Cancer and neoplasms
Knowledge and Attitude of Adolescents Regarding HPV Vaccine
Introduction
In the context of an alarming decline in HPV vaccination coverage globally, from 25% to 15% between 2019 and 2021, the WHO recommends that countries reinforce their HPV vaccination programs.1
Also, according to The European Cancer Organization report, it is estimated that about 29% of girls and 5% of boys were completely vaccinated with the HPV vaccine in 2020; there are still disparities between different regions and countries, with the lowest coverage in Eastern Europe (3% of girls and 0% of boys completely vaccinated) and the highest in Northern Europe (68% of girls and 11% of boys completely vaccinated).2
HPV vaccination in Romania is included in the National Vaccination Program, in the category of immunization of population groups at risk; it is an optional vaccination, which is carried out at the request of parents or legal representatives, request expressed through a solicitation made at the family doctor’s office. Initially, eligibility for free vaccination was regulated for girls in the age group of 11–14 years, but in September 2021, through a change in the legislation, the age group was extended to 18 years. Thus, at this moment, the vaccine is offered free of charge to girls who, at the time of request, are in the age group of 11–18 years.3–5 After two HPV vaccination campaigns that unfortunately did not work – The first, launched in 2008, lacking from the start in terms of information, addressed to 10–11-year-old girls and carried out in school offices, based on written consent of the parents, resulting in the vaccination of a proportion of 2.57% of the eligible girls (2.615 out of the 110.000 targeted), then the second, which was actually a relaunch of the first one, in June 2009, but targeting sixth- and seventh-grade girls, with an official information campaign under the slogan “You decide for your daughter’s health. Get informed!”, with a strategy that involved, first of all, informing and educating doctors and teachers, followed by meetings with parents and an opinion survey among them, with a dedicated website and a free phone line, but with still very low vaccination rates,6 the campaign was resumed in 2017, when the quarterly transmission to the National Institute of Public Health of the required doses for eligible girls was requested, girls for which parents submitted an application to the family doctor; the family doctors were informed and they started the catography.
At the end of 2019, more precisely in December, the vaccine was delivered to all Public Health Directorates and distributed according to requests; along with the vaccine, information leaflets about HPV infection and its associated risks were sent. Effective vaccination started in January 2020 and is ongoing depending on the availability of the vaccine and the number of requests.7 Thus, at this moment, the target group for HPV vaccination is represented by adolescents; at this stage of development, a series of major changes take place both physically, emotionally and behaviorally, aiming at independence in decision-making,8 including those related to vaccination. At this age, adolescents want to make their own choices about their own health and develop attitudes and behaviors that persist into adulthood. Vaccination behavior is influenced by their own views and opinions, but also by interaction with parents, friends, medical staff, as well as information they can access through the Internet, social networks or mass media.8,9
A series of studies that address the topic of HPV vaccination, namely attitudes, perceptions related to vaccination, but also strategies to combat hesitant behavior and increase vaccination rates, evaluate these issues from the parent’s point of view; very few studies approach these topics from the perspective of the adolescent.10–12 A hesitant behavior of parents related to HPV vaccination is decisively associated with low rates of HPV vaccination among adolescents.10,11 This is also the reason why the specialized literature addresses the issue of pro-vaccination education, in an attempt to identify interventions that can change the attitude of parents and implicitly of adolescents.13 Some studies suggest focusing on the generation directly targeted by vaccination: children, adolescents, young people.9–11,13
Public health programs aimed at educating adolescents about HPV vaccination have been shown to have a positive effect on their attitude, but they must be correlated with correct information for both adolescents and parents, and this is where the medical staff decisively intervenes, who, in turn, must be trained to provide accurate information.11–13 Cervical cancer ranks 4th globally in the grim ranking of the most common forms of cancer in women, with 604.000 new cases diagnosed in 2020 and 342.000 deaths recorded in the same year.14–16
