Blood, Diagnosis, Health Care, Symptoms, Treatment
What Is Iron Deficiency Anemia?
Iron deficiency anemia occurs when there is an inadequate amount of iron in the body to produce sufficient hemoglobin, the protein responsible for carrying oxygen in red blood cells. Insufficient iron levels can result in anemia, leading to symptoms such as headaches, pale skin, fatigue, and others.
The causes of iron deficiency anemia can include insufficient dietary intake of iron, blood loss (such as from menstruation or gastrointestinal bleeding), and certain medical conditions that affect iron absorption or utilization. Treatment approaches vary depending on the underlying cause but often involve dietary modifications to increase iron consumption or the use of iron supplements.
Iron deficiency anemia is a prevalent condition, affecting approximately 30% of the global population. While it can occur in individuals of any age or gender, it is more commonly observed in women and children. Early detection and appropriate management are key to addressing iron deficiency anemia and restoring optimal health.
Iron Deficiency Anemia Symptoms
Iron deficiency anemia is often characterized by a gradual onset of symptoms, which worsen as the condition progresses and the body experiences reduced oxygen supply. While some individuals with mild iron deficiency anemia may not experience noticeable symptoms, common manifestations of the condition can include:
- Fatigue or a persistent lack of energy
- Shortness of breath or chest pain, particularly during physical activity
- Dizziness or lightheadedness
- Headaches
- Pale or yellowish skin
- Cold hands and feet
- Rapid heartbeat or palpitations
- Unexplained weakness
- Pica, which involves cravings for non-food items like clay or ice
- Swollen or sore tongue
- Hair loss
- Brittle nails
What Causes Iron Deficiency Anemia?
Iron deficiency anemia develops when there is an insufficient amount of iron available in the body to produce an adequate amount of hemoglobin. Hemoglobin is the protein in red blood cells that carries oxygen to tissues throughout the body. Low iron levels can occur due to various factors.
Inadequate Iron Intake
Your body relies on dietary sources of iron to maintain healthy iron levels. Consuming iron-rich foods is crucial to prevent iron deficiency and maintain optimal iron status. The recommended dietary allowance (RDA) for iron varies depending on age, sex, and life stage. Here are the RDAs for different population groups:
- Infants 0-6 months: 0.27 mg
- Infants 7-12 months: 11 mg
- Children 1-3 years: 7 mg
- Children 4-8 years: 10 mg
- Children 9-13 years: 8 mg
- Adolescents 14-18 years: 11 mg for males, 15 mg for females
- Adults 19-50 years: 8 mg for males, 18 mg for females
- Adults 51+ years: 8 mg
- Pregnancy: 27 mg
- Breastfeeding: 9-10 mg
Problems Absorbing Iron
Several medical conditions and medications can interfere with iron absorption, leading to iron deficiency anemia. These include:
- Gastrointestinal conditions: Conditions like Crohn’s disease, celiac disease, ulcerative colitis, or an H. pylori infection can affect the absorption of iron in the gastrointestinal tract.
- Digestive system surgery: Certain surgeries, such as bariatric (weight loss) surgery, can alter the normal functioning of the digestive system and impact iron absorption.
- Genetic conditions: Genetic disorders like cystic fibrosis can impair the body’s ability to absorb iron properly.
- Medications: Certain medications used to treat heartburn, ulcers, and other acid-related conditions, such as proton-pump inhibitors (PPIs), calcium carbonate, and histamine-2 receptor antagonists, can interfere with iron absorption when taken long-term.
Blood Loss
Blood loss can lead to iron deficiency anemia as the body loses iron during bleeding. The causes of blood loss associated with iron deficiency anemia include:
- Heavy menstruation: Women with heavy or prolonged menstrual periods may experience significant blood loss, leading to iron deficiency anemia over time.
- Internal bleeding in the gastrointestinal tract: Conditions such as inflammatory bowel disease (e.g., Crohn’s disease, ulcerative colitis), colon cancer, or other gastrointestinal disorders can cause internal bleeding, resulting in iron loss.
- Bleeding during childbirth: Women who experience excessive bleeding during childbirth can develop iron deficiency anemia.
- Regular use of over-the-counter pain relievers: Long-term or excessive use of nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen can lead to gastrointestinal bleeding, contributing to iron deficiency anemia.
- Traumatic injury or surgery: Severe injuries or surgical procedures that involve significant blood loss can deplete iron stores and lead to anemia.
- Urinary tract bleeding: Bleeding in the urinary tract, such as from a urinary tract infection (UTI), can also result in iron loss and contribute to iron deficiency anemia.
Risk Factors
Iron deficiency anemia is indeed common and can affect individuals of all ages. Certain risk factors can increase the likelihood of developing this condition. These include:
- Following a vegetarian or vegan diet: Vegetarian and vegan diets may be lower in iron, especially heme iron found in animal-based sources. This can increase the risk of iron deficiency anemia, but it can be managed by ensuring adequate intake of iron-rich plant-based foods or through iron supplementation.
