Blood
Medicare approves WashU Medicine’s whole-genome test for blood cancers | Washington University School of Medicine in St. Louis
Complete picture of genetic errors can advance precision medicine approaches to treatment
<img width="700" height="467" src="https://medicalguru.us/wp-content/uploads/2023/08/ChromoSeq-screenschot-forweb-700×467-1.jpg" class="attachment-large size-large wp-post-image" alt decoding="async" srcset="https://medicalguru.us/wp-content/uploads/2023/08/ChromoSeq-screenschot-forweb-700×467-1.jpg 700w, https://medicalguru.us/wp-content/uploads/2023/08/ChromoSeq-screenschot-forweb-300×200-1.jpg 300w, https://medicalguru.us/wp-content/uploads/2023/08/ChromoSeq-screenschot-forweb-1536×1024-1.jpg 1536w, https://medicalguru.us/wp-content/uploads/2023/08/ChromoSeq-screenschot-forweb-600×400-1.jpg 600w, https://medicalguru.us/wp-content/uploads/2023/08/ChromoSeq-screenschot-forweb-186×124-1.jpg 186w, https://medicalguru.us/wp-content/uploads/2023/08/ChromoSeq-screenschot-forweb-220×147-1.jpg 220w, https://medicalguru.us/wp-content/uploads/2023/08/ChromoSeq-screenschot-forweb.jpg 1961w" sizes="(max-width: 700px) 100vw, 700px" data-attachment-id="123813" data-permalink="https://medicine.wustl.edu/news/medicare-approves-washu-medicines-whole-genome-test-for-blood-cancers/chromoseq-screenschot-forweb/" data-orig-file="https://medicalguru.us/wp-content/uploads/2023/08/ChromoSeq-screenschot-forweb.jpg" data-orig-size="1961,1307" data-comments-opened="0" data-image-meta="{"aperture":"0","credit":"","camera":"","caption":"","created_timestamp":"0","copyright":"","focal_length":"0","iso":"0","shutter_speed":"0","title":"","orientation":"0"}" data-image-title="ChromoSeq-screenschot-forweb" data-image-description data-image-caption="
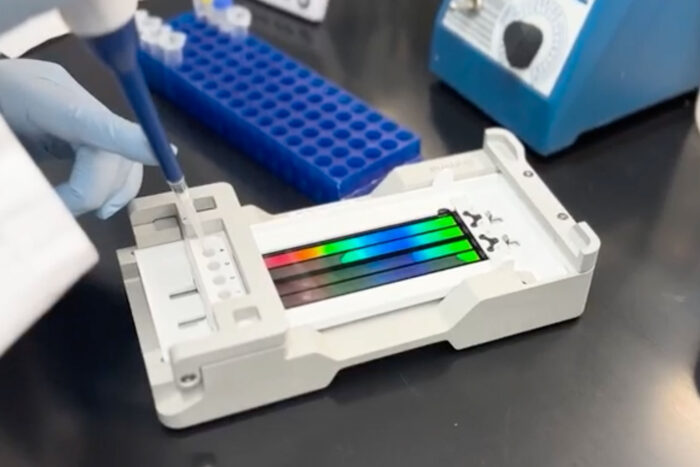
A laboratory worker loads a sample to run a ChromoSeq test, a new test for two blood cancers developed by a team at Washington University School of Medicine in St. Louis. ChromoSeq is the first whole-genome sequencing test for cancer to be approved for reimbursement by the Centers for Medicare & Medicaid Services.
” data-medium-file=”https://medicalguru.us/wp-content/uploads/2023/08/ChromoSeq-screenschot-forweb-300×200-1.jpg” data-large-file=”https://medicalguru.us/wp-content/uploads/2023/08/ChromoSeq-screenschot-forweb-700×467-1.jpg”>Katie Gertler
A laboratory worker loads a sample to run a ChromoSeq test, a new test for two blood cancers developed by a team at Washington University School of Medicine in St. Louis. ChromoSeq is the first whole-genome sequencing test for cancer to be approved for reimbursement by the Centers for Medicare & Medicaid Services.
A new test for two blood cancers – developed by a team at Washington University School of Medicine in St. Louis – is the first whole-genome sequencing test for cancer to be approved for reimbursement by the Centers for Medicare & Medicaid Services. The test, known as ChromoSeq, advances precision medicine approaches for treating blood cancers by identifying the full suite of genetic changes in a patient’s cancer cells, which provides crucial information that physicians can use to help determine the optimal treatment strategy for individual patients.
Since 2021, ChromoSeq has been used routinely by Washington University oncologists to guide treatment decisions for patients at Siteman Cancer Center with acute myeloid leukemia (AML) or a group of blood cancers called myelodysplastic syndrome (MDS). Siteman is based at Barnes-Jewish Hospital and Washington University. With Medicare approval for the test, physicians nationwide caring for Medicare patients diagnosed with AML or MDS will be able to order the test through Washington University Pathology Services, and Medicare will cover the cost.