In Romania, it ranks 3rd among all forms of cancer in women and 2nd if we talk about cancer in women aged 15–44. The latest statistics, from 2020, indicate 3380 new cases and over 1800 deaths.17 Almost all cases of cervical cancer can be attributed to HPV infection.14 It is the most common sexually transmitted infection, but most infections are asymptomatic; however, a small proportion of these may persist and progress not only to cervical cancer, but also to neoplasms of other locations. More than 200 HPV types have been identified, types 16 and 18 being the ones characterized by the highest carcinogenic capacity, causing 70% of cervical cancers worldwide.14,18 Prof. Harald zur Hausen was awarded the Nobel Prize in 2008 for demonstrating the involvement of HPV in cervical cancer, by isolating the genomes of virus types 16 and 18 from tumor cells.19 On the other hand, cervical cancer is the most preventable form of cancer, through vaccination and screening.14 The first HPV vaccine was licensed in 2006; currently, 6 types of vaccine are licensed, being indicated for administration to girls starting at the age of 9, up to 26 or 45 years; some vaccines can also be administered to males.20 By December 2022, 125 countries (64%) had introduced HPV vaccination in their national immunization programs for girls, while 47 countries had also introduced immunization in boys.20 The HPV vaccination in Romania is included in the national program as an optional vaccination (immunization of population groups at risk) and it is not part of the biannually evaluation of the vaccination coverage, which takes place in February and August; at this moment, we do not have official information regarding HPV vaccination coverage in Romania. In this study, we focused on the assessment of attitudes, perceptions and knowledge about HPV infection, HPV vaccination and cervical cancer, to highlight the importance of adolescent education as an important strategy for improving vaccination rates. The main aim of the study was to evaluate both knowledge and attitudes, as well as intentions, reservations, reasons that could influence the decision related to vaccination. The secondary aim was to identify the main behavioral patterns regarding HPV vaccination corresponding to the two GNV and GPV samples, in order to understand the mentalities that determine the attitudinal differences. The study was conducted in the context of an increasingly evident hesitant behavior related to vaccines and vaccination and in the absence of educational strategies/interventions addressed to the target group. The study can be the starting point for the development and implementation of strategies to combat hesitant behavior and increase vaccine acceptability for HPV vaccination.
Materials and Methods
Study Design
The study was carried out in 15 high schools from Bihor County, between April and June 2022 and involved the application of a questionnaire to teenage girls in the age group of 18–19 years, teenage girls that are in a position to make their own, assumed, informed decisions regarding their health status in general and vaccination in particular.
At first, we obtained the permission from the principals of all schools in order to apply the questionnaire, then all the eligible teenagers were informed that participation was voluntary, that only the investigators would have access to the personal data and that all results would be presented for the group, not individually.
Most of the questionnaires in print format were distributed and collected by the principal investigator or, in certain situations, by a designated person within the educational unit, trained in this regard.
The study was structured in six stages: identification of the female subjects in the 18–19-year-old group (stage I), distribution and collection of the questionnaires (stage II), establishing the belonging to one of the groups – GNP or GNV (stage III), the centralization, processing and interpretation of the results of the questionnaire for GPV and GNV (stage IV), identification of the main behavioral patterns of the two groups, in order to determine the main items that determine them and implicitly to highlight the level of knowledge and attitudes regarding HPV infection, vaccination and cervical cancer (stage V) and presenting previous studies that address the same topic and determine how or if the main results of this study are aligned with these or which are the differences found (stage VI).
The study was approved by the Ethics Committee of Oradea County Emergency Clinical Hospital – approval no. 1534 of 17.01.2019.
Participants
The studied group included 690 teenage girls aged 18–19, who agreed to complete the questionnaire; no parental consent was required. The total population of Bihor County, which was taken into account for this study, was of 6314 girls aged 18–19 years old. The required sample size calculated for this total population is represented by 363 subjects for a confidence level of 95%; the real value was within ±5% of the surveyed value. Inclusion criteria: at least 18 years of age, but within the WHO definition of adolescence as a stage of development (10–19 years), female gender, voluntary agreement to participate in the study, full completion of the questionnaire.