- Pregnancy, recent childbirth, and breastfeeding: During pregnancy, the demand for iron increases to support the growing fetus and placenta. Blood loss during childbirth can also deplete iron stores. Additionally, breastfeeding can lead to further iron depletion if the mother’s diet does not provide sufficient iron.
- Children who consume excessive cow’s milk: Consuming more than 16-24 ounces of cow’s milk per day in young children can interfere with iron absorption and contribute to iron deficiency anemia. It is important to limit cow’s milk intake and ensure children have a well-balanced diet that includes iron-rich foods.
- Having a chronic inflammatory disease: Chronic inflammatory conditions, such as heart failure or obesity, can disrupt iron metabolism and increase the risk of iron deficiency anemia. Inflammation can affect iron absorption, utilization, and storage in the body.
- Having myelodysplastic syndrome (MDS): Myelodysplastic syndrome is a group of disorders characterized by abnormal production of blood cells in the bone marrow. In MDS, the bone marrow may produce too few healthy red blood cells, leading to anemia, including iron deficiency anemia.
Diagnosis
To diagnose iron deficiency anemia, healthcare providers typically start with a thorough evaluation, including a physical exam and review of symptoms, medical history, and risk factors. They may then order specific blood tests to confirm the diagnosis and assess the severity of anemia.
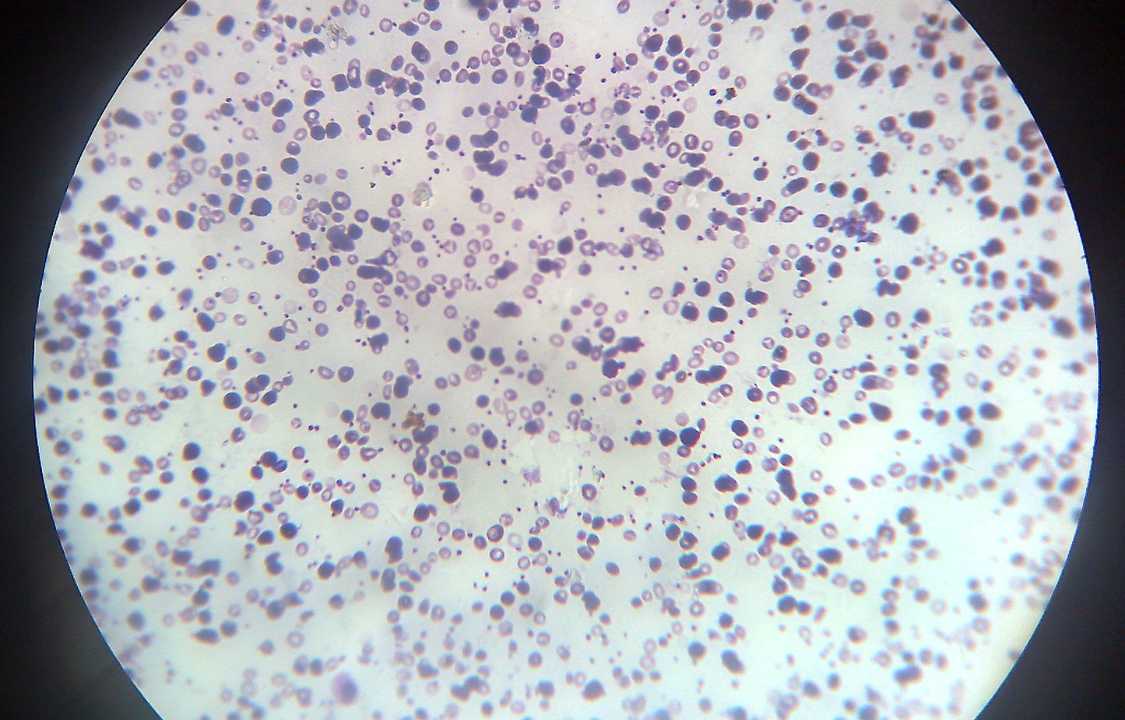
A key blood test used for diagnosis is the complete blood count (CBC), which provides information about red blood cells, hemoglobin levels, and other related parameters. In iron deficiency anemia, the CBC may show a decrease in hemoglobin levels and smaller or paler red blood cells.
In addition to the CBC, healthcare providers may order other blood tests to further evaluate iron status, including:
- Serum iron: This test measures the amount of iron in the blood, helping to assess iron levels in the body.
- Serum ferritin: Ferritin is a protein that stores iron in cells. Measuring serum ferritin levels can provide information about iron stores in the body. Low ferritin levels are indicative of iron deficiency.
- Serum transferrin: Transferrin is a protein that transports iron throughout the body. High levels of serum transferrin can suggest iron deficiency.
