Infection
MDR Escherichia coli Infections in Young Children
Introduction
Escherichia coli, a gram-negative pathogen in the Enterobacteriaceae family, is a significant cause of bloodstream, urinary tract, gastrointestinal, and respiratory infections worldwide.1 The global incidence of E. coli infections is increasing, according to the Global Burden of Foodborne Diseases report. Approximately 111 million illnesses and 63,000 deaths are attributed to diarrheagenic E. coli annually worldwide, Infection rates vary across different regions.2 This substantial burden necessitates a comprehensive understanding of the pathogen’s impact and its growing antimicrobial resistance crisis. This alarming burden highlights the urgent need for effective strategies to tackle E. coli infections and their associated challenges. Notably, the impact of E. coli on bloodstream infections, while not as clear as its role in urinary tract infections, has been identified as a leading cause of bloodstream infections.3 E. coli infections impose a substantial burden on pediatric health, affecting various body sites and warranting a comprehensive understanding of their prevalence and implications for effective disease management.4 E. coli bloodstream infections were not widely recognized as a common issue at the beginning of the 20th century; however, it has been consistently rising worldwide over the decades as shown by numerous studies.5,6 The gut microbiome is a common source of extraintestinal infections caused by E. coli and its population varies among individuals of different ages and lifestyles.7 The emergence of E. coli is a critical issue in the context of antimicrobial resistance, as its resistance rates are increasing worldwide, including in China.8 The complexity and incomplete understanding of antibiotic resistance development and dissemination are widely acknowledged. Despite numerous studies that demonstrate a correlation between the use of antibiotics and the emergence of antibiotic-resistant bacteria, the extent to which such selection is influenced by ecological or individual factors remains to be further elucidated.9,10 The impact of prior hospital exposure on trends in E. coli bloodstream infections, urinary tract infections and gastrointestinal infections has not been thoroughly investigated specifically in children. Recently, two studies from China were published indicating that among cases of bloodstream infection, 60–70% are caused by gram-negative bacteria, with E. coli being the predominant species that have been isolated.11,12 A MEDLINE database search with keywords such as “bloodstream infection”, “urinary tract infection”, “antimicrobial susceptibility”, and “China” yielded around 286 studies, but none of them focused on the trends of E. coli in these infections. A multicentre study revealed that E. coli infections with increased antimicrobial resistance occurred in China according to the China Antimicrobial Surveillance Network (CHINET-http://www.chinets.com,2016).12 A 12-year retrospective study suggests that Extended-spectrum β-lactamase (ESBL) -producing E. coli were resistant to ciprofloxacin, cefotaxime, and amoxicillin. However, resistance to these antibiotics has been increasing over time.11 The reason for the high prevalence of E. coli bloodstream infections, and urinary tract infections, as well as the development of antibiotic resistance, may be linked to increased antibiotic usage in the population, individual hospitals and primary care.13 Our hospital adopted a new antibiotic therapy policy in 201514 while monitoring the changes in antibiotic-resistant bacteria to be better equipped to prevent disease. This study aimed to investigate possible changes in antibiotic resistance patterns and the burden of E. coli infection in the bloodstream, urinary tract, gastrointestinal tract and other sites from paediatric patients aged 0–14 years in Shenzhen, China.
Method
Study Setting, Design, and Population
This study was in line with the Declaration of Helsinki guidelines and was approved by the Research Ethics of Shenzhen Children’s Hospital (Decision No 2018/03) which complies with global ethical standards. In the course of this retrospective study, we obtained a total of 4723 non-duplicate specimens, including urine, sputum, pus, blood, stool, and throat swab samples, collected between January 1, 2014, and December 30, 2018. These specimens were systematically gathered as part of a routine antimicrobial resistance surveillance initiative, encompassing patients from distinct age groups (0–1, 2–5, 6–10, and 11–14 years), each exhibiting specific clinical symptoms indicative of various infection types. The collection was tailored to encompass patients with suspected bloodstream infections, urinary tract infections, gastrointestinal infections, and respiratory infections. In particular, symptoms such as severe body pain, fever, rapid breathing, and rash were used as criteria for identifying potential bloodstream infections, while signs like pyuria were indicative of urinary tract infection or inflammation. Similarly, gastrointestinal and respiratory infections were characterized by abdominal pain, diarrhoea, bronchitis, and lung abscess symptoms. Our comprehensive analysis evaluated the interplay of patient demographics with the incidence of E. coli infections across these distinct categories, accounting for age and sex adjustments based on population estimates provided by the Shenzhen Children’s Hospital’s record room. Notably, verbal consent was procured from patients for the use of anonymized data in research, following the standard operating procedures of Shenzhen Children’s Hospital. This retrospective design was approved by the Research Ethics Committee of Shenzhen Children’s Hospital, and our central research laboratory strictly adhered to good clinical and laboratory practice (GCLP) guidelines, ensuring the reliability and validity of our findings.
