Adenomyosis, Diagnosis, Endometriosis, Health Care, Medical Care, Pain, Symptoms
Adenomyosis vs. Endometriosis: What’s the Difference?
Both conditions can cause pelvic pain and impact fertility.
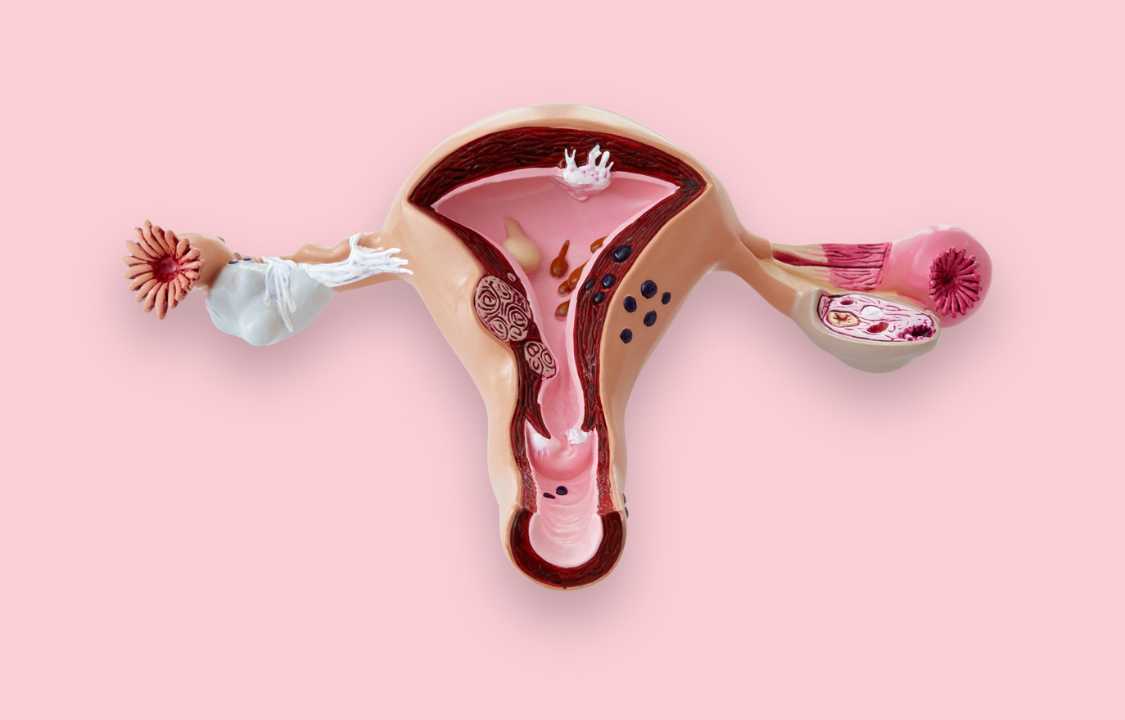
Adenomyosis and endometriosis are distinct medical conditions contributing to pelvic discomfort. Despite the shared symptom of pelvic pain, they diverge in terms of their underlying characteristics. These variations pertain to the specific patterns of growth exhibited by endometrial tissue—lining of the uterus—and the particular regions within the female reproductive system that these disorders affect.
Adenomyosis vs. Endometriosis
When an individual encounters distressing symptoms such as painful menstrual cycles, excessive bleeding, and persistent pelvic discomfort, these combined indicators could potentially point towards endometriosis. This medical condition involves the anomalous dispersion of endometrial tissue, extending and attaching itself beyond the confines of the uterus. During menstruation, this displaced endometrial tissue can expel blood into regions within and outside the pelvic cavity, leading to the gradual formation of cysts, scarring, and adhesions, as outlined by Johns Hopkins Medicine.
In contrast, if the endometrial tissue infiltrates deeply into the uterine muscle rather than migrating beyond the uterus itself, the diagnosis aligns with adenomyosis—a condition closely related to endometriosis, yet exhibiting distinct differences.
In cases of endometriosis, the endometrial tissue escapes the uterus and may establish itself on various external surfaces such as the bladder, bowels, or other organs across the body. Conversely, in adenomyosis, the endometrial tissue becomes enmeshed within the myometrium—a smooth muscular layer within the uterus that lies between its inner and outer layers. Once engrafted in this muscular layer, the displaced endometrial tissue undergoes shedding in synchronization with the rest of the endometrium during menstruation, resulting in heightened bleeding, discomfort, and cramping.
