Congenital disorders
Fetal Therapy – a hope beyond what you see
Dr. Lucky Gupta
Congenital anomalies are defined as structural or functional disorders that develop prenatally and may be identified before birth, at birth, or later in life. Major congenital anomalies are defined as anomalies with significant effect on life expectancy and they occur in 2-3% of live births and in 20-30% of stillbirths. Not all anomalies require surgical treatment and at present, the best treatment of congenital malformations has been a planned delivery at a tertiary care center.
The rapid advances in imaging techniques and prenatal diagnosis over the last three decades have allowed for the progressive development of prenatal interventions and surgeries and today they become an integral part of the management of high-risk pregnancies. Also, the acceptance of the anomalous fetus as a patient in its own right has propelled the growth of fetal therapy as a viable alternative to the termination of pregnancies or postnatal treatment.
Fetal therapy also known as fetal treatment or prenatal surgery is a procedure on a fetus while it is still developing in the uterus that aims to prevent or correct congenital anomalies in the fetus and prevent their severe consequences on later fetal development. It started with open fetal surgery, and then significantly advanced with innovations, towards minimally invasive fetal procedures. The ethical issues in the field of fetal surgery are complex because the medical intervention is always invasive as it involves at least two patients the mother and fetus. The overall goal of fetal intervention is clear: to improve the health of the fetus while minimizing morbidity and mortality to the mother.
Counseling to the parents about the antenatally detected fetal anomaly and its management presents a medicolegal challenge to the obstetrician and pediatric surgeon and at times help of a perinatologist, a geneticist, and a neonatologist has to be sought. After proper counseling and considering the medical, ethical, and legal aspects of the management of a particular anomaly, further steps will be performed accordingly. Multidisciplinary fetal teams, including a fetal surgeon, obstetrician, ultra sonographer, perinatologist, and anesthesiologist both pediatric and obstetrician, and cardiologist, are critical to the delivery of optimum care to both mother and fetus. Today, fetal therapeutic interventions constitute up to 30% of all fetal interventions performed in a tertiary fetal care clinic.
Fetal therapeutic interventions can be maternal-administered fetal therapy or direct fetal therapy.
Fetal surgery can be classified into three categories
* Open surgery
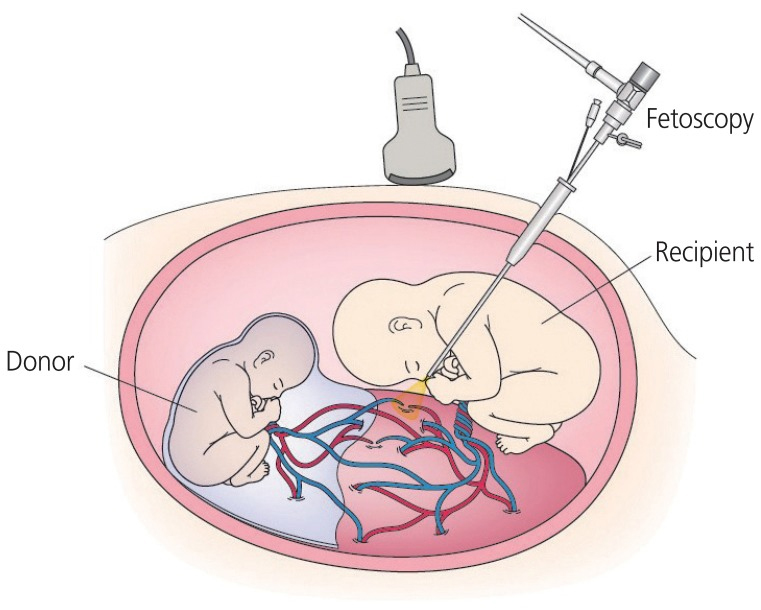
* Fetoscopic surgery i.e. minimally invasive fetal surgery
* EXIT procedures.
The various fetal conditions are intrauterine transfusion for fetal anemia, selective fetal reduction in discordant monochorionic twins, fetal therapy for twin reversed arterial perfusion sequence, and fetoscopic laser coagulation. Other conditions for fetal surgeries are posterior urethral valves, sacrococcygeal teratoma, congenital pulmonary airway malformation, myelomeningocele,congenital diaphragmatic hernia, etc.
EXIT (ex utero intrapartum treatment) is performed at delivery when there is airway obstruction and the baby will not be able to breathe after delivery e.g. tracheal atresia, or large cystic hygroma.
After performing the fetal intervention/surgery, the fetus will remain in the uterus for the remainder of the pregnancy. The mother will be inpatient for approximately 4-5 days, depending upon the procedure. The fetus will be usually delivered by planned Cesarean Section at 36 weeks of gestation. Earlier delivery will be required if pregnancy-associated complications develop.
Repairing the defect before the damage occurs is the principle behind fetal interventions and surgery. However, such interventions are not without fetal or maternal risks. Premature labor, chorioamnionitis, preterm premature rupture of membranes (PPROM), and miscarriage are some of the associated risks of invasive fetal intervention. Additionally, in the case of open fetal surgery, a mandatory cesarean for the current and subsequent deliveries also adds to potential maternal morbidity. The risks to the fetus are prematurity and fetal demise. These risks have to be weighed against the benefits of a planned intervention and every fetus has to be evaluated in detail for suitability. A thorough search for other associated anomalies and if needed, a detailed genetic workup should be undertaken and the results should be discussed with the family before proceeding with the planned intervention.
As always, the goal of fetal therapy is to provide the best possible outcome for the fetus, while minimizing the risk to the mother. The future of fetal therapy is undoubtedly moving toward minimally invasive treatment. To this end, significant efforts are being made toward decreasing the morbidity associated with fetal intervention, particularly Preterm premature rupture of the membranes. Although fetal surgical intervention is limited to the correction of structural anomalies; prenatal stem cell transplantation, and gene therapy are under extensive research to treat a wide range of genetic conditions.
(The author is Assistant Professor Department of Pediatric Surgery, AIIMS, Jammu.)