Cardiovascular
Cardiovascular prognosis of subclinical COPD
Eduardo José Pereira Ferreira,1– 4 Lucas Villar Shan de Carvalho Cardoso,3,5 Carlos José Oliveira de Matos,6 Igor Larchert Mota,3,4 Juliana Maria Chianca Lira,3,5 Mayara Evelyn Gomes Lopes,3,5 Giulia Vieira Santos,3,5 Maria Luiza Dória Almeida,2,3,5 Manuel Herminio Aguiar-Oliveira,2,3,5 Antônio Carlos Sobral Sousa,2– 5 Enaldo Vieira de Melo,3,5 Joselina Luzia Menezes Oliveira2– 5
1Department of Medicine, Federal University of Sergipe, Lagarto, 49400-000, Brazil; 2Postgraduate Program in Health Sciences, Federal University of Sergipe, Aracaju, 49100-000, Brazil; 3University Hospital, Federal University of Sergipe, Aracaju, 49100-000, Brazil; 4São Lucas Clinic and Hospital- Rede D’Or São Luiz, Aracaju, 49060-676, Brazil; 5Department of Medicine, Federal University of Sergipe, Aracaju, 49100-000, Brazil; 6Department of Physiotherapy, Federal University of Sergipe, Lagarto, 49400-000, Brazil
Correspondence: Eduardo José Pereira Ferreira, Federal University of Sergipe, Avenida Marechal Rondon, s/n- Jardim Rosa Elze, São Cristóvão, Sergipe, 49100-000, Brazil, Tel + 55 79 999319810, Email [email protected]
Background: Chronic obstructive pulmonary disease (COPD) worsens prognosis in patients with coronary artery disease (CAD). However, the cardiovascular prognosis in patients with stable or mildly symptomatic COPD remains unclear. Here, we sought to determine the long-term cardiovascular events in patients with subclinical or early-stage COPD with concomitant CAD.
Methods: This was a longitudinal analytical study involving 117 patients with suspected or established CAD who underwent assessment of pulmonary function by spirometry and who were followed up for six years (March 2015–January 2021). The patients were divided into two groups, one comprising COPD (n=44) and the other non-COPD (n=73) patients. Cox regression was used to evaluate the association between COPD and cardiovascular events, with adjustment for the established CAD risk factors, and the effect size was measured by the Cohen test.
Results: COPD patients were older (p=0.028), had a greater frequency of diabetes (p=0.026), were more likely to be smokers (p 0.001), and had higher modified Medical Research Council scores (p 0.001). There was no difference between the groups regarding gender, body mass index, hypertension, dyslipidemia, family history of CAD, and type of angina. CAD frequency and the proportion of patients with severe and multivessel CAD were significantly higher among COPD than among non-COPD patients (all p 0.001). At six-year follow-up, patients with COPD were more likely to have experienced adverse cardiovascular events than those without COPD (p 0.001; effect size, 0.720). After adjusting for established CAD risk factors, COPD occurrence remained an independent predictor for long-term adverse cardiovascular events (OR: 5.13; 95% CI: 2.29– 11.50; p 0.0001).
Conclusion: COPD was associated with increased severity of coronary lesions and a greater number of adverse cardiovascular events in patients with suspected or confirmed CAD. COPD remained a predictor of long-term cardiovascular events in stable patients with subclinical or early-stage of COPD, independently of the established CAD risk factors.
Keywords: COPD, coronary artery disease, risk factors, ischemic heart disease, myocardial infarction
Introduction
Despite being preventable and treatable, chronic obstructive pulmonary disease (COPD) is the third leading cause of death worldwide and the fourth leading cause of death in Brazil.1–3 This is mainly due to the chronic systemic inflammatory response induced by COPD and its promotive and aggravating effect on conditions such as pulmonary hypertension, lung cancer, and cardiovascular diseases (CVD).4–6
COPD is a risk factor for the development of coronary artery disease (CAD) independently of other cardiovascular risk factors and its occurrence worsens prognosis in patients with CAD.7,8 Excess or chronic inflammation can result in damage to the pulmonary and cardiovascular systems. The inflammatory environment is characterized by the recruitment of inflammation-associated immune cells, which further increases the inflammatory response, leading to atherosclerosis, increased platelet activation, thrombosis, and the accelerated evolution and ultimate rupture of vascular plaques.9–11 The shared risk factors between COPD and CAD, such as smoking and pulmonary malfunction, can further heighten the inflammatory response. Smoking disrupts the lipid profile, making it more atherogenic, thereby inducing changes in platelet function and causing endothelial damage. Lung malfunction, in turn, is associated with an increased risk for diabetes, hypertension, stroke, and CVD.12 Moreover, studies have shown that the prevalence of these comorbidities increases with the severity of the disease as well as the extent of COPD exacerbation.13
Despite being underdiagnosed, COPD is common in patients with CAD. Indeed, airflow limitation is not detected in 60% to 87% of patients with ischemic heart disease. The rates of underdiagnosis are even higher among former smokers, mildly symptomatic individuals, and patients with mild airflow limitation. Conversely, COPD is incorrectly diagnosed in a small proportion of CAD patients. This inaccuracy may be explained by the overlap in the clinical presentation of the two diseases, such as breathlessness and chest pain, which results in the lack of a second diagnosis once one has already been made.10,14,15
Large population-based studies have demonstrated that patients with COPD are at increased risk for cardiovascular events and associated mortality, particularly following COPD exacerbation, hospitalization, acute coronary syndrome, and cardiac revascularization.16,17 However, the cardiovascular prognosis of patients with mild/moderate or stable COPD remains unclear. Thus, the objective of this study was to assess the long-term cardiovascular events in patients with subclinical COPD or those in the initial stages of the disease with a concomitant diagnosis of CAD.
