Cardiovascular
Inhaler combination outperforms others in reducing COPD exacerbation, cardiovascular risks
August 23, 2023
3 min read
Source/Disclosures
Disclosures:
The study authors report no relevant financial disclosures. Blagev reports no relevant financial disclosures.
Key takeaways:
- Outcomes may vary among different fixed-dose combination inhalers for COPD.
- Fewer severe acute exacerbations occurred with glycopyrronium/indacaterol or umeclidinium/vilanterol vs. tiotropium/olodaterol.
Glycopyrronium/indacaterol reduced the likelihood for severe acute exacerbations and cardiovascular events compared with tiotropium/olodaterol among patients with COPD, according to study results published in CHEST.
Like glycopyrronium/indacaterol (Ultibro Breezhaler, Novartis), umeclidinium/vilanterol (Anoro Ellipta; GlaxoSmithKline) also reduced exacerbation risk but showed comparable cardiovascular event risk as tiotropium/olodaterol (Stiolto Respimat; Boehringer Ingelheim).
“This study provides further evidence of differences among [long-acting muscarinic antagonist]/[long-acting beta agonists] fixed-dose combinations to facilitate informed decision-making in clinical practice.” Ching-Fu Weng, MD, PhD, of the division of pulmonary medicine at Cathay General Hospital in Taipei, Taiwan, and colleagues wrote.
In a retrospective cohort study, Weng and colleagues evaluated 44,498 adults with COPD and a new prescription to one of three fixed-dose combinations of LAMAs and LABAs between January 2015 and June 2019.
The fixed-dose combinations included glycopyrronium/indacaterol (GLY/IND; n = 15,586), umeclidinium/vilanterol (UMEC/VI; n = 20,460) or tiotropium/olodaterol (TIO/OLO; n = 8,452).
Researchers propensity score matched the adults either 1:1 (in the case of comparing UMEC/VI to GLY/IND) or 2:1 (in the case of comparing UMEC/VI to TIO/OLO and GLY/IND to TIO/OLO) and assessed the risk for acute exacerbations and cardiovascular events between treatment groups using Cox regression models.
When comparing UMEC/VI against TIO/OLO, researchers found fewer and decreased risk for severe acute exacerbations with the combination of UMEC/VI (17.85 vs. 29.32 per 100 person-years; HR = 0.76; 95% CI, 0.68-0.84). When divided by age, only those aged 65 years or older demonstrated this risk difference (HR = 0.74; 95% CI, 0.65-0.83 vs. < 65 years, HR = 0.96; 95% CI, 0.75-1.22).
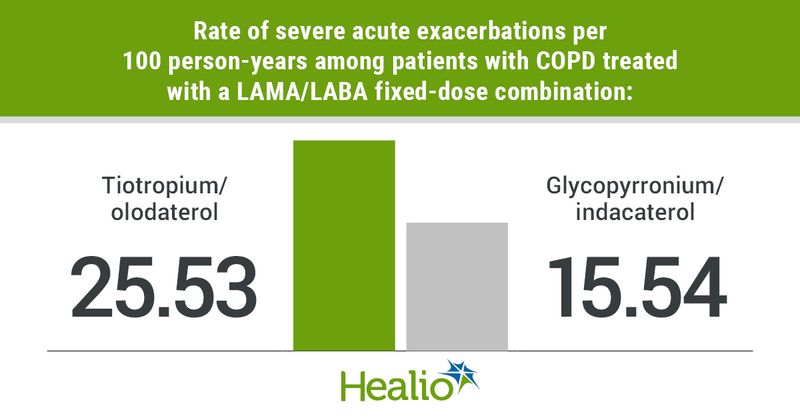
Comparing GLY/IND with TIO/OLO showed a similar reduction in severe acute exacerbations (15.54 vs. 25.53 per 100 person-years; HR = 0.77; 95% CI, 0.67-0.88), according to researchers.
Among those receiving UMEC/VI and those receiving GLY/IND, researchers found comparable incidence rates and likelihoods for an acute exacerbation.
These findings persisted in sensitivity analyses that used severe acute exacerbations and pneumonia events as the outcome, restricted the follow-up period and used the intention-to-treat analytical approach. However, the differences compared with TIO/OLO lessened when researchers used both severe and moderate acute exacerbations as the outcome.
In the assessment of cardiovascular events, patients receiving UMEC/VI vs. GLY/IND and those receiving UMEC/VI vs. TIO/OLO showed comparable outcomes, according to researchers.
However, researchers observed fewer cardiovascular events with GLY/IND vs. TIO/OLO (2.49 vs. 4.28 events per 100 person-years; HR = 0.7; 95% CI, 0.51-0.95). Notably, this finding did not persist on sensitivity analysis that limited follow-up to 6 months or less.
“The findings need to be verified in further research, and large-scale prospective studies are necessary to establish more robust evidence,” Weng and colleagues wrote.
Although more evidence is needed to support these results, this study by Weng and colleagues emphasizes the significance of identifying differences between LAMA/LABA inhalers, according to an accompanying editorial by Denitza P. Blagev, MD, associate professor in the department of medicine at The University of Utah and chief medical officer at Riverton Hospital at Intermountain Healthcare.
“On the surface these differences among LAMA/LABA combination inhalers seem trivial, surely hardly something to get excited about when prescribing to an individual, especially if there is a difference in cost or another reason to prefer one inhaler over another,” Blagev wrote. “On the other hand, when we look at these seemingly small differences over the number of people who take these medications worldwide, not only is the potential impact of such differences in efficacy and risk huge, but also it is shameful that with that many people’s lives at stake and that much money spent in this market, we have little certainty or high-quality data on which to base these decisions.”