C), and incidence of stent reimplantation for unstable angina (log-rank, P < 0.012; Figure 7D) than those with a SIRI value ≥ 4.15 at T2. In addition, patients with STEMI with a PIV < 622.71 at T2 had a lower long-term mortality rate (log-rank, P = 0.012; Figure 7E), incidence of MI (log-rank, P = 0.004; Figure 7F), incidence of heart failure (log-rank, P < 0.019; Figure 7G), and incidence of stent reimplantation for unstable angina (log-rank, P < 0.016; Figure 7H) than those with a PIV ≥ 622.71 at T2.
 |
Figure 6 Kaplan–Meier survival analysis. (A). Patients with a high SIRI value (SIRI ≥ 4.15) had a much lower event-free survival at long-term follow-up than patients with a low SIRI value (SIRI < 4.15); (B). Patients with a high PIV (PIV ≥ 622.71) had a much lower event-free survival at long-term follow-up than patients with a low PIV (PIV < 622.71). Abbreviations: SIRI, systemic inflammation response index; PIV, pan-immune-inflammation value. |
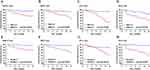 |
Figure 7 Kaplan–Meier survival analysis. (A). Patients with a high SIRI value (SIRI ≥ 4.15) had a much higher mortality rate at long-term follow-up than patients with a low SIRI value (SIRI < 4.15); (B). Patients with a high SIRI value (SIRI ≥ 4.15) had a much higher new-onset nonfatal acute myocardial infarction (AMI) rate at long-term follow-up than patients with a low SIRI value (SIRI < 4.15); (C). Patients with a high SIRI value (SIRI ≥ 4.15) had a much higher congestive heart failure (HF) rate at long-term follow-up than patients with a low SIRI value (SIRI < 4.15); (D). Patients with a high SIRI value (SIRI ≥ 4.15) had a much higher revascularization in unstable angina (UA) rate at long-term follow-up than patients with a low SIRI value (SIRI < 4.15); (E). Patients with a high PIV (PIV ≥ 622.71) had a much higher mortality rate at long-term follow-up than patients with a low PIV (PIV < 622.71); (F). Patients with a high PIV (PIV ≥ 622.71) had a much higher new-onset nonfatal acute myocardial infarction (AMI) rate at long-term follow-up than patients with a low PIV (PIV < 622.71); (G). Patients with a high PIV (PIV ≥ 622.71) had a much higher congestive heart failure (HF) rate at long-term follow-up than patients with a low PIV (PIV < 622.71); (H). Patients with a high PIV (PIV ≥ 622.71) had much a higher revascularization in unstable angina (UA) rate at long-term follow-up than patients with a low PIV (PIV < 622.71). Abbreviations: SIRI, systemic inflammation response index; PIV, pan-immune-inflammation value. |
Discussion
In the current study, we analyzed dynamic fluctuations in the total white blood cell count by reviewing the results of routine blood tests at four time points (on emergency admission, at 6–12 h after emergency primary PCI, at 12–48 h after PCI, and at discharge). Consistent with the results of Núñez et al, we found that serum neutrophils peaked at 12–24 h after PCI, while the serum lymphocyte count troughed within 12–24 h after PCI in patients with STEMI.19 Accordingly, our study concluded that the serum monocyte count peaked within 24–48 h after admission. Furthermore, the platelet count peaked at admission or 6–12 h after PCI in patients with STEMI, and platelet count fluctuation was smoother than fluctuations in neutrophil, monocyte, and lymphocyte counts throughout hospitalization. Serum inflammatory markers (SII, SIRI, and PIV) were compared at the four time points. The results showed that levels peaked at 6–12 h after PCI. This was further verified in another group of patients with STEMI by measuring SII, SIRI, and PIV values at three time points (on emergency admission, 12 h after PCI, and at discharge).