Methods
Study Design and Population
This was a longitudinal and analytical study, carried out from March 2015 to January 2021, involving a cohort of 117 patients with suspected or established CAD who underwent assessment of pulmonary function by spirometry and who were subsequently followed up for six years. These patients were referred by their physician for the evaluation of myocardial ischemia using the ergometric test or exercise stress echocardiography. At the time of the noninvasive cardiac test, spirometry was performed for all the patients (COPD or non-COPD). The inclusion criteria were patients older than 40 years who had stable cardiac and pulmonary disease (ie, those who did not present with clinical evidence of acute coronary syndrome, heart failure, respiratory infection, or recent hospitalization) at least eight weeks before data collection. The exclusion criteria were patients with a previous diagnosis of COPD, asthma or reversible obstruction, allergy, hyperreactivity, occupational lung disease, or sequelae of pulmonary pathologies such as tuberculosis or pulmonary fibrosis. Informed consent was obtained from all the participants and the study protocol was approved by the Research Ethics Committee of the Federal University of Sergipe as well as the local ethics committee of each participating institution and complies with the Declaration of Helsinki.
Demographic and Clinical Characteristics
Demographic and clinical data were collected via a structured case report form and included age, gender, weight, height, cardiovascular risk factors (such as diabetes, hypertension, dyslipidemia, family history of CAD), life habits, the medication used, actual symptoms, and assessment of limitation in activities of daily living imposed by dyspnea according to modified Medical Research Council (mMRC) criteria.18,19
Diagnosis of COPD
The diagnosis of COPD was established by spirometry, which was performed for all participants according to American Thoracic Society performance criteria.20 A post-bronchodilator ratio of forced expiratory volume in 1s (FEV1) to forced vital capacity (FVC) of less than 70% of the predicted value confirmed the presence of persistent airflow limitation, which was compatible with COPD diagnosis.21 COPD severity was evaluated following GOLD recommendations and the patients were categorized into four severity classes (GOLD I–IV) according to spirometric criteria.22
Diagnosis of CAD
All the patients included in this study had either suspected CAD based on a medical history of angina and/or inducible myocardial ischemia in the stress test (ergometric test or exercise stress echocardiography) or confirmed CAD with evidence of coronary atherosclerotic lesions by coronary computed tomography angiography or invasive coronary angiography.23 Among patients with known coronary anatomy, CAD was classified according to the degree of stenosis, severity, and extent of coronary lesions. Non-obstructive CAD was defined by the detection of lesions with a degree of luminal stenosis of less than 50%; the criterium for obstructive CAD was a degree of luminal stenosis of 50% or more in at least one of the coronary arteries. Meanwhile, CAD severity was graded according to the degree of luminal obstruction, as follows: discrete CAD, lesions with a degree of stenosis of less than 39%; moderate CAD, lesions with a degree of stenosis of 40% to 69%; and severe CAD, lesions with a degree of stenosis of 70% or more in at least one coronary segment. The criteria for determining the extent of CAD were based on the number of affected major epicardial vessels and the detection of disease in the left main coronary artery. Thus, the extent of CAD was classified as univessel, bivessel, trivessel, or left main CAD. The multivessel pattern represents obstructive CAD in two or more major epicardial vessels, including or not the left main coronary artery.24,25
Follow-Up and Adverse Cardiovascular Events
During the six years of follow-up, the patients were monitored for adverse cardiovascular events, including the need for invasive coronary angiography, cardiac revascularization, myocardial infarction, cardiac hospitalization, and cardiac death. The decision for invasive coronary angiography was taken by the patient’s cardiologist or, in an emergency, by the attending physician, according to standard clinical practice. Cardiac revascularization was described as any clinically driven revascularization event, including percutaneous coronary intervention (PCI) or bypass surgery. The diagnosis of myocardial infarction was defined as new Q waves, new persistent ST-segment or T-wave changes, or elevated troponin levels. Cardiac hospitalization was described as any hospitalization in which a suspected diagnosis of cardiac disorder was the primary reason for admission. Finally, cardiac death was diagnosed as an unexplained death without an identifiable non-cardiac cause.26,27