Specimen and Data Collection
Shenzhen Children’s Hospital has implemented an extensively defined standard operating procedure (SOP) for sample collection during paediatric clinical practices including rapid transportation of specimens to central laboratories. To assess the E. coli burden in the paediatric population urine, appendix, sputum, pus, blood, stool, and throat swab specimens were collected from patients suspected of having an E. coli infection using an aseptic technique and placed in sterile containers to prevent contamination by highly trained nursing staff. The samples were transported to the central laboratory, department of microbiology, within 30 minutes, and patient data, including age, gender, specimen type, and department of admission, was collated from the hospital record room in an Excel sheet.
Isolation and Identification of E. Coli
Samples suggestive of bloodstream infections, urinary tract infections, gastrointestinal infections, and respiratory infections were cultured on an enriched lauryl sulfate-aniline blue agar medium, MacConkey agar and 5% human blood agar. The plates were incubated aerobically at 37 °C/24 hrs and characterised phenotypically. The purity of the isolates was assessed and a colony count of ≥104 CFU/mL was considered significant. Bacterial identification was performed by the VITEK-2 system (bioMérieux, Lyon, France) which was further confirmed by the API-20E tests. Results were analysed and interpreted as per the manufacturer’s instructions.
Antimicrobial Susceptibility Testing
Antibiotic susceptibility testing (AST) was conducted on each isolate using the automated VITEK-2 system (bioMérieux, Lyon, France) and an ASTGN335 card, following the manufacturer’s instructions. The minimum inhibitory concentrations (MICs) were interpreted based on the clinical breakpoints published by the European Committee on Antimicrobial Susceptibility Testing (EUCAST, Version 9.0).15 Additionally, a broth microdilution method was employed, and the results were interpreted according to the Clinical and Laboratory Standards Institute (CLSI) guidelines (CLSI: M100-S22).16 The antibiotic susceptibility results were categorized as susceptible, intermediate, or resistant for antibiotics that belonged to the following classes categories: Penicillin’s – ampicillin, ampicillin/sulbactam, piperacillin/tazobactam; Monobactam – aztreonam; Fluoroquinolones – ciprofloxacin, levofloxacin; Cephalosporins – cefazolin, cefotetan, ceftazidime, ceftriaxone, cefepime; Aminoglycosides – amikacin, gentamicin, tobramycin; Carbapenems – ertapenem, imipenem; Nitrofurans – nitrofurantoin; and Sulfonamides – trimethoprim/sulfamethoxazole. Bacterial isolates that were resistant to at least one antibiotic of three or more antimicrobial classes were classed as multi-drug resistant (MDR).17 The results were validated by using E. coli (ATCC 25922) as a control strain. Furthermore, ESBL detection was performed by both the VITEK-2 system and double-disc diffusion method (DDDM) which includes a disc of amoxicillin-clavulanic acid (20/10 mcg), along with ceftriaxone (30 mcg), ceftazidime (30 mcg) and cefotaxime (30 mcg) to observe a synergistic reaction, a well-characterized strain of Salmonella typhimurium (SP-15-127) from our laboratory was used as a positive control.18 The distance between the discs is critical and 20 mm centre-to-centre. To assess the effect of antimicrobial resistance, which might also affect the treatment outcome we investigated resistance trends over the past 5 years among males and females, as well as assessed the prevalence of bloodstream infections, urinary tract infections, gastrointestinal infections and respiratory infections. We also evaluated the current choice of drugs available to treat these infections and sought to understand the severity of E. coli infection in young children.
Statistical Analysis
A chi-square test was performed to analyse the data using GraphPad Prism software, version 9, (GraphPad Software, San Diego, CA, USA). p-value ≤ 0.05 was considered to be statistically significant. Figures were created by using R ggplot2.
