Infection
Glycans and GBPs: How their interplay shapes immunity in infection and autoimmune diseases
In a recent review published in Cellular and Molecular Immunology, researchers discuss the regulatory roles of glycans and glycan-binding proteins (GBPs) in modulating immune responses, particularly in the context of autoimmune inflammation and chronic infection.
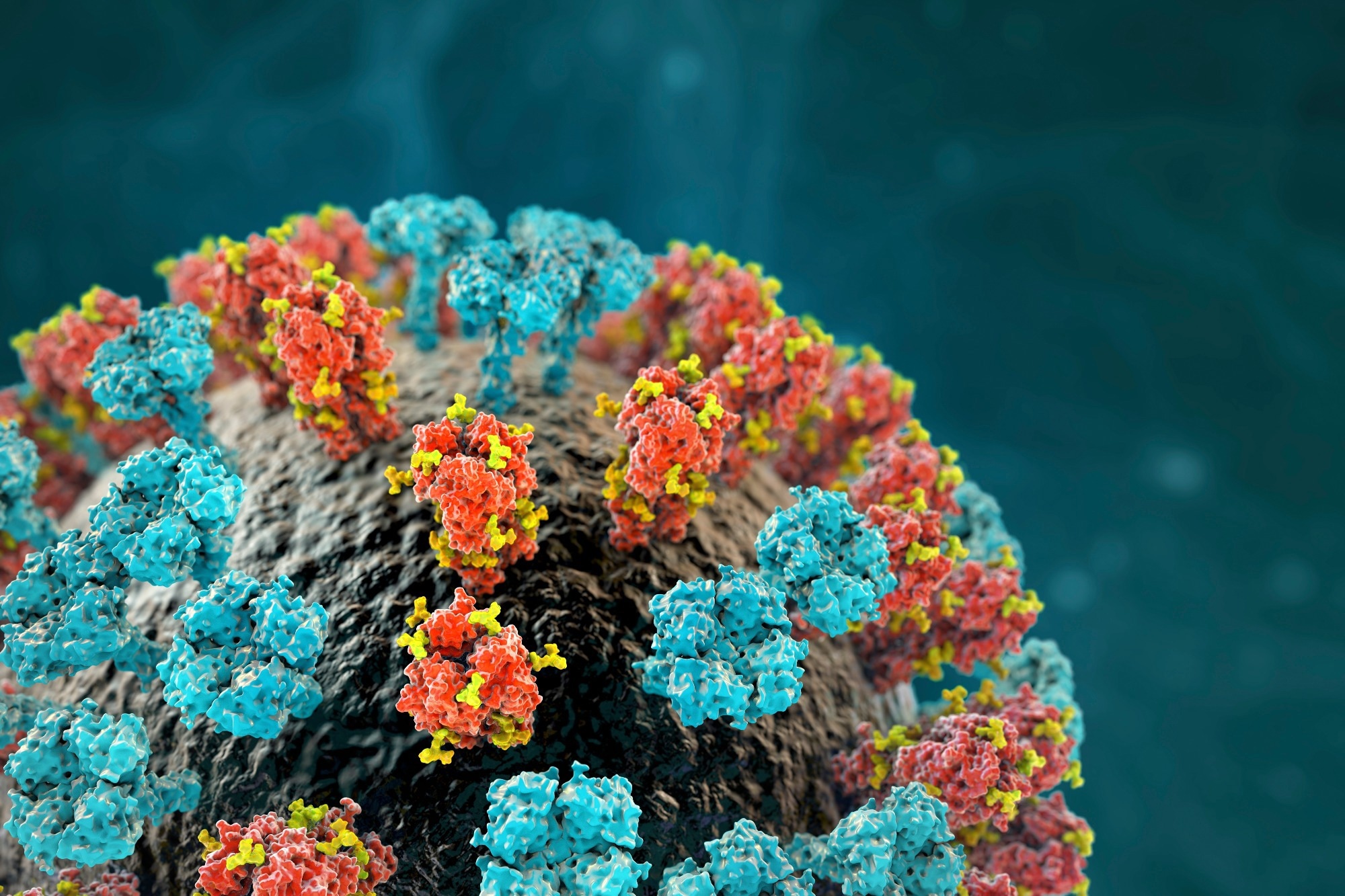
Study: Immune regulatory networks coordinated by glycans and glycan-binding proteins in autoimmunity and infection. Image Credit: Kateryna Kon / Shutterstock.com
Background
The immune system protects the body against external threats and internal abnormalities. Any disruption can lead to inflammation, autoimmune disorders, or even malignancy. Glycans are crucial components of a functioning immune system, as they interact with GBPs like lectins to create interfaces that influence various immune processes, including infection and cancer.
Protein glycosylation facilitates cell communication, particularly within the immune system. Thus, any change in cellular glycans can lead to pathological conditions.
Pathogens also utilize glycans to promote infections, a mechanism that is often utilized during vaccine development. Glycans can dictate self from non-self, thus explaining some microbial strategies and autoimmune reactions. Nevertheless, additional research is needed to elucidate how glycans and GBPs impact immune responses to understand their role in inflammation and infection.