Statistical Analysis
Continuous variables were expressed as means ± standard deviation. The Kolmogorov–Smirnov test was applied to evaluate the normality of distribution. According to the normality of the sample, the Student’s t-test or the Mann–Whitney test was used for independent groups. For categorical variables, the results are presented as absolute frequency or percentage; the chi-square test or Fisher’s exact test was employed for comparisons between the two groups, as appropriate. The Kaplan–Meier method was used to estimate adverse cardiovascular event-free survival and the Log rank test was used to test the differences between the groups. Cox regression was used to assess the association between COPD and the occurrence of combined adverse cardiovascular events, adjusting for the variables age, gender, diabetes, hypertension, and dyslipidemia. The effect size was measured by the Cohen test and Cohen’s h was categorized as a small (<0.25), medium (0.25<0.50), or large (≥0.50) effect size, based on benchmarks suggested by Cohen.28 Statistical analyses were performed using SPSS for Windows, version 26 (IBM Corporation, Armonk, NY, USA) and WINPEPI, version 11.65 (Copyright J.H Abramson, 23 August 2016). A p-value <0.05 was considered significant and the statistical power was 0.80 or higher.
Results
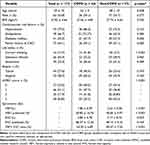
The demographic, clinical and spirometric data of all the patients (with or without COPD) are shown in Table 1. Patients with COPD were older (62 ± 9 vs 58 ± 10 years, p=0.028) and had a higher frequency of diabetes (47.7% vs 27.4%; p=0.026). There was also a greater proportion of current smokers (31.8% vs 2.7%; p<0.001) and higher mMRC scores (p<0.001) among the COPD patients. Additionally, patients with COPD had lower FEV1 and FEV1/FVC ratio (p<0.001) than patients without lung disease. There was no difference between the two groups regarding gender, body mass index, hypertension, dyslipidemia, family history of CAD, and type of angina. In the COPD group, 15 patients (34.1%) had mild lung disease (GOLD I), 23 (52.3%) had moderate disease (GOLD II), and 6 (13.6%) had severe disease (GOLD III). None of the patients had very serious disease (GOLD stage IV).
|
Table 1 Demographic and Clinical Characteristics of Patients with and without COPD |
Information relating to the presence, extent, and severity of CAD, as determined by invasive coronary angiography or coronary computed tomography angiography, is presented in Table 2. CAD frequency was significantly higher in patients with COPD than in those without COPD (90.9% vs 39.7%; p<0.001). Additionally, patients with COPD had a greater number of lesions with a degree of luminal stenosis of 50% or more (65.7% vs 17.8%; p<0.001) and greater proportions of severe CAD (54.5% vs 11.0%; p<0.001) and trivessel CAD (31.8% vs 11.0%; p<0.001) compared with non-COPD patients.
 |
Table 2 Presence, Extent and Severity of CAD in Patients with and without COPD |
At the six-year follow-up, patients with COPD were more likely to have experienced adverse cardiovascular events compared with patients without COPD (52.3% vs 11.0%; p<0.001), with an effect size of 0.720, which was characterized as a large effect. During follow-up, more than one-third of COPD patients underwent invasive coronary angiography (36.4% vs 9.6%; p<0.001). Moreover, the occurrence of myocardial infarction (27.3% vs 6.8%; p=0.002), cardiac revascularization (25.0% vs 5.5%; p=0.002), and cardiac hospitalization (27.3% vs 8.2%; p=0.019) was significantly higher in the COPD group than in the non-COPD group (Table 3). There was one cardiac death in the study population, followed in the COPD group.
 |
Table 3 Adverse Cardiovascular Events at Six-Years Follow-Up in Patients with and without COPD |
The relationship between COPD and adverse cardiovascular events was evaluated using the Kaplan–Meier method. At six-year follow-up, event-free survival was significantly higher in the non-COPD group than in the COPD group (86% vs 40%; p<0.001) (Figure 1). After adjusting for established risk factors for CAD, the presence of COPD remained an independent predictor for long-term adverse cardiovascular events (OR: 5.13, 95% CI: 2.29–11.50; p<0.0001).
|
Figure 1 Kaplan Meier curves of survival free of adverse cardiovascular events in COPD patients and non-COPD patients during six-year follow-up (p < 0.001). |
In the COPD group, there was a higher frequency of long-term adverse cardiovascular events among patients with moderate to severe pulmonary disease (GOLD stages II and III); than among those with mild disease (GOLD I) however, the difference was not significant (Table 4).