“This approval reflects the power and clinical validity of ChromoSeq to assess the full range of genetic mutations responsible for some of the most deadly blood cancers, which can help guide treatment decisions for individual patients,” said Richard Cote, MD, the Edward Mallinckrodt Professor and head of the Department of Pathology & Immunology, which runs the pathology service in collaboration with the clinical sequencing laboratory at WashU Medicine’s McDonnell Genome Institute. “Private insurance companies often follow Medicare’s lead in coverage decisions, so we expect that there will be demand for this test across the country. This approval stands as a testament to the vision of WashU physician-scientists Eric Duncavage, Dave Spencer, Molly Schroeder and their team, who spent years developing and validating this test.”
In recent years, as genome sequencing technology has advanced, costs have dropped dramatically – helping to make Medicare reimbursement possible. The testing will be performed by the McDonnell Genome Institute, which has extensive expertise in genome sequencing and analysis. Scientists at the Genome Institute were the first in the world to demonstrate the validity of whole-genome sequencing in identifying genetic errors responsible for the development and progression of cancer.
The treatment for AML and MDS depends on the cancers’ aggressiveness in individual patients. Aggressive cancers require intensive treatment with chemotherapy drugs and sometimes a stem cell transplant to put the cancer in remission, while less aggressive blood cancers often can be effectively treated with less intensive drug regimens. Treatment decisions typically hinge on the genetic changes exhibited by a patient’s cancer. Standard tests used in a patient’s diagnostic workup are only able to assess some of these changes and provide a limited view of the genetic errors that may be driving the development of a patient’s cancer.
Under the current standard of care, genetic changes are assessed using a combination of three tests: cytogenetics, which reveals chromosomal rearrangements and abnormalities; fluorescence in-situ hybridization, which also identifies chromosomal abnormalities as well as other mutations; and targeted sequencing of specific genes that previously have been linked to AML and MDS.
In 2021, David H. Spencer, MD, PhD, an associate professor of medicine; Eric J. Duncavage, MD, a professor of pathology & immunology; Molly C. Schroeder, PhD, an assistant professor of pathology & immunology; Shelly O’Laughlin, the director of clinical operations at the Genome Technology Access Center at the McDonnell Genome Institute; and Timothy J. Ley, MD, the Lewis T. and Rosalind B. Apple Professor of Medicine, published a groundbreaking paper in The New England Journal of Medicine showing that ChromoSeq is at least as accurate and often better than conventional genetic tests at providing the information necessary for doctors to determine the best treatment.
“All of the information that you can get from the three different tests that doctors now order as standard of care, we can get from ChromoSeq in one test,” said Meagan Jacoby, MD, PhD, an associate professor of medicine. “That can be important because sometimes the other tests don’t produce reliable results, and without that data, we have less confidence in our ability to assess a patient’s risk of aggressive disease. Knowing whether a patient is at low or high risk of aggressive disease is essential for us to know how to treat each patient most appropriately.”
Jacoby leads two ongoing clinical trials to evaluate how the data provided by ChromoSeq compares with standard-of-care testing, and how doctors use ChromoSeq under real-life conditions. Since ChromoSeq gathers data on the whole genome, it can scan for known mutations that are too rare to be included in targeted genetic sequencing tests. Jacoby said that preliminary data from the two ongoing clinical trials suggests that, in comparison to conventional tests, ChromoSeq can generate additional information that could change how individual patients are treated. The full impact of using ChromoSeq won’t be known until the trials are completed.
ChromoSeq also can be quickly updated as more information becomes available about how particular genetic changes contribute to blood cancers.
“If we want to look at additional genes or mutations, all we’d have to do is modify our data analysis slightly,” said Spencer, also the medical director of the clinical sequencing facility at the McDonnell Genome Institute. “Analysis of new regions would still need to be validated, but technical aspects of the assay in the lab would not need to be changed.”
The development of ChromoSeq is the latest in a long tradition of groundbreaking achievements in genomic science at WashU Medicine. In 2008, Ley and colleagues at the McDonnell Genome Institute became the first in the world to use whole-genome sequencing to identify the full suite of genetic changes in a cancer patient’s tumor cells and trace the patient’s cancer to its genetic roots. This pioneering work laid the groundwork for numerous other studies of whole-genome sequencing in virtually every kind of cancer, and advanced precision medicine approaches to cancer treatment that are based on the underlying genetics of a patient’s tumor.
“Sequencing the first cancer genome was a phenomenal achievement that took over a year and cost over $1 million dollars,” said Duncavage, also chief of the molecular oncology section in the Department of Pathology & Immunology. “Now we’ve reached the point where we can sequence a cancer genome in a few days for a few thousand dollars, and Medicare will cover the cost as it does for other clinical tests.”
The researchers now are working on developing whole-genome sequencing approaches to other forms of cancer, starting with other blood cancers such as acute lymphocytic leukemia and multiple myeloma.
“We chose those cancers because they involve the same kinds of patient samples — blood and bone marrow — so we can use the same laboratory procedures that we established for AML and MDS,” Spencer said. “With only slight modifications to this assay I can see a lot of potential for whole-genome sequencing to transform how we diagnose and treat other kinds of cancer.”