Results
Between Jan 1, 2014, to Dec 30, 2018, a total of 4214/4723 (89.22%) specimens’ cultures were positive on an enriched lauryl sulfate-aniline blue agar plate and primarily identified by the VITEK-2 system, of which 4148 (98.34%) were confirmed as E. coli by the API-20E system and colony morphology along with Gram staining. 66/4214 (1.57%) were false positives recorded by the VITEK-2 system and were subsequently excluded from the study. There were very few discrepancies in the identification of E. coli using both the VITEK-2 automated system and the API-20 method. Of which 2750 (66.31%) of the specimens were collected from hospitalised patients and 1398 (33.69%) from the outpatient department. The distribution of samples by the department was as follows: Infectious diseases had the highest number of cases with 1700 (40.98%), followed by our specialized respiratory infection department with 481 (11.59%), endocrinology 435 (10.48%), intensive care unit 396 (9.54%). Other departments with notable numbers of cases included surgery 279 (6.72%), haematology and oncology 252 (6.07%), immunology 236 (5.68%), gastrointestinal department 124 (2.98%), neurology 93 (2.24%), neonatology 87 (2.09%), and from an unknown source 65 (1.56%) (Supplementary Figure 1). Out of the 4148 cases of E. coli infection, 2645 (63.76%) were identified in male patients, and 1503 (36.23%) were identified in female patients with a mean age of 6.5 yrs. (median age 7 yrs.; SD 3·59 yrs.) (Figure 1). The overall prevalence of E. coli infection declined over the years but show the highest peak of each year in the mid (April to June) of 2014 and 2017. The age group 0–1 yr. had the highest burden of E. coli infection and further details on the burden of E. coli infections among the age groups are shown in Figure 1. The prevalence of E. coli infection was significantly higher in males than in females in the ages 11–14. group, [chi-square = 17.0533 (p-value is 0.0018)] while lower in the age group 6–10 yrs, [chi-square is 2.5942 (p-value is 0.62)] (Figure 2). Overall, between 2014–2018, the mean prevalence of E. coli infections was 829 with SD 238.10 (two-tailed p-value 0.005) but this number varied substantially across the study period. Out of 4148, 1481 (35.70%) isolates were recovered from urine samples, while 1343 (32.37%) were from sputum, 531 (12.80%) from pus, 423 (10.19%) from bloodstream infections and 230 (5.54%) from stool samples and 140 (3.37%) were recovered from throat swabs (Figure 3). The overall prevalence of E. coli gastrointestinal infection increased but that of respiratory infections declined year after year. The E. coli infection burden in urinary tract infections declined at a lower rate across the study period.
 |
Figure 1 Gender structured and trimester prevalence of Escherichia coli infection in young children in Shenzhen from 2014–2018. |
 |
Figure 2 Age Structured Escherichia coli infection in young children in Shenzhen from 2014–2018. |
 |
Figure 3 Escherichia coli abundance in different patient specimen samples over five years 2014–2018. |
Antimicrobial Susceptibility Profile
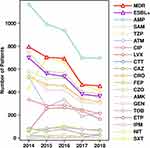
MICs determined by the automated AST VITEK-2 systems and by broth microdilution showed no discrepancies. Overall antimicrobial susceptibility results revealed that 3404 (82%) E. coli were highly resistant to ampicillin followed by cefazolin [n=2172, 52.36%], trimethoprim/sulfamethoxazole [n=1969, 47.46%], ampicillin/sulbactam [n=1895, 45.68%], ceftriaxone [n=1727, 41.63%], gentamicin [n=1496, 36.06%], aztreonam [n=1253, 30.20%], ciprofloxacin [n=1070, 25.79%] and levofloxacin [n=787, 18.97%], while lower resistance was observed against, cefepime [n=364, 8.77%], tobramycin [n=290, 6.99%], ceftazidime [n=264, 6.36%], piperacillin/tazobactam [n=82, 1.97%], cefotetan [n=79, 1.90%], amikacin [n=62, 1.49%] and nitrofurantoin [n=49, 1.18%]. Moreover, the results indicate that the majority of the E. coli isolates were sensitive to ertapenem, and imipenem (Figure 4). Out of the 4148 isolates tested, 744 (17.93%) were found to be sensitive to all tested antibiotics. The prevalence of ampicillin-resistant E. coli declined over subsequent years (Figure 5). An increase was observed in the case of cefepime, cefazolin, and ceftriaxone-resistant E. coli, whereas not many changes were observed in resistance against ciprofloxacin, gentamicin and ceftazidime. Our observations reveal that isolates obtained from gastrointestinal infection and urinary tract infections cases exhibit multiple drug-resistance phenotypes (the chi-square statistic is 0.7914, a p-value is 0.9396) (Supplementary Figure 2). We have found no compelling evidence to suggest that the development of drug resistance is linked to the infection site whether it is associated with bloodstream infections, urinary tract infections, or gastrointestinal infections. Our results suggested the use of imipenem and nitrofurantoin as the preferred drugs for treating bloodstream infections, urinary tract infections, respiratory infections and gastrointestinal infections shortly. Our results show that E. coli resistance to ciprofloxacin, cefepime, trimethoprim/sulfamethoxazole