Cardiovascular
Aspirin can help prevent a second heart attack, but most don’t take it
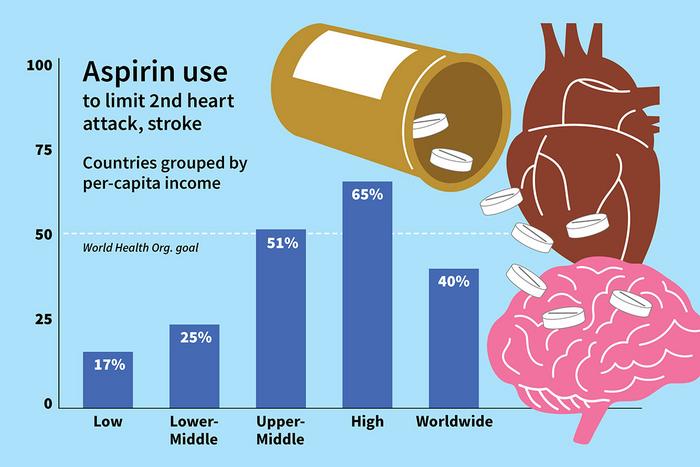
image: Worldwide, only 40% of eligible patients are taking daily aspirin to prevent a second heart attack or stroke, according to a new study led by Washington University School of Medicine in St. Louis. Grouped by per-capita income, the data show that aspirin use is even lower in lower-income countries. The World Health Organization has set a goal of having at least 50% of all eligible people taking daily aspirin by 2025.
view more
Credit: Mike Worful/Washington University School of Medicine
For people who have experienced a heart attack or stroke, taking a daily aspirin has been shown to help prevent a second one. Yet, despite aspirin’s low cost and its clear benefits in such scenarios, fewer than half of people worldwide who have had a heart attack or stroke take the medication, according to a new study led by researchers at Washington University School of Medicine in St. Louis and the University of Michigan.
The study appears Aug. 22 in JAMA.
Cardiovascular disease, including heart attack and stroke, is the leading cause of death globally. Multiple studies conducted in the 1970s and 1980s established that antiplatelet therapy — including aspirin — can reduce the risk of a second cardiovascular event, such as a second heart attack or stroke, by about one-quarter. Since then, daily aspirin has been recommended for this purpose. Daily aspirin therapy is also generally affordable. In the U.S., a monthly supply of baby aspirin (81 milligrams per dose) can cost from $2 to $8, depending on the retailer and the amount purchased.
“Survivors of heart attacks and stroke often face a high risk of having subsequent events,” said first author Sang Gune Yoo, MD, a cardiovascular disease fellow in the Cardiovascular Division at Washington University School of Medicine. “In fact, many people die from having recurring attacks. Aspirin offers one effective and relatively low-cost option for reducing the likelihood of additional events in individuals with established cardiovascular disease, and yet most people who could benefit from a daily aspirin don’t take it.”
According to Yoo, the new study can’t explain why aspirin is so underused, but there likely are multiple intersecting explanations, including varying accessibility to health care in general, inconsistent messaging surrounding use of the drug, and the fact that aspirin is not always available over-the-counter, requiring a prescription in some countries.
Despite the benefits of aspirin, the study showed that in low-income countries, only 16.6% of eligible individuals — those who had experienced a first heart attack or stroke — were taking aspirin to prevent a second heart attack or stroke. In lower-middle-income countries this number was 24.5%. It increased to 51.1% for upper-middle-income countries, and to 65% in high-income countries, including the United States.
Myriad factors contribute to the risk of heart attacks and strokes such as smoking, diabetes, unhealthy diet, genetics, lack of exercise, obesity and even air pollution. Aspirin works as a blood thinner, preventing small blood cells called platelets from forming clots. These clots can block arteries and contribute to a reduction in the amount of oxygen-rich blood being delivered to vital organs. Such blockage also can cause other complications, including a heart attack or stroke.
The researchers, including senior author David Flood, MD, an assistant professor in the Division of Hospital Medicine at the University of Michigan, analyzed data from nationally representative health surveys that were conducted in 51 low-, middle- and high-income countries. The surveys included questions about people’s medical history of cardiovascular disease and on aspirin use. The study included 125,505 individuals, with 10,590 self-reporting a history of cardiovascular disease.
An earlier study that was conducted by a different group of researchers, the Prospective Urban Rural Epidemiology cohort study, was published in 2011 and found similarly low aspirin usage. Despite international efforts to improve access to cardiovascular disease medicines, including aspirin, from 2011 through 2023, aspirin remains severely underused. Yoo said this lack of progress underscores the urgent need to continue developing and implementing interventions to promote aspirin use.
“We might expect that after 10 years there would be more widespread aspirin use, but things haven’t really changed,” Yoo said. “This research deals with a disease process that affects many people, regardless of where you live. We have to remember that this could benefit a tremendous number of people.”
Interventions, according to Yoo, should take a multipronged approach and should consider the contexts in which they’re being implemented. Such approaches could involve repurposing system-level strategies deployed to manage other chronic conditions, such as HIV/AIDS.
“Particularly in lower-middle-income countries, there is often a good infrastructure for caring for patients living with HIV or other endemic disease,” Yoo notes. “We can think about restructuring that so that we can also address comorbidities of heart attack and stroke such as cardiovascular disease as part of those existing systems, instead of having to reinvent the wheel.”
Interventions also could take place where aspirin is easily available, targeting pharmacies or primary care physicians to make the drug more accessible to eligible patients.
“In order to create interventions, we have to understand what is actually going on, which is what we’re trying to establish in this study,” Yoo said. “Then we can start to think about how to develop strategies to increase evidence-based aspirin use in order to save lives.”
###
This work was supported by the National Institutes of Health (NIH), grant numbers K23HL161271, P30DK092926 and 5P30AG024824; and the University of Michigan Caswell Diabetes Institute Clinical Translational Research Scholars Program.
Yoo SGK, et al. Aspirin for secondary prevention of cardiovascular disease in 51 low-, middle-, and high-income countries: a cross-sectional study of nationally representative, individual-level data. JAMA. Aug. 22, 2023.
About Washington University School of Medicine
WashU Medicine is a global leader in academic medicine, including biomedical research, patient care and educational programs with 2,800 faculty. Its National Institutes of Health (NIH) research funding portfolio is the third largest among U.S. medical schools, has grown 52% in the last six years, and, together with institutional investment, WashU Medicine commits well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice is consistently within the top five in the country, with more than 1,800 faculty physicians practicing at 65 locations and who are also the medical staffs of Barnes-Jewish and St. Louis Children’s hospitals of BJC HealthCare. WashU Medicine has a storied history in MD/PhD training, recently dedicated $100 million to scholarships and curriculum renewal for its medical students, and is home to top-notch training programs in every medical subspecialty as well as physical therapy, occupational therapy, and audiology and communications sciences.
Journal
JAMA
Subject of Research
People
Article Title
Aspirin for Secondary Prevention of Cardiovascular Disease in 51 Low-, Middle-, and High-Income Countries
Article Publication Date
22-Aug-2023