Cardiovascular
Cardiac CT before TAVR detects CAD with high accuracy, suggesting a reduced need for invasive imaging
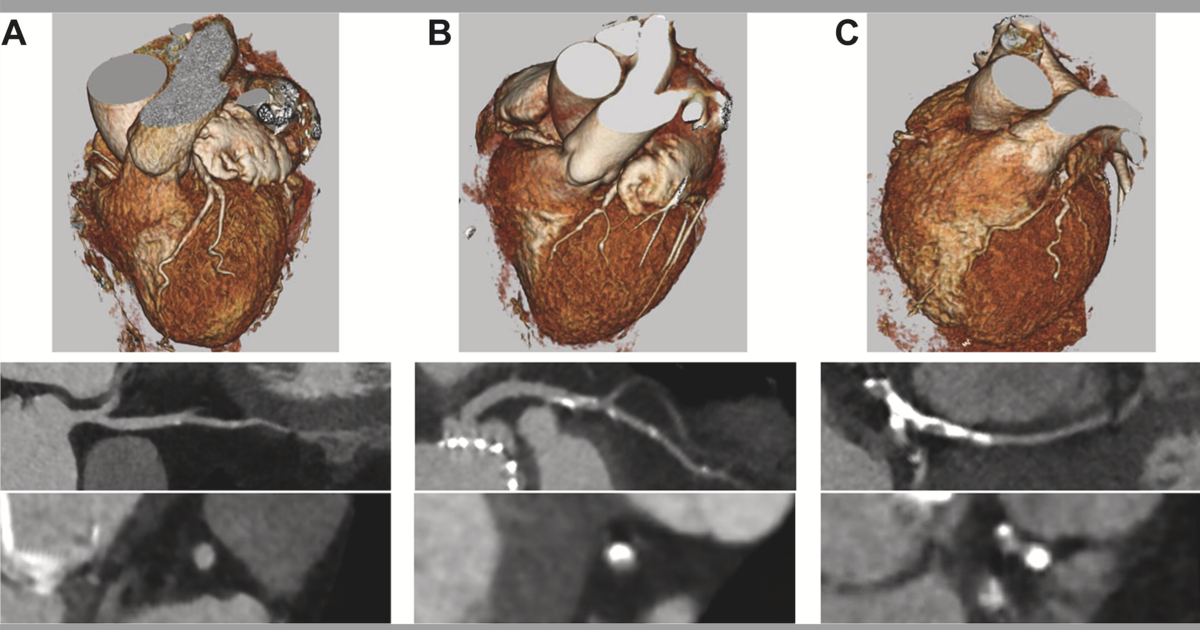
All patients underwent both CTA and ICA before TAVR, but the authors blinded themselves to ICA results to focus on the effectiveness of CTA. CTA coronary reconstruction was used to assess each patient’s left main coronary artery, proximal left anterior descending coronary artery, proximal left circumflex coronary artery, and proximal right coronary artery. At that point, ICA results were reviewed to examine if screening with CTA only provided an accurate snapshot of the patient’s coronary health.
Overall, the authors found that CTA evaluations were associated with a sensitivity of 90%, specificity of 92%, positive predictive value (PPV) of 74% and negative predictive value (NPV) of 97% when detecting stenosis of at least 50%. Those numbers improved to a sensitivity of 91%, specificity of 97%, PPV of 83% and NPV of 99% when detecting stenosis of at least 70%. When identifying graft patency, meanwhile, CTA’s sensitivity was 86%, its specificity was 97%, its PPV was 84% and its NPV was 98%.
In addition, the team performed a Cohen’s kappa analysis that determined the agreement between CTA and ICA was “substantial to near perfect.”
“Although CTA may not be a tool that can guide revascularization, its use has a place in the periprocedural TAVR process in ruling out significant proximal CAD,” the authors wrote. “At our institution, this could have spared 1,148 of 2,217 patients (51.8%) the need for additional invasive testing and the associated risks.”
The group concluded that the consistent use of pre-TAVR screening with CTA “could spare patients the need for additional invasive testing before the procedure.” More research is still needed, however, to further increase the potential impact of noninvasive screening.
Study co-authors from Cleveland Clinic included Samir R. Kapadia, MD; Amar Krishnaswamy, MD; James Yun, MD; Rishi Puri, MD, PhD; and others.
Read the full analysis in JACC: Cardiovascular Interventions here.