SII, SIRI, and PIV values at three time points and their dynamic fluctuations between time points for predicting the poor long-term prognosis of patients with STEMI, including acute MI, stent reimplantation for unstable angina, heart failure, and death, were then investigated. The predictive efficacy of SIRI and PIV at 12 h after PCI for adverse long-term prognosis of patients with STEMI was demonstrated with cutoff values of 0.764 and 0.738, respectively. To the best of our knowledge, this study comprehensively elucidated for the first time the effect of SII, SIRI, and PIV at different time points as well as their dynamic fluctuations between different time points on the long-term prognosis of patients with STEMI after PCI. Our results demonstrated that SIRI and PIV values at 12 h after PCI for predicting the poor long-term prognosis of patients with STEMI were superior to those on admission or discharge and dynamic fluctuations of these markers between time points. These findings provide a more convenient, cost-effective, and accurate approach to assessing the long-term prognosis of patients with STEMI as well as novel insights for the development of individualized management strategies in clinical practice for patients after discharge.
We also found that Killip class > II, total stent length, and the Gensini score on admission were independent risk factors for poor long-term prognosis after PCI in patients with STEMI, which was consistent with the results of previous studies.20 Accordingly, SIRI values at 12 h after PCI were demonstrated as a new independent predictor of poor long-term prognosis in patients with STEMI. The correlation analysis showed that SIRI values at 12 h after PCI in patients with STEMI were associated with the Gensini score, Killip class > II on admission, LVEF, and no-reflow after PCI. The Gensini score is a strong predictor of long-term adverse cardiovascular events in patients with STEMI after PCI. Coronary atherosclerosis underlies the development of coronary heart disease and MI. The development of coronary atherosclerosis is a sustained and dynamic inflammatory process of the vascular system.21 Our findings revealed that SIRI values at 12 h after PCI were positively correlated with the Gensini score, suggesting that these could influence long-term prognosis via coronary lesion severity. Killip class > II on admission was an independent risk factor for poor long-term prognosis, and the SIRI value at 12 h after PCI was positively correlated with Killip classification on admission, suggesting that it could influence the long-term prognosis of patients with STEMI via cardiac function status on emergency admission.
Previous studies have demonstrated that a reduced LVEF is an independent risk factor for poor long-term prognosis in patients with acute MI.22 SIRI values at 12 h after PCI were correlated with LVEF, indicating that these could influence the long-term prognosis of patients via reduced systolic and diastolic left ventricular function after MI. The occurrence of no-reflow after PCI in STEMI patients is highly correlated with reduced myocardial salvage and increased myocardial infarct size and is an independent risk factor for long-term MACEs such as malignant arrhythmia, heart failure, and death.23,24 SIRI levels at 12 h after PCI were associated with the occurrence of post-PCI no-reflow in this study, suggesting that these could influence patient long-term prognosis via myocardial infarct size. Based on the above, it could be inferred that SIRI values at 12 h after PCI were superior to those on admission and at discharge for predicting the long-term prognosis of patients with STEMI. This finding may be attributed to the fact that SIRI peaks more accurately reflect coronary lesion severity, cardiac function status on admission, myocardial contractility after MI, MI size, and degree of inflammation in patients with STEMI.
As a serum inflammatory indicator, SIRI is associated with various diseases such as cancer, stroke, and rheumatoid arthritis. Increased SIRI values may suggest poor long-term survival after surgery in patients with cancer as well as poor prognosis in patients with stroke.25–27 However, few studies have investigated the association between SIRI and cardiovascular diseases. In a 10-year follow-up study of 85,154 individuals, Jin et al confirmed that increased SIRI values were associated with higher all-cause mortality and incidence of acute MI in patients aged < 60 years.28 A single-center retrospective study by Ha confirmed that SIRI before PCI, as a continuous or categorical (tertiary) variable, was a strong independent predictor of MACEs (all-cause death, recurrence of non-fatal MI, non-fatal stroke, and unplanned revascularization) in 1724 patients with acute coronary syndromes after PCI.13 SIRI is a composite inflammatory indicator composed of neutrophil, monocyte, and lymphocyte counts, equivalent to the combination of neutrophil-lymphocyte ratio (NLR) and monocyte-to-lymphocyte ratio (MLR), making it more sensitive of and useful for reflecting immune inflammatory status. The roles of NLR and MLR as independent predictors of postoperative adverse cardiovascular events in patients with MI have been previously demonstrated.29,30 Serum inflammatory indicators (neutrophil, lymphocyte, and monocyte counts) were found to be independent predictors of long-term mortality in patients with acute MI.31 Neutrophils play a critical role in the rupture of atherogenic plaques, triggering acute coronary diseases.32 In patients with acute MI, the neutrophils can become activated and aggravate the inflammatory response at the site of coronary artery lesions, which are highly correlated with MI size.10 Dragu et al have reported that an elevated serum neutrophil count was associated with high mortality and could be used to predict poor prognosis in patients with acute MI.31
