Cardiovascular
Cardiovascular complications impact COVID-19 community-acquired pneumonia death rates
August 30, 2023
2 min read
Source/Disclosures
Disclosures:
Ali reports no relevant financial disclosures. Please see the study for all other authors’ relevant financial disclosures.
Key takeaways:
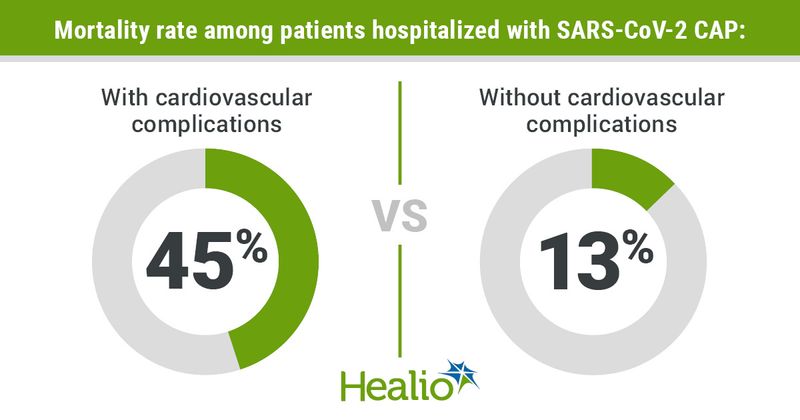
- Almost half of the patients with SARS-CoV-2 community-acquired pneumonia who developed cardiovascular complications died.
- Direct ICU admission was a risk factor for cardiovascular complication development.
Among patients hospitalized with SARS-CoV-2 community-acquired pneumonia, those with vs. without cardiovascular complications had a heightened mortality rate, according to results published in CHEST.
“The primary finding of the current study is that once patients develop a cardiovascular complication, their risk for mortality is substantially increased,” Ahmed Shebl Ali, MD, of the division of infectious diseases at University of Louisville, and colleagues wrote.
In a multicenter retrospective cohort study, Ali and colleagues evaluated 1,645 adults hospitalized with SARS-CoV-2 community-acquired pneumonia (CAP) during wave one (March to July 2020) and wave two (October 2020 to March 2021) of the pandemic to determine how cardiovascular complications change the risk for mortality compared with patients who have no cardiovascular complications.
Researchers defined cardiovascular complications as heart failure, sudden cardiac arrest, cardiogenic shock, acute myocardial infarction, pulmonary edema, new arrythmia, acute worsening of long-term arrhythmia, cerebrovascular accident, myocarditis or deep vein thrombosis.
Researchers also sought to understand which comorbidities and demographics put patients at an increased likelihood for developing cardiovascular complications using Cox proportional hazards regression models.
Of the total cohort, 18% (n = 300) had cardiovascular complications after a median 1.38 days of hospitalization, and a greater proportion of patients with these complications died compared with patients without these complications (45% vs. 13%).
Among the several cardiovascular complications, a new arrhythmia was the most common in this patient population (41%; n = 121), according to researchers.
Several demographics and comorbidities put patients at risk for cardiovascular complications once hospitalized with SARS-CoV-2 CAP, including:
- direct ICU admission (HR = 1.77; 95% CI, 1.36-2.32);
- history of congestive heart failure (HR = 1.59; 95% CI, 1.18-2.15);
- hypoxemia (PaO2/FIO2 less than 200; HR = 1.46; 95% CI, 1.11-1.92);
- history of atrial fibrillation (HR = 1.43; 95% CI, 1.06-1.95);
- age 65 years or older (HR = 1.34; 95% CI, 1.03-1.75);
- history of coronary artery disease (HR = 1.34; 95% CI, 1-1.79); and
- male sex (HR = 1.32; 95% CI, 1.03-1.68).
“Identifying these risk factors may allow clinicians to target high-risk patients for close monitoring and manage any cardiovascular complication in a timely manner,” Ali and colleagues wrote.
Notably, researchers found that once a patient developed a cardiovascular complication, the above factors did not increase risk for mortality. However, they did observe a low likelihood of being alive at discharge among those with hypoxemia (HR = 0.49; 95% CI, 0.3-0.83).
Among those who did not develop a cardiovascular complication, researchers found an elevated risk for mortality with direct ICU admission (HR = 1.8; 95% CI, 1.26-2.55) and a history of cerebrovascular disease (HR = 1.67; 95% CI, 1.12-2.48).
“Future studies should focus on preventing cardiovascular complications and provide a more in-depth analysis on markers of cardiac injury,” Ali and colleagues wrote. “Future studies should also assess long-term sequelae in patients who experienced cardiovascular complications.”