 |
Table 4 Adverse Cardiovascular Events at Follow-Up of COPD Patients According GOLD Class |
Discussion
In the present study, we demonstrated that patients with suspected or confirmed CAD and concomitant diagnosis of COPD have an adverse cardiovascular prognosis. The diagnosis of COPD in patients classified as stable or mildly symptomatic and with suspected or confirmed CAD was significantly associated with an increase in the number of long-term cardiovascular events requiring invasive coronary angiography, cardiac revascularization, cardiac hospitalization, and myocardial infarction during follow-up. Patients in the COPD group were older and had a higher frequency of diabetes compared with those in the non-COPD group; however, COPD remained an independent predictor of long-term cardiovascular events even after adjusting for established risk factors for CAD such as age, gender, hypertension, diabetes, and dyslipidemia. Patients with COPD also had a higher frequency of CAD, mainly severe and multivessel, and the more advanced the degree of COPD, the greater the severity of the coronary lesions and the extent of calcification, as previously suggested by us29 and others.30
Epidemiologic studies have identified a strong association between COPD and CAD, leading to the proposition that patients with COPD might be at higher risk of developing CAD and vice versa.31 However, in clinical practice, there is substantial underdiagnosis of COPD among individuals with CAD. In a population-based survey, CAD was reported in only 7% to 13% of patients diagnosed with COPD, and COPD was reported in 26% to 35% of patients with CAD. Studies have reported that persistent airflow limitation is not recognized in 60% to 87% of patients with CAD, especially those who are former smokers or have mild symptoms.14,32 In the present study, the presence of COPD was assessed by spirometry in patients categorized as stable or mildly symptomatic and who had not previously been diagnosed with COPD during routine and non-invasive investigation for myocardial ischemia by exercise stress echocardiography. Among the 117 patients, 44 (37%) were diagnosed with COPD, 86% of which exhibited mild or moderate airflow limitation and were classified as having COPD GOLD stage I or II.
Our results suggested the existence of inherent and reciprocal influences between COPD and CAD. Although the shared underlying pathogenic mechanisms are not fully understood, chronic and systemic inflammation, which affects both cardiovascular endothelial cells and the lung parenchyma, has been proposed to be the main causative factor in both diseases. Several studies have shown that patients with stable COPD and comorbid CAD have higher levels of inflammatory markers, including C-reactive protein (CRP); interleukins 6, 7, and 8; and fibrinogen, compared with patients without COPD. In addition, in COPD patients, elevated levels of inflammatory markers, especially CPR, have been associated with the exacerbations of pulmonary disease and worse long-term outcomes.9–12 Thus, more episodes of COPD exacerbation translate into more cardiovascular events, more hospital admissions, and a notable increase in the cost of medical care.33–36
CVD represents the major cause of hospitalization and death among COPD patients and the morbimortality rate is higher among these patients than among the general population. Furthermore, COPD has been determined to be a strong predictor of mortality, recurrent infarction, cardiovascular shock, and bleeding complications in patients suffering from myocardial infarction.30,37–40 Zhang et al6 found that the rate of in-hospital cardiovascular events, including myocardial infarction and heart failure, was increased in COPD patients undergoing PCI. Meanwhile, patients with more frequent or more recent hospitalizations due to COPD exacerbation within one year before PCI were at a higher risk of major adverse cardiovascular and cerebrovascular events (ie, myocardial infarction, repeat revascularization, stroke, and death) during follow-up, especially those with two exacerbations within one year or any exacerbation within one month before PCI.41
Most studies on COPD and CVD to date have focused on advanced or acute stages of one or both diseases, including hospitalization, respiratory infection, acute coronary syndrome, or after coronary revascularization.6,8,13,37–43 Here, we showed that stable patients with subclinical or early-stage of COPD and concurrent CAD were increased risk of long-term cardiovascular events. These results support the relevance of screening for COPD in cardiac patients and could be useful for guiding novel approaches in the patient’s lifestyle and prompting medical treatment to control risk factors, thereby reducing cardiovascular morbimortality.