Lymphocytes are primarily involved in immune system regulation. Evidence suggests that, in patients with MI, a low serum lymphocyte count may indicate a systemic immune inflammation status in addition to playing a crucial role in accelerating coronary atherogenesis33 and is correlated with microvascular obstruction degree and MI size.34,35 Dragu et al have confirmed that a reduction in serum lymphocyte count is associated with poor long-term prognosis in patients with MI.31 In addition, monocytes are among the most important inflammatory indicators of the systemic inflammatory response. Previous studies have reported that, in the early stages of atherosclerosis, monocytes transform into macrophages, proliferate, and participate in the formation of the core of atheromatous plaques by phagocytosing oxidized low-density lipoprotein cholesterol.36 During acute MI onset, monocytes participate in atheromatous plaque rupture and the subsequent platelet aggregation, resulting in acute coronary events via the secretion of lytic enzymes (such as matrix metalloproteinases) to destabilize the fibrous cap.37 Monocytes are not only involved in the development and progression of coronary atherosclerosis but also serve as prognostic markers in patients with acute MI.38 Li et al have demonstrated that serum inflammatory indicators of NLR and MLR at and between time points in patients with ischemic stroke who were treated with intravenous tissue plasminogen activator peaked within 48 h after thrombolysis treatment; moreover, NLR and MLR had better predictive efficacy for poor prognosis within 48 h after thrombolysis treatment.39 Núñez et al have demonstrated for the first time that NLR peaked in patients with STEMI within 12–24 h after admission and was more effective in predicting the incidence of long-term MACEs than NLR measured at other time points (such as on emergency admission).19 Consistent with the above, our study demonstrated for the first time that SIRI serum value peaks at 12 h after PCI in patients with STEMI and is superior to SIRI measured before PCI and at discharge and also superior to dynamic fluctuations in SIRI between time points for predicting clinical outcomes.
As a new indicator of systemic immune-inflammatory status, PIV consists of neutrophil, monocyte, lymphocyte, and platelet counts; moreover, it is a combination of NLR, MLR, and platelet-to-lymphocyte ratio (PLR). PLR is also an independent predictor of postoperative MACEs in patients with MI.20 Several studies have shown that an increased platelet count may be involved in the development and progression of coronary heart disease.40 Increased platelet counts lead to a sustained inflammatory response, with platelets aggregating and adhering to the surface of endothelial cells of coronary arteries inducing the release of various mediators and recruiting inflammatory cells (such as monocytes), which in turn further exacerbates the inflammatory response, resulting in acute coronary events.10 Murat et al have analyzed the predictive efficacy of preoperative PIV and have reported that it was superior to NLR, PLR, and SII in predicting in-hospital and long-term mortality in patients with STEMI.14 Our study further compared the predictive efficacy of serum PIV at different time points and its dynamic fluctuations between time points on the concurrent adverse cardiovascular events in patients with STEMI within 1 year after PCI. PIV peaked at 12 h after PCI and was better at predicting clinical outcomes than PIV measured before PCI and at discharge and was also superior to the dynamic fluctuations of PIV between time points.
This study had several limitations. First, it explored the value of serum inflammatory indicators (SII, SIRI, and PIV) and their dynamic fluctuations between time points for predicting poor prognosis in patients with STEMI but not in patients non-STEMI. Second, this was a single-center retrospective study with a relatively small sample size; therefore, these results require validation in larger multicenter prospective studies.
Conclusions
This study retrospectively analyzed for the first time values and dynamic fluctuations of serum inflammatory markers (SII, SIRI, and PIV) at multiple time points from admission to discharge in patients with STEMI and compared their predictive efficacy for long-term poor prognosis. SIRI or PIV at 12 h after PCI may be more accurate and economical prognostic markers in clinical practice, with the potential to guide the follow-up, optimize post-discharge management, improve the quality of life, and prolong the life expectancy of high-risk patients. Further research in a larger patient cohort is needed to validate these results and evaluate the predictive efficacy of SIRI or PIV at 12 h after PCI as biomarkers for long-term adverse prognosis in patients with STEMI.
