Cardiovascular
Maintaining residual kidney function linked to reduced risk of cardiovascular death
September 06, 2023
2 min read
Source/Disclosures
Published by:
Disclosures:
Okazaki and Daugirdas report no relevant financial disclosures. Please see the study for all other authors’ relevant financial disclosures.
Key takeaways:
- Patients on hemodialysis had a lower risk of cardiovascular death if they maintained some residual kidney function (RKF).
- Research is needed to determine whether uremic toxins play a role in mortality risk.
Results from a national cohort study of 39,623 patients starting thrice-weekly in-center hemodialysis showed that a lower baseline of urea was consistently associated with greater risk of cardiovascular death.
“[Residual kidney function] RKF is associated with improved survival among patients
on hemodialysis,” Masaki Okazaki, MD, of the Harold Simmons Center for Kidney Disease Research and Epidemiology, division of nephrology, hypertension and kidney transplantation, University of California Irvine School of Medicine, and colleagues wrote. “RKF substantially contributes to the maintenance of fluid and electrolyte balance and
enhanced clearance of both middle molecules and protein-bound solutes.
“Therefore, it is postulated that RKF could lead to better cardiovascular outcomes.”
Urea clearance, volume
The researchers looked at renal urea clearance and urine volume in the study group from Jan 1, 2007 to Dec. 31, 2011, using a multivariable cause-specific proportional hazards model to examine the associations between baseline RKF and cause specific mortality, including sudden cardiac death (SCD), non-SCD cardiovascular death (CVD), and non-CVD. SCD was defined as death due to cardiac arrest and cardiac arrhythmia; non-SCD CVD was defined as death in the patient study group attributable to acute myocardial infarction, atherosclerotic heart disease, congestive heart failure, cerebrovascular accident and other cardiovascular causes excluding SCD, the researchers wrote, and non-CVD “was death from infectious diseases, malignancy, withdrawal from dialysis or uremia and all other known causes.”
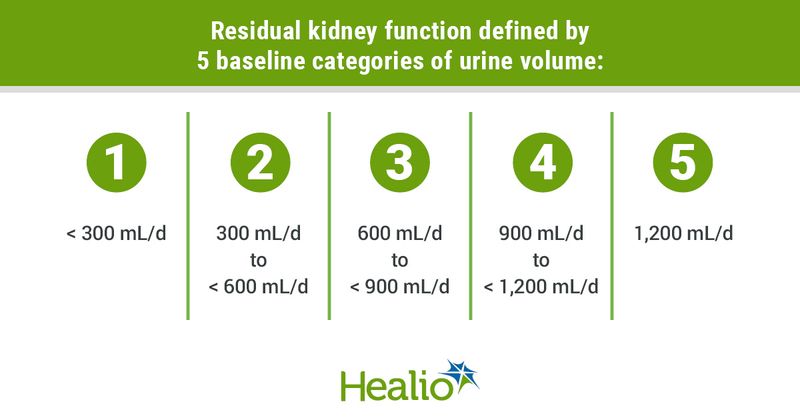
RKF was defined by 5 categories of baseline urine volume, including less than 300 ml/d; 300 ml/d to less than 600 ml/d; 600 ml/d to less than 900 ml/d; 900 ml/d to less than 1,200 ml/d and 1,200 ml/d.
Higher mortality
The study results showed a “significant trend toward a higher mortality risk across lower RKF levels, irrespective of cause of death in a case-mix adjustment model … Adjustment for ultrafiltration rate (UFR) slightly attenuated the association between low renal [urea clearance] and high cause-specific mortality, whereas adjustment for highest potassium did not have substantial effect,” the authors wrote.
Among the 12,169 patients where RKF changed over the length of the study, “a 6-month decline in renal [urea clearance] showed graded associations with SCD, non-SCD CVD, and non-CVD risk, whereas the graded associations between faster 6-month decline in urine output and higher death risk were clear only for SCD and non-CVD,” the authors wrote.
The association with SCD and non-CVD “were consistent across strata of demographics and relevant clinical factors,” the authors wrote. “In addition, a decline in renal [urea clearance] during the first 6 months of hemodialysis also showed a graded association with increased mortality in SCD, non-SCD CVD, and non-CVD.”
In a separate editorial, John T. Daugirdas, MD, from the department of medicine, division of nephrology at the University of Illinois College of Medicine, said the study results “suggest a broad-based benefit of increased residual kidney function on survival. The association was not limited to a reduced rate of sudden cardiac deaths or of non-SCD cardiovascular deaths but was as or more prominent with non-cardiovascular mortality,” Daugirdas wrote. “The exact mechanism whereby residual kidney function reduces death risk remains incompletely defined, but most likely is related to reduced serum levels of potential uremic toxins as opposed to reduced need for ultrafiltration or reductions in incidence of hyperkalemia.
“ … Future exploration of the role of RKF and urine volume on hard outcomes should ideally include measurement of serum levels such uremic toxins,” Daugirdas wrote.