Instrument of Evaluation
The basis of the study was a survey based on an anonymized questionnaire, structured in two parts – one general and one specific. The general part was divided into three categories: personal information (age, background), data regarding the source of information about HPV vaccination and data on the motivations for non-vaccination against HPV. The second, specific part consisted of a survey based on a questionnaire called the Attitudinal Identification Questionnaire Regarding HPV vaccination, with 3 subscales: subscale 1 – general attitudes about vaccines and vaccination (3 items), subscale 2 – knowledge about HPV infection, HPV vaccination and cervical cancer (8 items), subscale 3 – attitudes and perceptions related to HPV vaccination (4 items).
The Attitudinal Identification Questionnaire Regarding HPV vaccination was designed by the authors after consulting and reviewing the specialized literature on HPV vaccination from the perspective of adolescents and was approved by clinical psychologists from UMF “Iuliu Hațieganu” Cluj Napoca. The questionnaire was evaluated on a scale from 1 to 3 as follows: 1 – no, 2 – I do not know, 3 – yes.
Statistical Analysis
The results of the present study were processed using IBM-SPSS 22. The statistical indicators of the study were: mean (X), standard deviation (SD), arithmetic mean difference (MD), Student’s T-Test (t), level of probability (p), Confidence Interval with two levels: upper and lower (95%). For statistical significance of the study, we selected p ≤ 0.05. The method of measuring the reliability of the subkeys of the questionnaire and of the entire questionnaire was achieved by calculating Cronbach’s Alpha, which reflects the internal consistency, ie, the level of connection of a set of items as group elements. We used the Rotation Method: Varimax with Kaiser-Meyer-Olkin (KMO) to check the adequacy of sampling for the analysis and Bartlett’s test of sphericity; all the 15 items of the questionnaire were analyzed. For the present study, we considered it was relevant to take into account positive values greater than 0.700 for the factor analysis. The factor analysis (PCA) consists of the technique by which a large number of variables is reduced into a smaller number of factors by extracting the maximum common variation from all the analyzed variables and summing them into a distinct score usable in the analysis of behavioral patterns regarding the attitude towards HPV vaccination. In the case of factorial analysis, the Eigenvalues are also called characteristic roots that highlight the initial variance explained by that particular factor from the total variance; it is expressed as a percentage. A high factor score revealed a pattern of high educational relevance for HPV vaccination.
Results
Based on the answers to the question corresponding to item 14 of subscale 3 “if at this moment you were offered vaccination against HPV infection, what would be your attitude?”, we identified, at the time of applying the questionnaire, two groups: the group of teenage girls with a hesitant behavior – those who answered “do not know what decision I would take” or “I refuse” (n = 382) and the group of teenage girls without a hesitant behavior – those who answered “I would accept” or “I am already vaccinated” (n = 308). 5.51% from the girls included in the study were already vaccinated. The first group, which showed a hesitant attitude for HPV vaccination was called – The non-vaccine group (GNV), and the group that showed a positive attitude toward HPV vaccination was called – The pro-vaccine group (GPV).
Personal Data
The majority of the participating teenage girls (78.26%) were 18 years old at the time of application of the questionnaire, while 21.74% were 19 years old. 57.83% of the participants came from urban areas, while 42.17% live in rural areas. Also, when reported to the entire sample, participants from rural areas predominate in GNV (185–63.57% versus 106–36.43%). The characteristics of the participants are presented in Table 1.
 |
Table 1 Personal Data of the Study Samples |
The results of the Attitudinal Identification Questionnaire Regarding HPV Vaccination
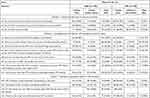
The results in Table 2 highlight the fact that a higher proportion of subjects from GPV show knowledge about HPV infection, HPV vaccination and cervical cancer and more positive attitude regarding HPV vaccination. For all three subscales, the answers of three points – yes – were higher for respondents from GPV compared to those from GNV.
|
Table 2 Comparative Analysis of the Distribution of Subjects According to the Weight of the Answers to the Subscales of the Attitudinal Identification Questionnaire Regarding HPV Vaccination, for the Two Groups (GNV versus GPV) |
In Subscale 1 – General attitudes related to vaccines and vaccination, the biggest difference between the groups regarding the affirmative answers (3 points – yes) was recorded in Q3. Do you think vaccines are safe? In favor of GPV (68.50% versus 29.06%), and the lowest in Q1. Do you think vaccines are necessary to prevent certain diseases? Also for GPV (97.40% versus 79.84%).