Data Sharing Statement
Data from this study are available from the corresponding author upon request.
Ethical Approval and Informed Consent
This study was conducted in accordance with the Declaration of Helsinki and was approved by the Local Ethics Committee of the 904th Hospital of the People’s Liberation Army Joint Logistic Support Force (The ethics approval number was 20230324). Considering the retrospective nature of the study, the requirement for patient consent was waived by the ethics committee. All patient data were anonymized or maintained confidentially.
Author Contributions
All authors made a considerable contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be submitted for publication; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported by the Major Provincial Health Care Commission (ZD2021020), the Key topics in medical and health of Wuxi Bureau of Science and Technology, Jiangsu Province (Y2021011), and the Natural Science Foundation of Jiangsu Province (BK20201139).
Disclosure
The authors declare that there are no conflicts of interest.
References
1. Vaduganathan M, Mensah GA, Turco JV, Fuster V, Roth GA. The global burden of cardiovascular diseases and risk: a compass for future health. J Am Coll Cardiol. 2022;80(25):2361–2371. PMID: 36368511. doi:10.1016/j.jacc.2022.11.005
2. Ibanez B, James S, Agewall S, et al.; ESC Scientific Document Group. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–177. PMID: 28886621. doi:10.1093/eurheartj/ehx393
3. Vogel B, Claessen BE, Arnold SV, et al. ST-segment elevation myocardial infarction. Nat Rev Dis Primers. 2019;5(1):39. PMID: 31171787. doi:10.1038/s41572-019-0090-3
4. Khera S, Kolte D, Gupta T, et al. Temporal trends and sex differences in revascularization and outcomes of ST-segment elevation myocardial infarction in younger adults in the United States. J Am Coll Cardiol. 2015;66(18):1961–1972. PMID: 26515998. doi:10.1016/j.jacc.2015.08.865
5. Desai MM, Stauffer BD, Feringa HH, Schreiner GC. Statistical models and patient predictors of readmission for acute myocardial infarction: a systematic review. Circ Cardiovasc Qual Outcomes. 2009;2(5):500–507. PMID: 20031883. doi:10.1161/CIRCOUTCOMES.108.832949
6. Falk E. Pathogenesis of atherosclerosis. J Am Coll Cardiol. 2006;47(8 Suppl):C7–12. PMID: 16631513. doi:10.1016/j.jacc.2005.09.068
7. Pietilä KO, Harmoinen AP, Jokiniitty J, Pasternack AI. Serum C-reactive protein concentration in acute myocardial infarction and its relationship to mortality during 24 months of follow-up in patients under thrombolytic treatment. Eur Heart J. 1996;17(9):1345–1349. PMID: 8880019. doi:10.1093/oxfordjournals.eurheartj.a015068
8. Kumar V, Prabhu SD, Bansal SS. CD4+ T-lymphocytes exhibit biphasic kinetics post-myocardial infarction. Front Cardiovasc Med. 2022;9:992653. PMID: 36093172; PMCID: PMC9452745. doi:10.3389/fcvm.2022.992653
9. Kumar V, Rosenzweig R, Asalla S, Nehra S, Prabhu SD, Bansal SS. TNFR1 contributes to activation-induced cell death of pathological CD4+ T lymphocytes during ischemic heart failure. JACC Basic Transl Sci. 2022;7(10):1038–1049. PMID: 36337927; PMCID: PMC9626895. doi:10.1016/j.jacbts.2022.05.005
10. Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005;352(16):1685–1695. PMID: 15843671. doi:10.1056/NEJMra043430
11. Balta S, Ozturk C. The platelet-lymphocyte ratio: a simple, inexpensive and rapid prognostic marker for cardiovascular events. Platelets. 2015;26(7):680–681. PMID: 25549287. doi:10.3109/09537104.2014.979340
12. Öcal L, Keskin M, Cerşit S, et al. Systemic immune-inflammation index predicts in-hospital and long-term outcomes in patients with ST-segment elevation myocardial infarction. Coron Artery Dis. 2022;33(4):251–260. PMID: 35044330. doi:10.1097/MCA.0000000000001117
