Infection
I’m a doctor who specializes in treating leprosy. Here’s what I want you to know
In recent weeks, you may have seen alarming headlines about how leprosy might become “endemic” in Florida. As a physician in Florida who specializes in treating leprosy, also known as Hansen’s disease, this case report was not “news” to us in the field: We have known for some time about endemic cases of leprosy. However, given how rare the disease is in the state, there is no cause for alarm — despite the fearful headline.
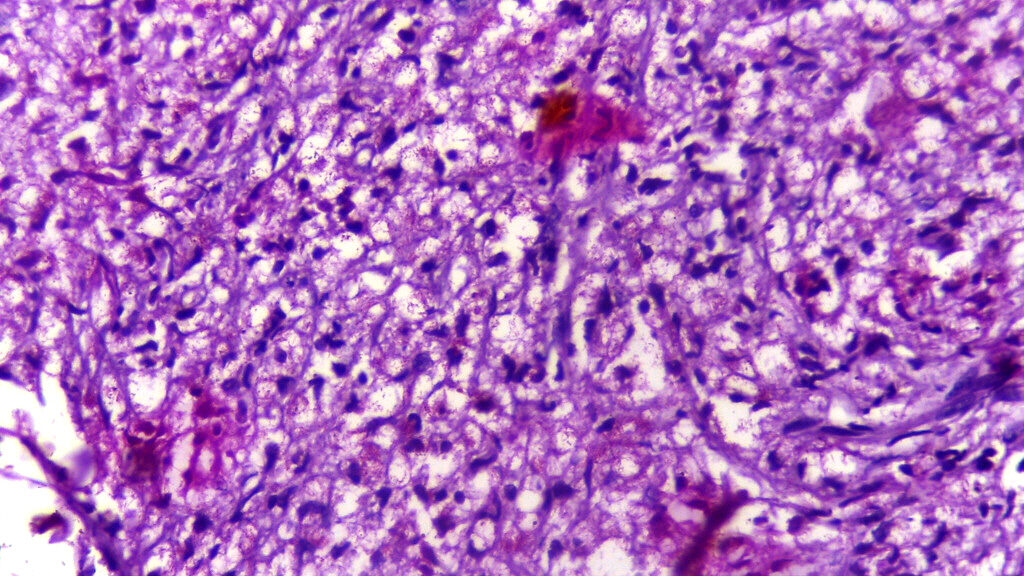
Leprosy is caused by infection with one of the bacteria from the Mycobacterium leprae complex. This organism infects the skin and nerves of affected patients and presents as rashes that often have absent sensation, and can have pain or loss of sensation in the hands and feet. Due to the nerve involvement and subsequent loss of protective sensation, patients with leprosy can burn or injure themselves without even noticing, which can lead to infections and subsequent complications requiring amputation. (Despite the popular misconception, leprosy does not cause spontaneous amputations or loss of skin — like a nose or finger falling off.) Because of these injuries, leprosy causes significant morbidity for patients that are affected and is the leading cause of infectious disability worldwide.
Leprosy remains a significant global health burden, with more than 200,000 cases worldwide in 2019. The prevalence of leprosy is highest in resource-limited settings, such as India, Brazil, Indonesia, Nepal, and Bangladesh, where the organism is considered endemic. Most cases are transmitted through household contacts. In other countries where leprosy is present in lower rates, infection is often acquired abroad.
Despite the rarity of leprosy in the United States, there is a long history of management of these patients, beginning in the late 1800s, when a deserted “Indian Camp Plantation” was used in Carville, Louisiana, as a quarantine site for patients with leprosy. In 1917, the National Leprosarium in this location was established, providing care for patients afflicted with the disease. Currently, the National Hansen’s Disease Program (NHDP) provides care for patients with leprosy through the primary location, now in Baton Rouge, and 16 additional federally funded sites. In 2020, there were 159 new cases in the U.S.