In Subscale 2 – Knowledge about HPV infection, HPV vaccination and cervical cancer, positive results for GPV were higher than for GNV. The biggest differences between groups for affirmative answers (3 points – yes) were recorded for item: Q11. Have you ever heard that HPV vaccination protects against genital HPV infection? Where 162 subjects (42.41%) answered affirmatively for GNV, and 225 subjects (73.05%) for GPV. The smallest difference between groups for affirmative answers was recorded for item Q5. Have you ever been told by a doctor that you have a sexually transmitted infection? (2.60% versus 2.36%).
The analysis of the results for the responses of the subjects from the two groups for Subscale 3 – Attitudes and perceptions related to HPV vaccination highlights a higher share of affirmative responses of GPV compared to GNV for all items (Table 2).
The statistical parameter Cronbach’s Alpha calculated for the entire questionnaire recorded values higher than 0.800 for both groups (0.872 for GNV and 0.858 for GPV), which reflects a very good high reliability and the results of the questionnaire are statistically validated for this study (Table 3). Also, the analysis of Cronbach’s Alpha values for each subscale, for both GNV and GPV groups, reflected a good and very good reliability, with the values falling between 0.714 and 0.896.
 |
Table 3 Cronbach’s Alpha Values of the Attitudinal Identification Questionnaire Regarding HPV Vaccination and Subscales |
The results of the Attitudinal Identification Questionnaire Regarding HPV vaccination for both GPV and GNV groups were statistically significant for all items, the significance threshold values being lower than the selected reference value of p < 0.05 (Table 4). Analyzing the arithmetic averages of the two groups included in the study, we can observe that the results of GPV are higher than those recorded by GNV for all items of the three subscales of the questionnaire. The differences of arithmetic mean between GPV and GNV, for all items, fell between the lower and upper limits of the 95% Confidence Interval. The statistically significant differences between the two groups reflect a higher level of knowledge and a more positive attitude in GPV compared to GNV, a fact that must be optimized by developing and implementing a health education strategy at the level of the young generation and by expanding the methods of information in high schools.
|
Table 4 Descriptive Statistics of the Attitudinal Identification Questionnaire Regarding HPV Vaccination |
In the study, separately for GNV and GPV, we performed a principal components analysis (PCA) on the 15 items of the Attitudinal Identification Questionnaire regarding HPV vaccination with orthogonal rotation (Varimax). The Kaiser-Meyer-Olkin measure verified the sampling adequacy for the analysis, KMO = 0.779 for GNP and KMO = 0.765 for GPV, values that are above Kaiser’s criteria (>0.5). Bartlett’s test of sphericity for GPV was χ2 (105)= 1657.476, p < 0.001, and for GNP χ2 (105)= 1587.589, p < 0.001 which indicated a sufficiently high correlation between items for PCA (Table 5).
|
Table 5 Items Relevance for the Patterns – Rotated Component Matrix for GNV and GPV |
Following the data analysis, we identified that for GNV five components had eigenvalues above Kaiser’s criterion of 1 and in combination explained 63.56% of the variance. Following the processing of the GNV results, five behavioral patterns were obtained (Table 5) which were renamed according to the most relevant value obtained vertically as follows: C1-Q6. Have you ever heard that the HPV virus is transmitted through unprotected sex? With 0.862; C2 – Q12. HPV vaccination would be beneficial in protecting me in the future with 0.780; C3 – Q1. Do you think vaccines are necessary to prevent certain diseases? With 0.805; C4 – Q10. Have you ever heard that there is currently a vaccine that can prevent HPV infection and by implication cervical, vulvar, vaginal cancer? With 0.708; C5 – Q5. Have you ever been told by a doctor that you have a sexually transmitted infection? With 0.974. In order to highlight the most significant items that define the five behavioral patterns, we have bolded the numbers in Table 5 for GNV. For GNV, Eigenvalues showed the variance for each identified component, the highest percentage value being 24.54% for the first component, and the lowest for the fifth component of 6.74% (Table 5).