13. Han K, Shi D, Yang L, et al. Prognostic value of systemic inflammatory response index in patients with acute coronary syndrome undergoing percutaneous coronary intervention. Ann Med. 2022;54(1):1667–1677. PMID: 35695557; PMCID: PMC9225721. doi:10.1080/07853890.2022.2083671
14. Murat B, Murat S, Ozgeyik M, Bilgin M. Comparison of pan-immune-inflammation value with other inflammation markers of long-term survival after ST-segment elevation myocardial infarction. Eur J Clin Invest. 2023;53(1):e13872. PMID: 36097823. doi:10.1111/eci.13872
15. Thygesen K, Alpert JS, Jaffe AS, et al. Executive group on behalf of the joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) task force for the universal definition of myocardial infarction. fourth universal definition of myocardial infarction. Circulation. 2018;138(20):e618–e651. PMID: 30571511. doi:10.1161/CIR.0000000000000617
16. Verheggen PW, de Maat MP, Cats VM, et al. Inflammatory status as a main determinant of outcome in patients with unstable angina, independent of coagulation activation and endothelial cell function. Eur Heart J. 1999;20(8):567–574. PMID: 10337541. doi:10.1053/euhj.1998.1312
17. Niccoli G, Burzotta F, Galiuto L, Crea F. Myocardial no-reflow in humans. J Am Coll Cardiol. 2009;54(4):281–292. PMID: 19608025. doi:10.1016/j.jacc.2009.03.054
18. Liu Y, Ye T, Chen L, et al. Systemic immune-inflammation index predicts the severity of coronary stenosis in patients with coronary heart disease. Coron Artery Dis. 2021;32(8):715–720. PMID: 33826540. doi:10.1097/MCA.0000000000001037
19. Núñez J, Núñez E, Bodí V, et al. Usefulness of the neutrophil to lymphocyte ratio in predicting long-term mortality in ST segment elevation myocardial infarction. Am J Cardiol. 2008;101(6):747–752. PMID: 18328833. doi:10.1016/j.amjcard.2007.11.004
20. Ozcan Cetin EH, Cetin MS, Aras D, et al. Platelet to lymphocyte ratio as a prognostic marker of in-hospital and long-term major adverse cardiovascular events in ST-segment elevation myocardial infarction. Angiology. 2016;67(4):336–345. PMID: 26101368. doi:10.1177/0003319715591751
21. Nichols M, Townsend N, Scarborough P, Rayner M. Cardiovascular disease in Europe 2014: epidemiological update. Eur Heart J. 2014;35(42):2950–2959. PMID: 25139896. doi:10.1093/eurheartj/ehu299
22. Tsai TH, Chua S, Hussein H, et al. Outcomes of patients with Killip class III acute myocardial infarction after primary percutaneous coronary intervention. Crit Care Med. 2011;39(3):436–442. PMID: 21242801. doi:10.1097/CCM.0b013e318206ccc3
23. Ndrepepa G, Tiroch K, Keta D, et al. Predictive factors and impact of no reflow after primary percutaneous coronary intervention in patients with acute myocardial infarction. Circ Cardiovasc Interv. 2010;3(1):27–33. PMID: 20118156. doi:10.1161/CIRCINTERVENTIONS.109.896225
24. Morishima I, Sone T, Mokuno S, et al. Clinical significance of no-reflow phenomenon observed on angiography after successful treatment of acute myocardial infarction with percutaneous transluminal coronary angioplasty. Am Heart J. 1995;130(2):239–243. PMID: 7631601. doi:10.1016/0002-8703(95)90434-4
25. Xu Y, He H, Zang Y, et al. Systemic inflammation response index (SIRI) as a novel biomarker in patients with rheumatoid arthritis: a multi-center retrospective study. Clin Rheumatol. 2022;41(7):1989–2000. PMID: 35266094. doi:10.1007/s10067-022-06122-1
26. Geng Y, Zhu D, Wu C, et al. A novel systemic inflammation response index (SIRI) for predicting postoperative survival of patients with esophageal squamous cell carcinoma. Int Immunopharmacol. 2018;65:503–510. PMID: 30408627. doi:10.1016/j.intimp.2018.10.002