Cardioprotective medications such as antiplatelets, statins, and cardioselective beta-blockers are rarely used in COPD patients despite the evidence of their safety. Aspirin is mandatory for the treatment of patients with CAD, predominantly after myocardial infarction and cardiac revascularization. Furthermore, the results of observational studies and meta-analyses have suggested that antiplatelet therapy is beneficial for COPD patients, independently of CAD.44 An observational cohort study involving 1343 patients with known thrombocytosis and hospitalized for acute exacerbation of COPD found that antiplatelet therapy was correlated with lower one-year mortality, while the results of another national prospective multicenter study also suggested that antiplatelet medication reduced mortality among COPD patients.45,46
Statins are used primarily in the treatment of hypercholesterolemia and the prevention of cardiovascular events. However, they also have recognized pleiotropic immunomodulatory and anti-inflammatory properties, which may be useful for mitigating the chronic systemic inflammation found in patients with COPD. Data from a large case-control study (Rotterdam Study), which enrolled 7983 participants older than 55 years, showed that long-term statin therapy was associated with a 39% decrease in the risk of all-cause death among COPD patients, independently of age, gender, the use of other drugs, the duration of COPD, pack years, total serum cholesterol, and cardiovascular covariables. This protective effect of statins was even more pronounced in patients with high levels of inflammatory markers (CRP >3 mg/dL), who obtained a 78% reduction in the risk of death.47 Meanwhile, other observational studies reported that only 42% of COPD patients who had any degree of angiographic CAD were receiving statin therapy and 67% among those with angiographically proven severe CAD. The inconsistency of statin prescription may be explained by the more favorable lipid profiles found in COPD patients compared with general population.46,47
Beta-blockers are a standard class of anti-ischemic drugs historically prescribed to patients with CAD and heart failure, for whom they are known to reduce mortality. However, their use among COPD patients remains controversial owing to their potential for inducing acute bronchospasm via the non-selective blockade of β2 subtype receptors, which consequently also inhibits the action of beta-agonist drugs.48,49 Another aspect refers to the heterogeneity of COPD presentation; for instance, studies have reported degrees of pulmonary disease and asthma overlap ranging from 6% to 55%.50
Selective β1 blockers, such as metoprolol and bisoprolol, are significantly less likely to induce bronchoconstriction. They also exert potentially beneficial effects in COPD patients by decreasing heart rate acceleration caused by bronchodilators and may increase the sensitivity of β2 receptors for beta-agonists. Clinical trials and large meta-analyses have shown that cardioselective beta-blockers are safe and are associated with a better prognosis in patients with stable COPD and concurrent CAD, particularly those with milder COPD, even though some results may have been affected by the bias inherent in observational studies.51–58 In contrast, a recent randomized controlled trial (BLOCK-COPD) found no effect of metoprolol in reducing the incidence of exacerbations among patients with moderate to severe COPD who did not have an established indication for the beta-blocker treatment.59
In summary, in the present study, we showed that COPD was undiagnostic in cardiac patients, especially in individuals with stable and mildly symptomatic disease. Additionally, cardiac patients with concurrent COPD were older, had a higher frequency of diabetes, and exhibited more progressive and more severe coronary atherosclerosis than patients without pulmonary disease. COPD was an independent predictor of long-term cardiovascular events requiring coronary angiography, cardiac revascularization, cardiac hospitalization, and myocardial infarction; this adverse cardiovascular prognosis was found even in patients with subclinical and early-stage lung disease. Combined, these results suggest that screening for COPD in cardiac patients may be beneficial to improving their treatment and preventing the occurrence of cardiovascular events.
Study Limitations
This study was a nonrandomized and retrospective cohort and has inherent limitations, including selection bias. Additionally, the diagnosis of COPD was determined by spirometry in patients with stable and mildly symptomatic disease during routine and non-invasive investigation for myocardial ischemia by exercise stress echocardiography; consequently, patients with severe pulmonary disease (GOLD stages III and IV) may have been underrepresented, which may have affected the assessment of the relationship between COPD grades and cardiovascular outcomes. Despite these limitations, we believe that the major strength of this study lies in the quality of the reported event data used to assess the impact of COPD on long-term clinical outcomes. Future prospective and randomized clinical trials will be necessary to confirm these observations.
Conclusions
COPD was associated with an increase in the severity of coronary lesions and adverse cardiovascular events in patients with suspected or confirmed CAD. In addition, COPD was a predictor of long-term cardiovascular events in patients with subclinical or early-stage of lung disease, independently of the established risk factors for CAD. Our findings suggest that screening for COPD in cardiac patients could be useful in risk stratification as well as in determining the appropriate treatment for controlling risk factors and reducing cardiovascular morbimortality.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Vogelmeier C. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2020 report [Internet]. Fontana: Global Initiative for Chronic Obstructive Lung Disease (GOLD); 2020:141. Available from: https://goldcopd.org/wp-content/uploads/2019/12/GOLD-2020-FINAL-ver1.2-03Dec19_WMV.pdf. Accessed August 14, 2023.
2. The top 10 causes of death [Internet]. Newsroom: fact sheets. Geneva: World Health Organization; 2018. Available from: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death. Accessed August 14, 2023.
