Infection
Who should get the new RSV vaccines? Here’s everything you need to know
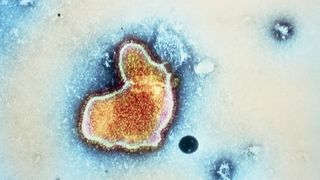
Respiratory syncytial virus, or RSV, is a common respiratory virus that spreads seasonally. A new drug and several vaccines that prevent the infection have recently come to market.
Here’s what you need to know about the three new shots — two vaccines and one injectable drug — that were recently approved by the Food and Drug Administration (FDA) to fight RSV.
Related: What does it mean for a disease to be ‘endemic’?
How serious is RSV?
Most people who contract RSV develop only cold-like symptoms, like a runny nose, decreased appetite, coughing and sneezing. Mild infections usually resolve without medical treatment. However, RSV can be severe and potentially fatal in infants, young children and older adults.
RSV season typically runs from fall to spring, although its timing has been disrupted in recent years due to the COVID-19 pandemic. Every year in the U.S., the virus leads to approximately 2.1 million doctor’s visits among children younger than 5 and about 58,000 to 80,000 hospitalizations in the same age group, the CDC estimates. It’s the most common cause of hospitalization in infants, and annually, 100 to 300 children under 5 die from the infection in the U.S.
The children at highest risk include premature babies, infants, children under age 2 who were born with heart disease or have chronic lung disease, and children with weakened immune systems or neuromuscular disorders.
Among adults ages 65 and older, RSV leads to 60,000 to 160,000 hospitalizations each year and about 6,000 to 10,000 deaths in the U.S. Older adults at the highest risk include those with chronic heart or lung disease, those with weakened immune systems, and those living in nursing homes or long-term care facilities. RSV infections in this age group can also worsen existing conditions, like chronic obstructive pulmonary disease (COPD) and congestive heart failure.
Is there a vaccine for RSV?
Yes, there are two FDA-approved vaccines for RSV — one for older adults, and one for both older adults and pregnant people.
The FDA approved the first-ever RSV vaccine in May 2023. The shot, called Arexvy and made by the pharmaceutical company GSK, is approved for adults ages 60 and older.
The vaccine contains an adjuvant, a substance that revs up the immune system, and a lab-made version of a protein found on the surface of the virus. The virus uses this fusion, or “F” protein, to break into cells. The shot trains the immune system to recognize what the F protein looks like in its “prefusion” form, the shape it’s in before it infects cells.
The second RSV vaccine approved by the FDA is called Abrysvo. Made by Pfizer, the shot was approved for older adults in May 2023 and for pregnant people in August 2023. Like Arexvy, Abrysvo contains lab-made perfusion F proteins. Neither vaccine contains preservatives, according to their drug labels .
How effective are the RSV vaccines?
In older adults, GSK’s Arexvy and Pfizer’s Abrysvo offer similar protection against RSV-associated “lower respiratory tract disease” (LRTD), meaning infections that affect the lungs.
In the first RSV season after vaccination, GSK’s Arexvy lowers the chance of RSV-related LRTD by 82.6% and the risk of having to see a doctor for LRTD by 87.5%. A year after receiving one dose of vaccine, participants entered their second RSV season post-vaccination; data collected at that time showed that the shot was still 56.1% effective at preventing LRTD.
By comparison, in the first RSV season, Pfizer’s Abrysvo is 88.9% protective against LRTD and 84.6% effective at preventing doctor’s visits for LRTD. It’s 78.6% protective against LRTD in the second season, based on data from part of a subsequent season, according to a Morbidity and Mortality Weekly Report (MMWR) from the CDC.
When given in pregnancy, Abrysvo protects newborns by providing them with anti-RSV antibodies that cross the placenta and likely also crop up in breast milk. Abrysvo is specifically approved for use between week 32 and 36 of pregnancy; in clinical trials, this timing resulted in the most protection for newborns. The babies’ LRTD risk was slashed by 91.1% within 90 days of birth and by 76.5% within 180 days.
Who should get an RSV vaccine?
Adults ages 60 and older can get one dose of one of these RSV vaccines after discussing it with their doctor, the CDC says.
“The decision to vaccinate an individual patient should be based on a discussion between the healthcare provider and the patient,” the CDC states. “It may be informed by the patient’s risk of severe RSV disease and their characteristics, values, and preferences; the healthcare provider’s clinical discretion; and the characteristics of the vaccine.”
The CDC doesn’t say all older adults should get the shot, and instead recommends parsing risks and benefits of the shot with a doctor. That’s partly because six cases of “inflammatory neurologic events” were reported in clinical trials of the vaccines. These included cases of Guillain-Barré syndrome, a condition in which the immune system attacks the nerves, and acute disseminated encephalomyelitis, which causes swelling in the brain and spinal cord, according to the CDC’s MMWR.
Still, both RSV vaccines were deemed very safe in clinical trials with tens of thousands of people, and their most common side effects were mild. Given how few people experienced the inflammatory neurologic events, it’s currently unclear if these conditions occurred by chance or if the shots somehow raised their likelihood.
“Until additional evidence becomes available from postmarketing surveillance clarifying the existence of any potential risk, RSV vaccination in older adults should be targeted to those who are at highest risk for severe RSV disease and therefore most likely to benefit from vaccination,” the MMWR states.
As of Aug. 23, the CDC had not issued an official recommendation about the use of Abrysvo in pregnancy; an advisory committee is expected to discuss the topic in October. The vaccine will be made publicly available after this guidance is issued, NBC reported.

Do you get vaccinated for RSV as a child?
No. There is no approved RSV vaccine for children.
However, newborns will get indirect protection in their early months of life if their parents receive an RSV vaccine during pregnancy. However, this protection comes from RSV-fighting antibodies that pass through the placenta. The shot doesn’t result in a permanent “memory” of RSV in the child’s immune system, like a vaccine given in childhood would.
Is there a drug to prevent RSV in children?
Yes, there are two antibody-based drugs available to protect infants from RSV.
Note that, at this time, the CDC has not issued guidance about whether it would be better for pregnant people to get the new prenatal RSV vaccine during pregnancy, or to wait until after birth to give their baby an antibody drug. (This article will be updated when there is guidance available.)
In August 2023, the FDA approved a drug called Beyfortus (generic name nirsevimab-alip). The shot contains lab-made proteins that mimic antibodies made by the immune system. Called a monoclonal antibody, this type of drug doesn’t train a child’s immune system to make its own RSV-fighting antibodies, like a vaccine would. Instead it provides a ready-made supply.
All infants younger than 8 months who are born during, or are just entering, their first RSV season should get a shot of Beyfortus, according to the CDC. Some children between the ages of 8 months and 19 months who are at increased risk of severe RSV, including those with weakened immune systems, should also get a shot for their second RSV season.
The one-time shot protects children for about five months, the length of an average RSV season, the CDC states.
An older antibody shot against RSV, called Synagis (generic name palivizumab), was first approved in 1998. However, only children at the highest risk of severe disease, not healthy children, should be given that one, the CDC recommends.
“Palivizumab is limited to children under 24 months of age with certain conditions that place them at high risk for severe RSV disease,” the CDC states. “It must be given once a month during RSV season.”
For example, Synagis is recommended for premature babies, especially those with chronic lung disease, and infants with certain heart diseases. This limited usage is partly due to the drug’s high cost and the fact that it requires at least one and up to five shots a month during RSV season.
This article is for informational purposes only and is not meant to offer medical advice.