and piperacillin/tazobactam is significantly higher in females than males compared to other drugs (Supplementary Figure 3). Based on the specimens, all tested drugs were found to be significant (all P values <0.01), is revealed that the infection site of E. coli was not more concern but still high resistance was reported in urinary tract infections. The prevalence of ESBL-producing E. coli was found to be 49.54% [n=2055], and multidrug-resistant (MDR) phenotype was observed in 60% [n= 1233/2055] of the ESBL-producing isolates. Overall, the mean prevalence of ESBL over the 5 years was 411 with SD 116.8 (Two-tailed p-value 0.00045), but this number varied substantially across the study period, notably; the present study reported the declining prevalence of ESBL E. coli from 2014 −2018 in young children at Shenzhen, China (Figure 5). It is worth noting that a high prevalence of ESBL E. coli was found in age groups 0–1 years and it has contributed to the MDR phenotype in this organism. During the study period, not much change was observed in the age group 11–14 (Supplementary Figure 4).
 |
Figure 4 Overall antimicrobial susceptibility of Escherichia coli isolates collected from 2014–2018. Abbreviations: AMK, amikacin; AMP, ampicillin; ATM, aztreonam; CAZ, ceftazidime; CIP, ciprofloxacin; CRO, ceftriaxone; CTT, cefotetan; CZO, cefazolin; ETP, ertapenem; GEN, gentamicin; IMP, imipenem; LVX, levofloxacin; NIT, nitrofurantoin; SAM, ampicillin/sulbactam; SXT, trimethoprim/sulfamethoxazole; TOB, tobramycin; TZP, piperacillin-tazobactam. |
|
Figure 5 Antimicrobial resistance, MDR phenotype and ESBL production of Escherichia coli trends based on a year-on-year basis from 2014–2018. Abbreviations: AMK, amikacin; AMP, ampicillin; ATM, aztreonam; CAZ, ceftazidime; CIP, ciprofloxacin; CRO, ceftriaxone; CTT, cefotetan; CZO, cefazolin; ETP, ertapenem; GEN, gentamicin; IMP, imipenem; LVX, levofloxacin; NIT, nitrofurantoin; SAM, ampicillin/sulbactam; SXT, trimethoprim/sulfamethoxazole; TOB, tobramycin; TZP, piperacillin-tazobactam. |
Discussion
Escherichia coli is a significant pathogen in bloodstream infections and urinary tract infections, which can potentially lead to fatal outcomes. Proper characterization of these infections requires consideration of various factors such as epidemiology, antimicrobial susceptibility, and host determinants. A comprehensive understanding and analysis of these factors can aid in the development of effective treatment strategies and control measures to prevent the spread of E. coli infections in the bloodstream infection, wound infections, respiratory infections and urinary tract infections. This effect might be quantitatively small for an individual, but its overall contribution to the spread of antibiotic resistance in the population is important. The extensive sample size, well-defined sampling departments, and specimens, as well as the inclusion of only gender and age data of individual patients along with their antimicrobial susceptibility profiles, in our study, allowed us to gain further insight into the intricate interplay of factors associated with antibiotic resistance and the trends of E. coli infection in young children over five years. Moving forward, we plan to expand our research to include the geographical distribution of E. coli and the occurrence of bacteraemia and urinary tract infections. To detect the burden of E. coli in bloodstream infections, urinary tract infections, RI and GI cases, the determination of its presence in blood, urine, sputum, throat swabs and faecal samples depends on the decision of both physicians and patients to undergo culture tests. As a result, likely, the reported cases do not encompass all incident cases within the population or hospital admissions. It is expected that the missed incident cases are distributed equally across E. coli-related bloodstream infections, urinary tract infections, and GI cases. We have discovered that when detecting E. coli using an automated system such as Vitek-2 and API-20, we did not observe any significant differences. Moreover, both methods had been validated previously and yielded similar results to ours.19 Based on our laboratory’s practice, we recommend the use of enriched lauryl sulphate-aniline blue agar for culture E. coli. Our study indicates that the infectious diseases department has the highest burden of E. coli infections among admitted patients, followed by respiratory diseases, endocrinology, and the intensive care unit. The infectious disease departments are in high demand, as they cover a wide variety of infections and have the highest disease burden. Although there may be a higher number of reported cases, there have not been any studies reported from China to the best of our knowledge. Our study supports the previous finding that there is a high prevalence of E. coli pathogens in both the intensive care unit and general medicine departments.20 In our study, it was observed that the prevalence of E. coli infections (bloodstream infections and urinary tract infections) was higher in male patients at 63.31% (p<0.001) than in female patients at 36.69% among young children. These