3. Macedo L, Lacerda EM, Markman-Filho B, et al. Tendências da morbidade e mortalidade da DPOC no Brasil, de 2000 a 2016 [Trends in COPD morbidity and mortality in Brazil, from 2000 to 2016]. J Bras Pneumol. 2019;45(6):e20180402. Portuguese. doi:10.1590/1806-3713/e20180402
4. King P. Inflammation in chronic obstructive pulmonary disease and its role in cardiovascular disease and lung cancer. King Clin Trans Med. 2015;4:26.
5. Enriquez J, Parikh SV, Selzer F, et al. Increased adverse events after percutaneous coronary intervention in patients with COPD. Chest. 2011;140(3):604–610. doi:10.1378/chest.10-2644
6. Zhang M, Cheng Y-J, Zheng W, et al. Impact of chronic obstructive pulmonary disease on long-term outcome in patients with coronary artery disease undergoing percutaneous coronary intervention. Biomed Res Int. 2016;2016:8212459. doi:10.1155/2016/8212459
7. Mannino DM, Higuchi K, T-c Y, et al. Economic burden of chronic obstructive pulmonary disease by presence of comorbidities. Chest. 2014;147:1199–1201. doi:10.1378/chest.15-0380
8. Chen W, Thomas J, Sadatsafavi M, FitzGerald JM. Risk of cardio- vascular comorbidity in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Lancet Respir Med. 2015;3(8):631–639. doi:10.1016/S2213-2600(15)00241-6
9. Daher A, Dreher M. The bidirectional relationship between chronic obstructive pulmonary disease and coronary artery disease. Herz. 2020;45:110–117. doi:10.1007/s00059-020-04893-4
10. Boschetto P, Beghé B, Fabbri LM, Ceconi C. Link between chronic obstructive pulmonary disease and coronary artery disease: implication for clinical practice. Respirology. 2012;17(3):422–431. doi:10.1111/j.1440-1843.2011.02118.x
11. Barnes PJ. Inflammatory mechanisms in patients with chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2016;138(1):16–27. doi:10.1016/j.jaci.2016.05.011
12. Hasan A, Ansari N, Parvez A, Beg M, Bhargava R. Understanding the relation between COPD and coronary artery disease. J Indian Acad Clin Med. 2014;15(2):120–124.
13. Papaioannou AI, Bartziokas K, Loukides S, et al. Cardiovascular comorbidities in hospitalised COPD patients: a determinant of future risk? Eur Respir J. 2015;46(3):846–849. doi:10.1183/09031936.00237014
14. Roversi S, Roversi P, Spadafora G, Rossi R, Fabbri LM. Coronary artery disease concomitant with chronic obstructive pulmonary disease. Eur J Clin Invest. 2014;44(1):93–102. doi:10.1111/eci.12181
15. Kart L, Akkoyunlu ME, Bayram M, et al. COPD: an underdiagnosed disease at hospital environment. Wien Klin Wochenschr. 2014;126(3–4):73–78. doi:10.1007/s00508-013-0458-4
16. Pizarro C, Linnhoff F, van Essen F, et al. Lower extremity and carotid artery disease in COPD. ERJ Open Res. 2016;2(4):00037–02016. doi:10.1183/23120541.00037-2016
17. Williams MC, Murchison JT, Edwards LD, et al. Coronary artery calcification is increased in patients with COPD and associated with increased morbidity and mortality. Thorax. 2014;69(8):718–723. doi:10.1136/thoraxjnl-2012-203151
18. Bestall JC, Paul EA, Garrod R, Garnham R, Jones PW, Wedzicha JA. Usefulness of the Medical Research Council (MRC) dyspnea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54(7):581–586. doi:10.1136/thx.54.7.581
19. Kovelis D, Segretti NO, Probst VS, Lareau SC, Brunetto AF, Pitta F. Validação do Modified Pulmonary Functional Status and dyspnea questionnaire e da escala do Medical Research Council para o uso em pacientes com doença pulmonar obstrutiva crônica no Brasil [Validation of the Modified Pulmonary Functional Status and dyspnea questionnaire and the Medical Research Council scale for use in patients with chronic obstructive pulmonary disease in Brazil]. J Bras Pneumol. 2008;34(12):1008–1018. Portuguese. doi:10.1590/S1806-37132008001200005
20. Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirom- etry. Eur Respir J. 2005;26(2):319–338. doi:10.1183/09031936.05.00034805