Protein glycosylation
Protein glycosylation, a crucial posttranslational modification, dictates significant cellular functions in tissues and organisms. This modification is widespread, with anomalies found in many human diseases.
The “glycome” encompasses the myriad of glycans linked to proteins and lipids. These glycans drive processes like protein folding, cell communication, development, and essential interactions in the immune system.
GBPs, including galectins and sialic acid-binding immunoglobulin-like lectins (siglecs), are often considered the “sugar code” of biological information. Essential to biology and medicine, understanding protein glycosylation hinges on the cellular machinery in the endoplasmic reticulum (ER) and Golgi compartments that contribute to glycan diversity.
N-linked glycoproteins constitute a significant portion of this modification and are essential for cellular balance. Comparatively, O-linked glycoproteins, including mucins, contribute to the diverse functions related to glycosylation.
Glycans serve structural, metabolic, and informative roles as they influence many processes ranging from disease to immunity. It is evident that glycan alterations significantly influence disease mechanisms and, as a result, may serve as biomarkers in clinical scenarios.
Synchronizing immune tolerance: glycans and GBPs
Glycans present on the surface of immune cells can be interpreted by GBPs, which subsequently leads to critical immune responses, such as determining “self” from “non-self.” Glycans and GBPs form multifaceted interactions, serving as pivotal regulators of immune tolerance. Within this system, GBPs specifically identify particular glycan structures, which impact functions like pathogen recognition and immune cell activation.
Three lectin families, including C-type lectins, galectins, and siglecs serve crucial roles in immune regulation.
C-type lectins primarily recognize specific sugars to control both innate and adaptive immunity. Galectins, which are widely found in immune cells, interact with specific sugar structures on cell surfaces, thus influencing various functions ranging from endocytosis to signaling. These proteins can regulate both anti-inflammatory and pro-inflammatory responses.
Comparatively, siglecs interact with sialic-acid-containing glycans, which are involved in phagocytosis and pathogen interactions.
Glycans and GBP in infection
In host-pathogen interactions, numerous cellular and molecular interactions occur, many of which involve glycans and GBPs. For example, in antibody-mediated immune reactions, the relationship between glycans and GBPs is essential, with glycans attached to antibodies determining either pro-inflammatory or anti-inflammatory responses.
Microbial glycans, which are distinct from pathogen-driven epitopes like proteins and deoxyribonucleic acid (DNA), are vital in self/non-self differentiation. The dynamics between pathogen glycomes and host-derived GBPs are not fully understood; however, the host immune system employs various GBPs for pathogen identification, which influences both innate and adaptive immune responses.
Eukaryotic cells, such as fungi, possess ER and Golgi glycosylation machinery, with their N-glycome resembling that of mammalian cells. Host GBPs, including dendritic cell-specific intercellular adhesion molecule-3-grabbing non-integrin (DC-SIGN) and Dectin-1, recognize specific glycan structures in fungi. For example, glycan recognition during Candida albicans infection influences human DC responses.
Viruses exploit host enzymes for glycosylation by generating glycans resembling those in infected cells. This type of glycosylation impacts the immune system’s ability to recognize viruses, as well as the ability of the virus to infect and evade immunity. The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative agent of the coronavirus disease 2019 (COVID-19), exhibits glycan structures significant for cell interaction.
Bacteria also exhibit O- and N-glycosylation mechanisms. Mycobacterium tuberculosis (Mtb) has glycans pivotal for infection, as they dictate internalization, colonization, and further infection.
Galectins also interact with bacterial surface glycans, thereby affecting bacterial movement and immune responses. These findings demonstrate that a complex network of glycans and GBPs mediate various aspects of infections.
Glycans and GBPs in chronic inflammation and autoimmune conditions
In the progression from healthy to inflamed tissue, cellular glycosylation changes are observed. Inflammation and autoimmune diseases lead to significant alterations in cellular glycosylation patterns, such as the reduced expression of N-acetylglucosaminyltransferase V (MGAT5).
Inflammatory bowel disease (IBD), a severe gastrointestinal condition, is often accompanied by abnormalities in glycosylation. For example, mice without β1,6-branched N-glycans are more prone to severe colitis; however, treatment with N-acetylglucosamine (GlcNAc) reduces the severity of this condition.
Glycosylation also impacts the activity of GBPs, including galectins. The disruption of galectin-1 signaling in IBD patients, for example, has significant implications for gut immunity.
During the resolution phase of autoimmune inflammation, glycans play a part in restoring immune cell balance. These intricate interactions reflect the significant role of glycosylation in inflammation and autoimmune disorders.
Conclusions
In the post-genomic era, studying the glycome has revealed essential immune pathways, thus deepening our grasp of innate and adaptive immunity. Glycans and GBPs, like galectins and siglecs, are key to these processes, as they modulate immune checkpoints and T-cell functions, while various pathogens utilize glycans for host interactions.
Host cells mirror these glycan structures, either amplifying immunity or aiding disease resolution. GBPs decode these interactions; however, further research is needed to better understand the concept of glycoimmunology and ultimately leverage this information for therapeutic advancements in conditions ranging from infections to cancers.