Infection
8 long-term effects of infectious arthritis, prevention and management tips
Health expert reveals the long-term effects of infectious or septic arthritis along with some prevention and management tips
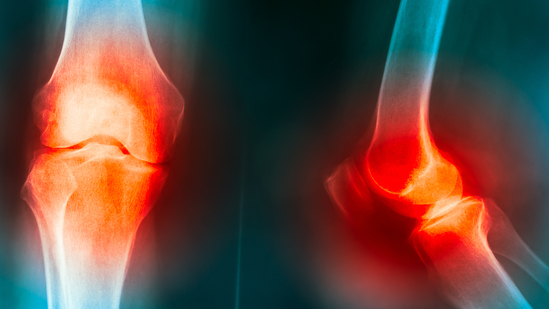
Infectious arthritis, also known as septic arthritis, is a health condition that arises when a joint becomes infected by microorganisms such as bacteria, viruses or fungi. While the acute phase of infectious arthritis can be painful and debilitating, the long-term effects of this condition can also have a lasting impact on joint health, mobility and overall quality of life.
In an interview with HT Lifestyle, Dr Prithaviraj Deshmukh, Orthopedic Surgeon and Pain Management Specialist at Nexus Day Surgery Center in Mumbai, revealed the 8 long-term effects of infectious arthritis –
- Joint Damage and Deformities: One of the most significant long-term effects of infectious arthritis is joint damage. The infection causes inflammation within the joint, leading to the destruction of cartilage and bone. This damage can result in joint deformities, which can affect both the function and appearance of the joint. Over time, the joint’s ability to move smoothly and bear weight can be compromised, leading to decreased mobility and potentially altering the individual’s gait.
- Chronic Pain and Discomfort: Long-term pain and discomfort are common consequences of infectious arthritis. The persistent inflammation caused by the infection can result in chronic pain that affects daily activities and reduces overall quality of life. The pain can be worsened by joint damage, nerve irritation, and ongoing inflammation, leading to limitations in movement and difficulty performing simple tasks.
- Limited Range of Motion: Infectious arthritis can lead to stiffness and limited range of motion in the affected joint. The ongoing inflammation and joint damage can cause scar tissue to form, restricting the joint’s ability to move freely. This limitation can impact daily activities such as walking, reaching and bending, making it challenging to maintain an active lifestyle.
- Secondary Osteoarthritis: In some cases, infectious arthritis can lead to the development of secondary osteoarthritis. The initial infection can accelerate the breakdown of joint tissues, including cartilage. Over time, this can contribute to the development of osteoarthritis, a chronic degenerative joint condition. Osteoarthritis can worsen joint pain, reduce joint function and further complicate the management of the affected joint.
- Functional Impairment: The combined effects of joint damage, pain, limited range of motion and potential deformities can lead to functional impairment. Individuals with infectious arthritis may find it challenging to perform basic activities of daily living such as dressing, bathing, and cooking. Functional impairment can significantly impact independence and overall well-being.
- Psychosocial Impact: The long-term effects of infectious arthritis can extend beyond physical symptoms to affect a person’s emotional and psychological well-being. Coping with chronic pain, functional limitations and potential disability can lead to feelings of frustration, anxiety and depression. Individuals may also experience a loss of identity, especially if their ability to engage in activities they once enjoyed is compromised.
- Recurrence and Reinfection: While successful treatment can resolve the acute infection, there is a risk of recurrence or reinfection in some cases. Factors such as immune system function, underlying health conditions, and the presence of prosthetic joints can contribute to the risk of recurrent infections. Repeat infections can exacerbate the long-term effects of infectious arthritis and further damage the joint.
Prevention and Management
Dr Prithaviraj Deshmukh suggested, “Preventing and managing the long-term effects of infectious arthritis requires a comprehensive approach. Timely and appropriate treatment of the initial infection is crucial to minimize joint damage. Antibiotics, antiviral medications, or antifungal treatments may be prescribed based on the causative agent. Post-infection, ongoing medical monitoring is necessary to detect any signs of recurrence or complications. Physical therapy plays a vital role in maintaining joint function, reducing stiffness, and improving muscle strength. Assistive devices such as canes or braces may be recommended to support joint stability and mobility.”
He recommended, “Lifestyle modifications, such as maintaining a healthy weight and engaging in joint-friendly exercises, can help alleviate strain on affected joints. Psychological support, counselling, and pain management strategies can address the emotional toll of living with infectious arthritis. In conclusion, the long-term effects of infectious arthritis can be complex and far-reaching. Joint damage, chronic pain, limited mobility and potential psychosocial impact are some of the challenges individuals may face. ”
Early and comprehensive treatment, along with ongoing management and support, is essential to mitigate the impact of infectious arthritis on joint health and overall quality of life. By addressing the physical, emotional and functional aspects of the condition, individuals can work towards achieving a better quality of life despite the challenges posed by infectious arthritis.