21. Pereira CADC. Espirometria. J Bras Pneumol. 2002;28(Suppl 3):S1–S82.
22. Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD executive summary. Am J Respir Crit Care Med. 2017;195(5):557–582. doi:10.1164/rccm.201701-0218PP
23. Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines [published correction appears in Circulation. 2021 Nov 30;144(22):e455]. Circulation. 2021;144(22):e368–e454. doi:10.1161/CIR.0000000000001029
24. Sara L, Szarf G, Tachibana A, et al. II Diretriz de Ressonância Magnética e Tomografia Computadorizada Cardiovascular da Sociedade Brasileira de Cardiologia e do Colégio Brasileiro de Radiologia [II Guidelines for Cardiovascular Magnetic Resonance and Computed Tomography of the Brazilian Society of Cardiology and the Brazilian College of Radiology]. Arq Bras Cardiol. 2014;103(6 Suppl 3):1–86. Portuguese. doi:10.5935/abc.2014S006
25. Scanlon PJ, Faxon DP, Audet A, et al. ACC/AHA practice guidelines ACC/AHA guidelines for coronary angiography. J Am Coll Cardiol. 1999;33(6):1756–1824. doi:10.1016/s0735-1097(99)00126-6
26. Bosco E, Hsueh L, McConeghy KW, et al. Major adverse cardiovascular event definitions used in observational analysis of administrative databases: a systematic review. BMC Med Res Methodol. 2021;21(1):241. doi:10.1186/s12874-021-01440-5
27. Poudel I, Tejpal C, Rashid H, Jahan N. Major adverse cardiovascular events: an inevitable outcome of ST elevation myocardial infarction? A literature review. Cureus. 2019;11(7):e5280. doi:10.7759/cureus.5280
28. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd ed. L. Erlbaum Associates; 1988:147–149. doi:10.4324/9780203771587
29. Mota IL, Sousa ACS, Almeida MLD, et al. Coronary lesions in patients with COPD (Global Initiative for Obstructive Lung Disease Stages I–III) and suspected or confirmed coronary arterial disease. Int J Chron Obstruct Pulmon Dis. 2018;13:1999–2006. doi:10.2147/COPD.S162713
30. Dursunoglu N, Dursunoglu D, Yıldız Aİ, Uludag B, Alaçam ZN, Sarıçopur A. Severity of coronary atherosclerosis in patients with COPD. Clin Respir J. 2017;11(6):751–756. PMID: 266055171. doi:10.1111/crj.12412
31. Schnell K, Weiss CO, Lee T, et al. The prevalence of clinically-relevant comorbid conditions in patients with physician-diagnosed COPD: a cross-sectional study using data from NHANES 1999–2008. BMC Pulm Med. 2012;12(1):26. doi:10.1186/1471-2466-12-26
32. Soriano JB, Rigo F, Guerrero D, et al. High prevalence of undiagnosed airflow limitation in patients with cardiovascular disease. Chest. 2010;137(2):333–340. doi:10.1378/chest.09-1264
33. Mooe T, Stenfors N. The prevalence of COPD in individuals with acute coronary syndrome: a Spirometry-Based Screening Study, COPD. J Chron Obstruct Pulmon Dis. 2015;12(4):453–461. doi:10.3109/15412555.2014.974742
34. Mullerova H, Agusti A, Erqou S, Mapel DW. Cardiovascular comorbidity in chronic obstructive pulmonary disease: systematic literature review. Chest. 2013;144:1163–1178. doi:10.1378/chest.12-2847
35. Eriksson B, Lindberg A, Mullerova H, Ronmark E, Lundback B. Association of heart diseases with COPD and restrictive lung function–results from a population survey. Respir Med. 2013;107:98–106. doi:10.1016/j.rmed.2012.09.011
36. de Lucas-Ramos P, Izquierdo-Alonso JL, Rodriguez-Gonzalez JM, Frances JF, Lozano PV, Bellón-Cano JM; CONSISTE study group. Chronic obstructive pulmonary disease as a cardiovascular risk factor. Results of a case-control study (CONSISTE study). Int J Chron Obstruct Pulmon Dis. 2012;7:679–686. PMID: 23055717; PMCID: PMC3468057. doi:10.2147/COPD.S36222
37. Hadi HA, Zubaid M, Mahmeed WA, et al. Prevalence and prognosis of chronic obstructive pulmonary disease among 8167 Middle Eastern patients with acute coronary syndrome. Clin Cardiol. 2010;33(4):228–235. PMID: 20394044; PMCID: PMC6653010. doi:10.1002/clc.20751
38. Finkelstein J, Cha E, Scharf SM. Chronic obstructive pulmonary disease as an independent risk factor for cardiovascular morbidity. Int J Chron Obstruct Pulmon Dis. 2009;4:337–349. PMID: 19802349; PMCID: PMC2754086. doi:10.2147/copd.s6400
39. Huiart L, Ernst P, Suissa S. Cardiovascular morbidity and mortality in COPD. Chest. 2005;128(4):2640–2646. doi:10.1378/chest.128.4.2640