results were consistent with another study by Randi et al, which reported 77% of E. coli bloodstream infections in male adult patients.21 Although there are few population-based studies on sex differences in the epidemiology of BSI, to our knowledge, all studies have focused on the adult age group, and no previous studies have analysed sex differences in bloodstream infections or respiratory infections among young children. Several studies have suggested that females are more prone to urinary tract infections, due to their shorter urethra, which increases the risk of bacterial ascent from the perianal region into the bladder. However, we have observed a higher number of urinary tract infections in our male patients, which differs from other studies.22 Moreover, the prevalence of urinary tract infections has been found to vary among children of different ages and ethnic groups. Our observation that E. coli urinary tract infections are higher in males is supported by other studies. For instance, Alexander et al reported that E. coli is responsible for 80% to 90% of urinary tract infections in children, and the prevalence is higher in boys than in girls.23 Our findings have demonstrated a consistently higher prevalence of E. coli urinary tract infections (35.7%) in young children (excluding 2016 for gastrointestinal), compared to respiratory infection (35.7%), wound infection (12.78%), bloodstream infections (10.13%) and GI (5.55%). This is in line with the results of previous studies.24 The higher prevalence of E. coli urinary tract infections is driven by modifiable risk factors such as being overweight or obese and having poor fluid intake, which increase the risk of urinary tract infections in children.25 We have assessed the higher number of E. coli burden in the hospitalized patients about 2750 (66.31%) and among them, 1908 (46.0%) showed MDR phenotype. We hypothesised that crowded living conditions in hospitals might be associated with increased physical contact between people and with less hygienic conditions that further increase the risk of transmission of E. coli and other pathogens. Our hypothesis has been supported by Marcelo et al, which reported fluconazole-resistant E. coli transmission in a crowded population.10 However, generally, more crowded population conditions did not confer an increased risk for urinary tract infections, wound infections and bloodstream infection, except in places like overloaded hospitals where common instruments, washrooms, and shared wards facilitated the transmission of resistant bacteria or resistance genes within the population. Furthermore, molecular analyses such as pulse-feed gel electrophoresis and multi-locus typing /Whole genome sequencing studies are required to warrant the hypothesis. Antimicrobial stewardship has become increasingly crucial with the emergence of multi-drug-resistant E. coli, including the production of extended-spectrum beta-lactamases, which we identified in 2055 (49.54%) isolates, and is declining each year. Djuikoue et al, have highlighted a significant prevalence of ESBL-producing E. coli in blood samples of young children from Yaoundé, resulting in mortality among infants in Cameroon.26 Overall antimicrobial susceptibility results revealed that E. coli were highly resistant to ampicillin (82%), cefazolin (52.36%), trimethoprim/sulfamethoxazole (47.46%), ampicillin/sulbactam (45.68%), ceftriaxone (41.63%), gentamicin (36.06%), aztreonam (30.20%), ciprofloxacin (25.79%) and levofloxacin (18.97%). Moreover, the results indicate that the majority of the E. coli isolates were sensitive to ertapenem, and imipenem. The treatment guidelines suggest cefixime, cefpodoxime, cephalexin, ampicillin, and ceftriaxone being first-line agents used to treat uncomplicated bloodstream infections), wound infections or urinary tract infections.27 Unfortunately, many studies have suggested the highest growth of resistance against first-line antibiotics in E. coli, which is consistent with our findings.28 With the escalation of antibiotic resistance, managing infections caused by carbapenemase and ESBL-producing pathogens has become a progressively daunting endeavour. As treatment options diminish, colistin has reemerged as a final recourse antibiotic to address infections induced by these profoundly resistant pathogens29,30 Clinicians must review patient age, and gender-specific culture results and follow local antibiograms and antimicrobial sensitivity patterns available at their institution precisely so that appropriate therapy can be delivered. Our data suggest that imipenem and nitrofurantoin are the drugs of choice to treat multiple antibiotic-resistant E. coli infections in case of bloodstream infections, urinary tract infections, and gastrointestinal infections. Similar to our study, Sara et al have suggested that imipenem is effective in the treatment and control of serious infections caused by MDR E. coli and in the reduction of bacterial resistance emergence.31 As healthcare providers play a pivotal role in patient care, their understanding and recognition of the evolving patterns of antibiotic resistance are essential in guiding appropriate