27. Zhang Y, Xing Z, Zhou K, Jiang S. The predictive role of Systemic Inflammation Response Index (SIRI) in the prognosis of stroke patients. Clin Interv Aging. 2021;16:1997–2007. PMID: 34880606; PMCID: PMC8645951. doi:10.2147/CIA.S339221
28. Jin Z, Wu Q, Chen S, et al. The associations of two novel inflammation indexes, SII and SIRI with the risks for cardiovascular diseases and all-cause mortality: a ten-year follow-up study in 85,154 individuals. J Inflamm Res. 2021;14:131–140. PMID: 33500649; PMCID: PMC7822090. doi:10.2147/JIR.S283835
29. Sen N, Afsar B, Ozcan F, et al. The neutrophil to lymphocyte ratio was associated with impaired myocardial perfusion and long term adverse outcome in patients with ST-elevated myocardial infarction undergoing primary coronary intervention. Atherosclerosis. 2013;228(1):203–210. PMID: 23489347. doi:10.1016/j.atherosclerosis.2013.02.017
30. Song FH, Zheng YY, Tang JN, et al. A correlation between monocyte to lymphocyte ratio and long-term prognosis in patients with coronary artery disease after PCI. Clin Appl Thromb Hemost. 2021;27:1076029621999717. PMID: 33749340; PMCID: PMC7989235. doi:10.1177/1076029621999717
31. Dragu R, Huri S, Zukermann R, et al. Predictive value of white blood cell subtypes for long-term outcome following myocardial infarction. Atherosclerosis. 2008;196(1):405–412. PMID: 17173924. doi:10.1016/j.atherosclerosis.2006.11.022
32. Guasti L, Dentali F, Castiglioni L, et al. Neutrophils and clinical outcomes in patients with acute coronary syndromes and/or cardiac revascularisation. A systematic review on more than 34,000 subjects. Thromb Haemost. 2011;106(4):591–599. PMID: 21866299. doi:10.1160/TH11-02-0096
33. Major AS, Fazio S, Linton MF. B-lymphocyte deficiency increases atherosclerosis in LDL receptor-null mice. Arterioscler Thromb Vasc Biol. 2002;22(11):1892–1898. PMID: 12426221. doi:10.1161/01.atv.0000039169.47943.ee
34. Blum A, Sclarovsky S, Rehavia E, Shohat B. Levels of T-lymphocyte subpopulations, interleukin-1 beta, and soluble interleukin-2 receptor in acute myocardial infarction. Am Heart J. 1994;127(5):1226–1230. PMID: 8172050. doi:10.1016/0002-8703(94)90040-x
35. Ommen SR, Gibbons RJ, Hodge DO, Thomson SP. Usefulness of the lymphocyte concentration as a prognostic marker in coronary artery disease. Am J Cardiol. 1997;79(6):812–814. PMID: 9070569. doi:10.1016/s0002-9149(96)00878-8
36. Gisterå A, Hansson GK. The immunology of atherosclerosis. Nat Rev Nephrol. 2017;13(6):368–380. PMID: 28392564. doi:10.1038/nrneph.2017.51
37. Lindau A, Härdtner C, Hergeth SP, et al. Atheroprotection through SYK inhibition fails in established disease when local macrophage proliferation dominates lesion progression. Basic Res Cardiol. 2016;111(2):20. EPMID: 26891724; PMCID: PMC4759214. doi:10.1007/s00395-016-0535-8
38. Gratchev A, Sobenin I, Orekhov A, Kzhyshkowska J. Monocytes as a diagnostic marker of cardiovascular diseases. Immunobiology. 2012;217(5):476–482. PMID: 22325375. doi:10.1016/j.imbio.2012.01.008
39. Li G, Hao Y, Wang C, Wang S, Xiong Y, Zhao X. Association between neutrophil-to-lymphocyte ratio/lymphocyte-to-monocyte ratio and in-hospital clinical outcomes in ischemic stroke treated with intravenous thrombolysis. J Inflamm Res. 2022;15:5567–5578. PMID: 36185640; PMCID: PMC9518842. doi:10.2147/JIR.S382876
40. Ibrahim H, Schutt RC, Hannawi B, DeLao T, Barker CM, Kleiman NS. Association of immature platelets with adverse cardiovascular outcomes. J Am Coll Cardiol. 2014;64(20):2122–2129. PMID: 25457402. doi:10.1016/j.jacc.2014.06.1210