According to Table 5, the analysis of GPV results highlights 4 behavioral patterns whose eigenvalues were above Kaiser’s criterion of 1 and in combination explained 60.68% of the variance. The four behavioral patterns of GPV (Table 5) were renamed according to the most relevant value obtained vertically as follows: C1 – Q4. Have you ever heard of HPV (human papilloma virus) infection? With 0.817; C2 – Q14. If at this moment you were offered vaccination against HPV infection, what would be your attitude? With 0.849; C3 – Q2. Do you think it is important for you and your loved ones to be vaccinated? With 0.871; C4 – Q5. Have you ever been told by a doctor that you have a sexually transmitted infection? With 0.726. We have bolded the items that are significant for each of the 4 patterns for GPV in Table 5. For GPV, Eigenvalues showed the variance for each identified component, the highest percentage value being 23.65% for the first component, and the lowest for the fifth component of 7.30% (Table 5).
Analysis of the Results Regarding the Information Environment Regarding HPV Vaccination and Information About the Motivations for Not Vaccinating
Most of the participants (70.58%) specified that they had heard about HPV infection. When asked where some adolescent girls indicated a single source, while others indicated different environments in which this topic was discussed; thus, 27.82% said they heard about HPV infection from medical personnel, 22.17% at school, 19.56% from a family member or friend, 9.71% from TV/radio, while 32.03% said they read on the internet. A small part (1.16%) indicated that they documented themselves, reading certain magazines or books in the medical field. In the studied group, the main reason that would lead participants to refuse vaccination, would be the fear of possible side effects (46.52%), followed by the concern that the vaccine is not safe (35.36%), the concern that the vaccine will not be effective (12.75%), fear of injection (8.55%), vaccine cost (7.54%). Other reasons cited were: insufficient knowledge about the vaccine or the fact that they have not started their sexual activity and do not see the point of vaccination; in contrast, some teenage girls believe that the effects of vaccination would be reduced by the fact that they are sexually active. Speculations, myths about infertility caused by the vaccine are indicated by one of the teenagers as a reason for refusal. Another teenager is convinced that despite the vaccination, infection is possible and thus believes that the vaccine is not necessary. Several teenage girls specify that their parents (especially the mother) do not agree with the vaccination.
Discussion
Most of the studies that address the subject of the hesitant behavior related to the HPV vaccination, discuss this problem from the perspective of the parents or the healthcare professionals, without taking into consideration what the teenagers want or think. This study’s purpose was to evaluate knowledge and attitude from the adolescents’ point of view, since they represent the target group for the HPV vaccination. In order to fight vaccine hesitancy and improve vaccination rates, interventions/strategies should be focused not only on parents, but also on adolescents. Hence, it is very important to understand the factors that can influence the decision regarding vaccination from their perspective.
This is why the study aimed to evaluate both knowledge and attitudes related to HPV infection, HPV vaccination, cervical cancer, as well as the reasons that could influence the decision related to vaccination in a population subgroup that can make an informed decision about vaccination, without parental consent. The secondary aim was to identify the main behavioral patterns regarding HPV vaccination in order to understand what determined the attitudinal differences. Following the analysis of the results for the two groups (GNV and GPV) of the study, there were significant differences between them in terms of perception and knowledge, in favor of GPV, which includes teenage girls more aware of the role and importance of HPV vaccination and more open to the idea of vaccination. For the GNV group or the hesitant group, the behavior can be explained by the fact that even if they have heard about the HPV infection being transmitted through unprotected sex and they think that vaccination in general is necessary to prevent certain diseases, adolescents in this group do not think or do not know if HPV vaccination would be effective in protecting them in the future. Also, the majority of teenagers in GNV have not heard about the HPV vaccine and its role in protecting against cervical cancer. As far as the GPV group or the non-hesitant group is concerned, the majority have heard about the HPV infection and think that vaccination is very important not only to protect themselves, but also their loved ones and the most important aspect, all of them declare they would accept HPV vaccination if it would be offered to them or they are already vaccinated (38 girls – 12.34% are already vaccinated in GPV, 5.51% if we relate to the entire sample).