treatment decisions. Monitoring the prevalence of ESBL-producing E. coli infections in pediatric patients can offer valuable insights into the local and regional antimicrobial resistance trends, helping healthcare professionals make informed choices when prescribing antibiotics. By regularly assessing the susceptibility profiles of E. coli isolates, physicians, pharmacists, and other healthcare professionals can identify emerging trends of resistance and adjust empiric antibiotic therapies accordingly. Tailoring treatment regimens based on local resistance patterns can improve patient outcomes, reduce the risk of treatment failure, and mitigate the development of further antibiotic resistance. Furthermore, fostering collaboration and communication between healthcare facilities, researchers, and public health authorities is vital to effectively combat antimicrobial resistance. This exchange of data and information can lead to a more comprehensive understanding of the epidemiology of ESBL-producing E. coli infections and enable the implementation of evidence-based interventions to curb their spread. Education and awareness campaigns targeted at healthcare professionals can also play a significant role in promoting judicious antibiotic use and antimicrobial stewardship. Our results show the resistance development for ciprofloxacin, cefepime, trimethoprim/ sulfamethoxazole and piperacillin/tazobactam are significantly higher in girls, no gender base supportive studies published yet so further large-scale study required. The present study suggests that the specimen’s origin and tested all drugs were found to be significant, first report best of our knowledge. The research has several limitations. We were unable to obtain patient characteristics, accessibility to medical services before arriving at our hospital, self-prescribed consumption of antibiotics, and geographical area. Another limitation is that we could not assess the associations between individual-patient antibiotic use (not available in the research database) and the risk of resistant infections, or between specific empirical regimens and outcomes. These associations are important future research priorities. We only have antibiograms, but representative isolates should be selected for whole-genome sequencing. Their analysis could increase the understanding of the pathogenesis of E. coli in young children and provide a further picture of the molecular epidemiology of E. coli and identify any clonal relationship. Furthermore, we could not assess the associations between individual-patient antibiotic use and the risk of developing resistant infections. The data on individual antibiotic prescriptions were not included in the research database, which hinders our understanding of the impact of specific empirical treatment regimens on the development of antibiotic resistance. Lastly, the study’s retrospective design may have inherent limitations, including incomplete or missing data and potential biases in data collection. While we made efforts to minimize these limitations, they should be taken into consideration when interpreting the results. By acknowledging these limitations, we aim to provide a transparent assessment of the study’s scope and potential implications. Future research endeavours can build upon these limitations and address these gaps to further our understanding of E. coli infections and antibiotic resistance in pediatric clinical cases.
Conclusion
In summary, there has been a decline in the prevalence of E. coli infections burden in young children in Shenzhen, China. E. coli urinary tract infections were found to be the most challenging to the healthcare system among children aged 1–5 years. Notably, the use of first-line antibiotics, such as cefixime, cefpodoxime, cephalexin, ampicillin, and ceftriaxone in primary care, was associated with an increased subsequent prevalence of resistant E. coli bloodstream infections and urinary tract infections. This supports initiatives aimed at reducing the use of broad-spectrum and inappropriate antibiotics. The high rate of ESBL-producing E. coli and multidrug-resistant (MDR) phenotype in paediatric patients is worrisome. Further molecular studies are required to investigate the transmission of drug-resistant genes in E. coli among young communities along with additional surveillance to aid and improve antimicrobial stewardship.
Ethics Approval
This study was in line with the Declaration of Helsinki guidelines and was approved by the Research Ethics of Shenzhen Children’s Hospital (Decision No 2018/03) which complies with global ethical standards.
Consent to Publish
We did not use the patient’s name or personal information; therefore, the Research Ethics Committee of the Shenzhen Children’s Hospital waived the requirement for written consent. In addition, Shenzhen Children’s Hospital collects verbal consent from patients by asking for their permission to use their anonymised data for research purposes.
Funding
This work was supported by Shenzhen Fund for Guangdong Provincial High-Level Clinical Key Specialties (No. SZGSP012); Shenzhen Key Medical Discipline Construction Fund (No. SZXK034).