- Peripheral blood smear: This test involves examining a blood sample under a microscope to assess the size, shape, and color of red blood cells. Iron deficiency anemia may show small or pale red blood cells.
If bleeding is suspected as a cause of anemia, additional tests may be ordered, such as:
- Fecal occult blood test: This test detects the presence of blood in the stool, indicating gastrointestinal bleeding.
- Endoscopy: Using a camera-equipped tube inserted through the mouth, the esophagus and stomach are examined to identify potential sources of bleeding in the upper gastrointestinal tract.
- Colonoscopy: A similar procedure to endoscopy, but focuses on visualizing the colon to check for abnormalities or sources of bleeding.
- Pelvic examination and ultrasound: For individuals who menstruate, a pelvic examination can help identify sources of bleeding, and an ultrasound may be used to evaluate the uterus and bladder for abnormalities causing heavy or abnormal menstrual bleeding.
- Urine testing: This helps detect the presence of blood or hemoglobin in the urine, which may indicate bleeding in the urinary tract.
Treatments for Iron Deficiency Anemia
Treatment for iron deficiency anemia aims to replenish iron levels and address any underlying causes. The specific treatment approach depends on the severity of the anemia and individual factors. Here are some common treatment options:
- Dietary Changes: Consuming iron-rich foods can help restore iron levels. This includes incorporating sources of heme iron from animal products like red meat, poultry, and seafood, as well as non-heme iron from plant-based sources like beans, leafy green vegetables, fortified grains, and pasta. Including vitamin C-rich foods with iron-rich meals can enhance iron absorption.
- Iron Supplements: Iron supplementation is often recommended to boost iron levels. Over-the-counter iron supplements or prescription iron supplements in liquid, tablet, or capsule form may be prescribed. Taking vitamin C supplements alongside iron supplements can enhance iron absorption.
- Intravenous (IV) Iron: In cases of severe iron deficiency anemia, poor iron absorption, or intolerance to oral supplements, intravenous iron may be administered. This involves receiving iron directly into the bloodstream through an IV in a healthcare setting. It can be given in a single large dose or multiple smaller doses over several weeks.
- Blood Transfusion: Severe cases of iron deficiency anemia, particularly those associated with acute blood loss or significant symptoms, may require blood transfusions. Blood transfusions involve receiving donated blood to quickly replenish red blood cells. While blood transfusions provide temporary relief, they do not address the underlying iron deficiency, so additional treatments are necessary to restore iron levels.
Prevention
To maintain healthy iron levels and prevent iron deficiency anemia, it is important to make certain lifestyle choices. Here are some recommendations:
- Iron supplementation: If you possess risk factors for iron deficiency anemia, consult your healthcare provider who may recommend iron supplements. In some cases, a multivitamin containing iron may suffice.
- Address underlying causes: If you have an underlying condition that increases the risk of iron deficiency or experience heavy bleeding, collaborate with your healthcare provider to manage the condition effectively and prevent excessive bleeding.
- Moderate caffeine intake: It is advisable to limit the consumption of caffeinated beverages such as coffee, tea, and other similar drinks. Caffeine can hinder the absorption of iron in the body.
Complications
Untreated iron deficiency anemia can result in various health complications, including the following:
- Cardiovascular problems: Anemic individuals may experience a rapid or irregular heartbeat as their heart works harder than usual. If left untreated, this can eventually lead to heart failure.
- Increased susceptibility to infections: Iron deficiency anemia weakens the immune system, making individuals more prone to infections.
- Complications during pregnancy: Pregnant individuals with iron deficiency anemia face a higher risk of preterm delivery, low birth weight, and postpartum depression.
- Impaired growth and development: Children with severe or long-term iron deficiency anemia may encounter growth and developmental delays, along with shorter attention spans.
- Cognitive impairment: Severe iron deficiency anemia can lead to cognitive problems, including memory difficulties, lack of focus, and poor concentration.
- Restless legs syndrome: This condition is characterized by an irresistible urge to move the legs due to uncomfortable sensations experienced.
Living With Iron Deficiency Anemia
If you are suffering from iron deficiency anemia, it is common to experience weakness and a lack of energy, making it challenging to perform daily tasks. Managing the condition and its symptoms can be frustrating, but it is crucial to take care of yourself both physically and emotionally.
Treatment for iron deficiency anemia aims to restore your iron stores, and you should start feeling better within a few weeks. It may take a few months for your iron stores to be fully replenished. In the meantime, it is important to focus on following a healthy and balanced diet, taking your prescribed iron supplements as directed, and giving yourself enough rest whenever possible.
Seeking support from your loved ones can also be beneficial during this time. Reach out to family and friends for assistance and understanding. If you find that your symptoms are not improving with treatment, it is important to contact your healthcare provider for further guidance and evaluation.
Remember to prioritize self-care and stay consistent with your treatment plan to effectively manage iron deficiency anemia and regain your energy levels.