40. Gupta AS, Rajesh V, James P. Cardiovascular comorbidities associated with patients with chronic obstructive pulmonary disease – a hospital-based study. Egypt J Bronchol. 2019;13(5):591–595. doi:10.4103/ejb.ejb_64_19
41. Lin W-C, Chen C-W, Lu C-L. The association between recent hospitalized COPD exacerbations and adverse outcomes after percutaneous coronary intervention: a nationwide cohort study. Int J Chron Obstruct Pulmon Dis. 2019;14:169–179. doi:10.2147/COPD.S187345
42. Jatene T, Biering-Sørensen T, Nochioka K, et al. on behalf of the BASKET-PROVE investigators, frequency of cardiac death and stent thrombosis in patients with chronic obstructive pulmonary disease undergoing percutaneous coronary intervention (From the BASKET-PROVE I and II Trials). Am J Cardiol. 2016. doi:10.1016/j.amjcard.2016.09.013
43. Campo G, Guastaroba P, Marzocchi A, et al. Impact of COPD on long-term outcome after St-segment elevation myocardial infarction receiving primary percutaneous coronary intervention. Chest. 2013;144(3):750–757. doi:10.1378/chest.12-2313
44. Pavasini R, Biscaglia S, d’Ascenzo F, et al. Antiplatelet treatment reduces all-cause mortality in COPD patients: a systematic review and meta-analysis. COPD. 2016;13(4):509–514. doi:10.3109/15412555.2015.1099620
45. Harrison MT, Short P, Williamson PA, et al. Thrombocytosis is associated with increased short and long term mortality after exacerbation of chronic obstructive pulmonary disease: a role for antiplatelet therapy? Thorax. 2014;69(7):609–615. doi:10.1136/thoraxjnl-2013-203996
46. Ekstrom MP, Hermansson AB, Strom KE. Effects of cardiovascular drugs on mortality in severe chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013;187(7):715–720. doi:10.1164/rccm.201208-1565OC
47. Lahousse L, Loth DW, Joos GF, et al. Statins, systemic inflammation and risk of death in COPD: the Rotterdam study. Pulm Pharmacol Ther. 2013;26(2):212–217. doi:10.1016/j.pupt.2012.10.008
48. Matera MG, Calzetta L, Cazzola M. β-Adrenoceptor modulation in chronic obstructive pulmonary disease: present and future perspectives. Drugs. 2013;73(15):1653–1663. doi:10.1007/s40265-013-0120-5
49. Chang CL, Mills GD, McLachlan JD, et al. Cardio-selective and non-selective beta-blockers in chronic obstructive pulmonary disease: effects on bronchodilator response and exercise. Intern Med J. 2010;40(3):193–200. doi:10.1111/j.1445-5994.2009.01943.x
50. Leung JM, Sin DD. Asthma-COPD overlap syndrome: pathogenesis, clinical features, and therapeutic targets. BMJ. 2017;358:j3772. doi:10.1136/bmj.j3772
51. Salpeter S, Ormiston T, Salpeter E. Cardioselective beta-blockers for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2005;4:CD003566.
52. Albouaini K, Andron M, Alahmar A, et al. Beta-blockers use in patients with chronic obstructive pulmonary disease and concomitant cardiovascular conditions. Int J Chron Obstruct Pulmon Dis. 2007;2(4):535–540.
53. Van Gestel YR, Hoeks SE, Sin DD, et al. Impact of cardioselective beta-blockers on mortality in patients with chronic obstructive pulmonary disease and atherosclerosis. Am J Respir Crit Care Med. 2008;178:695–700. doi:10.1164/rccm.200803-384OC
54. Lalmohamed A, Stojanovic D, Durand M, et al. Benefits of beta blockers in COPD patients and immortal/immeasurable time bias. BMJ. 2011;342:d2549. doi:10.1136/bmj.d2549
55. Rabe KF, Hurst JR, Suissa S. Cardiovascular disease and COPD: dangerous liaisons? Eur Respir Rev. 2018;27(149):180057. doi:10.1183/16000617.0057-2018
56. Li X-F, Mao Y-M. Beta-blockers in COPD: a systematic review based on recent research, Life Sci. 2020;252:117649. doi:10.1016/j.lfs.2020.117649
57. Higuchi S, Kohno T, Kohsaka S, et al. Different impact of beta-blockers on long-term mortality in heart failure patients with and without chronic obstructive pulmonary disease. J Clin Med. 2021;10:4378. doi:10.3390/jcm10194378
58. Etminan M, Jafari S, Carleton B, FitzGerald JM. Beta-blocker use and COPD mortality: a systematic review and meta-analysis. BMC Pulm Med. 2012;12:48. doi:10.1186/1471-2466-12-48
59. Dransfield MT, Voelker H, Bhatt SP, et al. Metoprolol for the prevention of acute exacerbations of COPD. N Engl J Med. 2019;381(24):2304–2314. doi:10.1056/NEJMoa1908142