Disclosure
The authors declare no competing financial or non-financial conflict of interests in this work.
References
1. Ohmagari N, Choi WS, Tang HJ, et al. Targeted literature review of the burden of extraintestinal pathogenic Escherichia Coli among elderly patients in Asia Pacific regions. J Med Econ. 2023;26(1):168–178. doi:10.1080/13696998.2023.2169447
2. Jennifer C, Danielle T, Talia P, Patricia G. CDC yellow book; 2024. Available from: https://wwwnc.cdc.gov/travel/yellowbook/2024/infections-diseases/escherichia-colidiarrheagenic#:~:text=reservoirs%20of%20STEC.-,Epidemiology,certain%20types%20of%20diarrheagenic%20E. Accessed August 18, 2023.
3. Cheung DA, Nicholson A, Butterfield TR, DaCosta M. Prevalence, co-infection and antibiotic resistance of Escherichia Coli from blood and urine samples at a hospital in Jamaica. J Infect Dev Ctries. 2020;14(2):146–152. doi:10.3855/jidc.11361
4. MacKinnon MC, Sargeant JM, Pearl DL, et al. Evaluation of the health and healthcare system burden due to antimicrobial-resistant Escherichia coli infections in humans: a systematic review and meta-analysis. Antimicrob Resist Infect Control. 2020;9(1):200. doi:10.1186/s13756-020-00863-x
5. Rodríguez I, Figueiredo AS, Sousa M, et al. A 21-year survey of Escherichia coli from Bloodstream Infections (BSI) in a tertiary hospital reveals how community-hospital dynamics of B2 phylogroup clones influence local BSI rates. mSphere. 2021;6(6):e0086821. doi:10.1128/msphere.00868-21
6. Zheng B, Chen Y, Violetta L, Xiao Y, Li L. Bloodstream infections caused by Entero-bacteriaceae in China. Lancet Infect Dis. 2019;19(8):810–811. doi:10.1016/S1473-3099(19)30352-4
7. Martinson JNV, Walk ST. Escherichia coli residency in the gut of healthy human adults. EcoSal Plus. 2020;9(1):1. doi:10.1128/ecosalplus.ESP-0003-2020
8. Patil S, Chen X, Lian M, Wen F. Phenotypic and genotypic characterization of multi-drug-resistant Escherichia coli isolates harboring blaCTX-M group extended-spectrum β-lactamases recovered from pediatric patients in Shenzhen, southern China. Infect Drug Resist. 2019;12:1325–1332. doi:10.2147/IDR.S199861
9. Nathan C, Cars O. Antibiotic resistance–problems, progress, and prospects. N Engl J Med. 2014;371(19):1761–1763. doi:10.1056/NEJMp1408040
10. Low M, Neuberger A, Hooton TM, et al. Association between urinary community-acquired fluoroquinolone-resistant Escherichia coli and neighbourhood antibiotic consumption: a population-based case-control study. Lancet Infect Dis. 2019;19(4):419–428. doi:10.1016/S1473-3099(18)30676-5
11. Peng Z, Wang Y, Jia L, Jiang Y, Li X. A 12-year retrospective analysis of blood culture isolates in the intensive care unit of a tertiary hospital in China. Clin Lab. 2023;69(1). doi:10.7754/Clin.Lab.2022.220223
12. Hu F, Yuan L, Yang Y, et al. A multicenter investigation of 2773 cases of bloodstream infections based on China antimicrobial surveillance network (CHINET). Front Cell Infect Microbiol. 2022;12:1075185. doi:10.3389/fcimb.2022.1075185
13. Vihta KD, Stoesser N, Llewelyn MJ, et al. Trends over time in Escherichia coli bloodstream infections, urinary tract infections, and antibiotic susceptibilities in Oxfordshire, UK, 1998–2016: a study of electronic health records. Lancet Infect Dis. 2018;18(10):1138–1149. doi:10.1016/S1473-3099(18)30353-0
14. Koo A, Li C, Liu L, et al. Successful adaptation of fever and neutropenia clinical practice guideline in China. Appl Cancer Res. 2017;37:40. doi:10.1186/s41241-017-0047-3
15. EUCAT, The European Committee on Antimicrobial Susceptibility Testing (EUCAST). Breakpoint tables for interpretation of MICs and zone diameters. Version 9.0; 2019. Available from: http://www.eucast.org. Accessed August 21, 2019.
16. CLSI. Clinical and Laboratory Standards Institute (CLSI) methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically. CLSI standard M07. 10. Wayne: CLSI; 2015.