Symptoms
“Both disorders can induce discomfort,” stated Sanjay Agarwal, MD, the Director of the Center for Endometriosis Research and Treatment at the University of California, San Diego. Individuals grappling with adenomyosis typically encounter pain aligned with their menstrual cycles, whereas those afflicted with endometriosis might also endure pain during bowel movements and at various junctures within their menstrual cycle.
“In cases of adenomyosis, the primary impact on one’s quality of life manifests as painful menstruation,” elaborated Dr. Agarwal. “This could be attributed to the fact that endometriosis spreads more extensively.”
The manifestation of symptoms for both conditions spans a spectrum—occasionally leaving the disorders asymptomatic. Research suggests that approximately one-third of women with adenomyosis do not experience any noticeable symptoms, as highlighted in an Obstetrical and Gynecological Survey publication.
Similar observations extend to endometriosis, as stated in an August 2021 study featured in Reproductive Biomedicine & Society Online: “The presentation varies among different women. Some individuals encounter recurring monthly pelvic pain and profuse bleeding, others confront fertility complications, while some remain entirely symptom-free.”
Diagnosing
While an increasing number of healthcare practitioners are adopting a symptom-based approach to address endometriosis, primarily concerning pelvic pain and painful menstruation, the most definitive confirmation of this condition arises from a surgical procedure known as laparoscopy. In the course of a laparoscopy, a thin tube equipped with a light and camera is delicately introduced through a small incision in the abdominal region. This specialized instrument, when inserted, enables healthcare experts to visually inspect for endometrial lesions, cysts, and adhesions, which can subsequently be excised if detected.
In comparison, diagnosing adenomyosis is notably less intrusive. According to MedlinePlus, medical professionals can employ magnetic resonance imaging (MRI) to visualize whether the myometrium, the uterine muscle layer, exhibits abnormal thickness—a distinctive indication of the condition. Both MRIs and transvaginal ultrasounds serve as valuable tools in identifying cysts situated within the uterine walls and detecting myometrial texture irregularities. Classification of adenomyosis hinges on the extent of growth: if confined to a few cysts, it’s labeled as focal, while the presence of abnormal myometrial changes throughout the uterus is designated as diffuse adenomyosis.
Infertility Issues
Both these conditions possess the potential to elevate the risk of compromised fertility—characterized by difficulties in either achieving conception or sustaining a pregnancy to full term.
In the context of adenomyosis, the Obstetrical and Gynecological Survey article underscores that embryos could encounter challenges in implanting within an enlarged and firm uterus. Instances of pregnancy loss are also more prevalent in this scenario. Researchers additionally discerned that women afflicted with adenomyosis, who undergo in vitro fertilization (IVF), exhibit twice the miscarriage rate compared to those facing both adenomyosis and endometriosis.
In a January 2021 study published in Reproductive BioMedicine Online, adenomyosis patients undergoing assisted reproductive therapy (ART) for fertility treatment displayed elevated miscarriage rates and reduced rates of clinical pregnancy.
Should interventions such as IVF prove ineffective, healthcare practitioners might recommend a therapeutic regimen known as a gonadotropin-releasing hormone agonist, as delineated in a Human Reproduction Open study. This approach curbs the production of reproductive hormones, encompassing progesterone and estrogen, thereby diminishing the dimensions of the uterine growth.
An alternate avenue involves surgical excision of the growths, referred to as adenomyomas, along with uterine reconstruction. As outlined in a study featured in Fertility and Sterility, these alternative treatments have demonstrated efficacy in enhancing the prospects of spontaneous pregnancy among women afflicted by adenomyosis. Moreover, the drug protocol might bolster the success rate of IVF as well.
However, contingent upon the extent and distribution of the condition, women dealing with extensive adenomyosis might ultimately necessitate a surrogate to carry their pregnancy, as noted by Dr. Agarwal.
Treating Adenomyosis vs. Endometriosis
The treatment strategies for both these conditions share commonalities and escalate in intensity, ranging from the utilization of birth control pills to inhibit the release of reproductive hormones, to surgical interventions encompassing the removal of endometrial cysts, scar tissue, implants, adenomyomas, or even the complete uterus.
Within this spectrum, there exists an array of hormonal medications that women can explore, as highlighted in a BioMed Research International article. These medications aim to lower the production of estrogen, a hormone that exacerbates both adenomyosis and endometriosis. Administered via injections, hormonal IUDs, or oral pills, these drugs have demonstrated efficacy in mitigating menstrual cramps, discomfort during sexual activity, and persistent pelvic pain experienced in both conditions.
If you find yourself grappling with symptoms associated with either of these conditions, your healthcare provider can expertly assess and determine the most suitable treatment approach tailored to your specific circumstances.