The exact mechanism for the transmission of leprosy is unknown. It is thought to spread through respiratory droplets after prolonged periods of exposure, such as a household contact. It is important to note that spread does not occur by incidental contact.
The other unique feature about this disease is that over 95% of the world’s population is immune to infection. Therefore, most people will never go on to develop disease even if they do come in contact with the bacteria.
Finally, there is potential transmission of leprosy through zoonotic, or animal exposure, sources. This has been established specifically with the 9-banded armadillo, which has been confirmed to be a source. This armadillo is found in the southeastern and south central United States, as well as Central and South America. Its location in the U.S. correlates with the places where leprosy is found, including my home state of Florida.
The recent discussion about Florida potentially becoming a site for endemic leprosy in the U.S. began with a research letter published in Emerging Infectious Diseases. The report described a case of leprosy in central Florida in which the patient had no previous international travel or known zoonotic exposure (such as to the 9-banded armadillo). Given the higher prevalence of leprosy in central Florida as compared with other parts of the state and the country, the article concluded that leprosy may be endemic in Florida and travel to the state should be considered when performing contact tracing.
The majority of cases of leprosy seen in the United States are acquired internationally, with 75% of cases diagnosed in the United States in 2020 occurring among immigrants. However, as the director for the University of Miami/Jackson Memorial Hospital Hansen’s Disease Clinic, the only NHDP clinic in Florida, I see many of the cases being diagnosed throughout the state. For some time, my colleagues and I have seen cases in people who haven’t traveled internationally or otherwise have an easy explanation for their infection. In some of these cases, the patients do report having been exposed to 9-banded armadillos. But in others, they do not report any direct contact. The potential source of transmission is unclear and is still being studied.
So I am glad to see that there is more attention being paid here. But I want to be clear: Though we are not sure on the method of acquisition of the infection in some patients in Florida and do not have obvious sources of exposure, the overall number of cases in Florida is very low. In 2020, the last year for which data is available, there were just 27.
Additionally, again, leprosy is not a highly contagious disease, as the majority (>95%) of the population is immune to infection with the organism, and will never develop disease. Acquisition of the disease in someone who is genetically susceptible to the infection requires prolonged contact (such as a same household contact), and therefore, one cannot catch leprosy by walking near someone with the disease.
Finally, leprosy is also a very treatable disease, and with the initiation of antibiotic therapy, curable in over 99% of patients without recurrence, though some may have long-lasting disabilities or immune diseases after they complete antibiotic therapy.
Therefore, despite the occurrence of these locally acquired cases in Florida, the risk of acquiring leprosy in Florida remains exceedingly rare.
But the recent article does highlight the need for additional education on the disease for both the public and health care providers to better identify the early symptoms of leprosy and institute therapy as soon as possible to prevent disability.
One of the benefits of the increased attention on leprosy is the opportunity to improve people’s understanding of the disease. After the article was released, I received many worried texts and calls. Despite none of these people ever knowing someone affected with leprosy, they have strong presumptions about the disease.
And unfortunately, while much of what people believe about the disease is completely untrue, these false beliefs negatively affect the lives of patients with leprosy. This occurs worldwide, where the skin discoloration of one standard medication taken for leprosy is so stigmatizing that on the label it warns about depression and suicide risk because of this side effect.
Stigma occurs here in the U.S. as well. My patients with leprosy tell me that when they are admitted to the hospital for non-leprosy related medical events, they are treated as if they have the plague and approached with caution. This is not right. But with increased understanding of this disease, we can help remediate that.
And hopefully, the increased attention will lead to more funding and research into this area. Leprosy disproportionately affects resource-limited settings, and development of new therapeutics for the management has been slow because of lack of investment. Increased funding for research both within the United States and abroad will help to improve the lives of all patients and minimize disability in the future.
Andrea Maderal, M.D., is the director for the University of Miami/Jackson Memorial Hospital Hansen’s Disease Clinic.