17. Gardp.org-Global Antibiotic Research. Partnering to Save Lives. Available from: https://revive.gardp.org/resource/multidrug-resistant-mdr/?cf=encyclopaedia. Accessed August 18, 2023.
18. Patil S, Liu X, Chen H, Francisco NM, Wen F, Chen Y. Genetic characterization of colistin-resistant Salmonella enterica ST34 Co-harbouring plasmid-borne mcr-1, blaCTX-M-15 and blaKPC-2 recovered from a paediatric patient in Shenzhen, China. Infect Drug Resist. 2022;15:757–763. doi:10.2147/IDR.S349585
19. O’Hara CM, Tenover FC, Miller JM. Parallel comparison of accuracy of API 20E, Vitek GNI, MicroScan walk/away rapid ID, and Becton Dickinson cobas micro ID-E/NF for identification of members of the family Enterobacteriaceae and common gram-negative, non-glucose-fermenting bacilli. J Clin Microbiol. 1993;31(12):3165–3169. doi:10.1128/jcm.31.12.3165-3169.1993
20. Karn M, Bhargava D, Dhungel B, Banjara MR, Rijal KR, Ghimire P. The burden and characteristics of nosocomial infections in an intensive care unit: a cross-sectional study of clinical and nonclinical samples at a tertiary hospital of Nepal. Int. J Crit Illn Inj Sci. 2021;11(4):236–245. doi:10.4103/ijciis.ijciis_7_21
21. Mohus RM, Gustad LT, Furberg AS, et al. Explaining sex differences in risk of bloodstream infections using mediation analysis in the population-based HUNT study in Norway. Sci Rep. 2022;12(1):8436. doi:10.1038/s41598-022-12569-8
22. Gu J, Chen X, Yang Z, Bai Y, Zhang X. Gender differences in the microbial spectrum and antibiotic sensitivity of uropathogens isolated from patients with urinary stones. J Clin Lab Anal. 2022;36(1):e24155. doi:10.1002/jcla.24155
23. Leung AKC, Wong AHC, Leung AAM, Hon KL. Urinary Tract Infection in Children. Recent Pat Inflamm Allergy Drug Discov. 2019;13(1):2–18. doi:10.2174/1872213X13666181228154940
24. Mattoo TK, Shaikh N, Nelson CP. Contemporary management of urinary tract infection in children. Pediatrics. 2021;147(2):e2020012138. doi:10.1542/peds.2020-012138
25. Renko M, Salo J, Ekstrand M, et al. Meta-analysis of the risk factors for urinary tract infection in children. Pediatr Infect Dis J. 2022;41(10):787–792. doi:10.1097/INF.0000000000003628
26. Djuikoue CI, Djouela Djoulako PD, Wouambo RK, et al. Prevalence of Escherichia coli producing Extended Spectrum Beta-Lactamase (ESBL) driven septicaemia in children aged 0–2 years in two districts hospitals in Yaounde, Cameroon. Bacteria. 2022;1(4):294–301. doi:10.3390/bacteria1040022
27. Helwig H. Contemporary issues in the management of pediatric infections. Pediatr Infect Dis J. 1997;16(3 Suppl):S39–S42. doi:10.1097/00006454-199703001-00003
28. World Health Organization. Report signals increasing resistance to antibiotics in bacterial infections in humans and need for better data. Available from: https://www.who.int/news/item/09-12-2022-report-signals-increasing-resistance-to-antibiotics-in-bacterial-infections-in-humans-and-need-for-better-data. Accessed August 18, 2023.
29. Katip W, Yoodee J, Uitrakul S, Oberdorfer P. Efficacy of loading dose colistin versus carbapenems for treatment of extended spectrum beta lactamase producing Enterobacteriaceae. Sci Rep. 2021;11(1):18. doi:10.1038/s41598-020-78098-4
30. Katip W, Rayanakorn A, Oberdorfer P, Taruangsri P, Nampuan T. Short versus long course of colistin treatment for carbapenem-resistant A. baumannii in critically ill patients: a propensity score matching study. J Infect Public Health. 2023;16(8):1249–1255. doi:10.1016/j.jiph.2023.05.024
31. Farhan SM, El-Baky RMA, Abdalla S, et al. In vitro and in vivo effect of amikacin and imipenem combinations against multidrug-resistant E. coli. Trop Med Infect Dis. 2022;7(10):281. doi:10.3390/tropicalmed7100281