The results of our study align with previous studies that mention the importance of HPV vaccination and the importance of launching educational and information campaigns regarding the risks of HPV infection.
Thus, it is very important to involve adolescents in the process of making a decision and to educate them in the sense of awareness of the importance of HPV vaccination in preventing not only infection, but most importantly, in preventing different forms of cancer.11 School seems to be the preferred environment for children and adolescents to discuss sexually transmitted infections, vaccines and vaccination, as they feel that here they can communicate without being judged; if the information is provided by people (teachers) whom they trust and admire, the attitude is favorable.12 The specialized literature highlights the fact that, by talking with adolescents about their fears related to the HPV vaccine, communicating in a language they understand, recommending the vaccine with confidence, medical professionals can definitely influence the decision regarding vaccination.13,21 70% of young people aged between 15 and 26 participating in a recent study, had knowledge about HPV vaccination and the association with cervical cancer; the main sources of information reported were similar to those in our study: those from the school (53%) or social environment (parents, friends – 20%), medical staff (23%), except for the internet, which was reported as a source of information by 32% of the teenagers in our study compared to 1% of young people from the cited study.22 On the other hand, the study carried out by Galvao et al highlighted the fact that the majority of adolescents (72.7%) do not have enough information about the HPV infection or the vaccine that prevents it, and 65.9% presented an unfavorable attitude related to the HPV vaccination.11 Also, in the study conducted by Zhang et al in adolescents aged 12–14 years, only 17.1% of the participants indicated that they had heard about the HPV vaccine; however, 67.3% of respondents expressed their willingness to get vaccinated. Adolescents who have heard about cervical cancer, HPV vaccines and those who understand the risk of the disease are the ones who expressed their intention to get vaccinated. 79.2% of teenagers recognized the fact that their parents’ opinion matters.23 The study conducted by Gomes et al highlighted that adolescents have a low level of knowledge about both HPV infection and the vaccine. Adolescents indicated school (39%), followed by TV/radio (38%) as the main source of vaccination information; parents were not indicated as an important source of information.24 Ramanadhan et al organized 6 focus groups, the participants being teenagers aged between 11 and 14 years and medical professionals. The main concerns expressed by teenagers were fear of injection and possible side effects. Potential adverse reactions were indicated as the main reason of concern in our study, as well. Also, as in the present study, adolescents expressed openness to receiving more information about HPV vaccination, preferably from a credible, authoritative source. Parents, doctors and the Internet were indicated as the main sources of information regarding HPV vaccination. Adolescents recognized that parents are the ones making medical decisions in general; this is also true for HPV vaccination.25
Adolescent participants in studies included in a systematic review reported dissatisfaction with the quality and quantity of information available about HPV vaccination. Also, some adolescents reported that they do not vaccinate because their parents do not agree (25% of adolescent girls in UK studies, 38.5% of adolescent girls participating in a German study).13,26 11% of the teenage girls included in a study carried out in 2015 in Romania declared that their parents consider HPV vaccination unsafe;13,27 49% of teenage girls in a UK study reported being influenced in making a decision by certain rumors about vaccination.13 Fernandes et al conducted a study on young women aged between 18 and 25 years; among the participants, 48.88% had received at least one dose of HPV vaccine, while 50% of the unvaccinated ones expressed their intention to get vaccinated. Lack of knowledge about vaccination, fear of possible side effects and the cost of the vaccine were the main reasons that stood in the way of vaccination intention. The doctor’s recommendation or recommendations from the social environment (parents, already vaccinated friends) influenced the decision. Most of the participants presented a positive attitude related to HPV vaccination.28
Dal Col Barthes et al conducted interviews with girls aged 11–14 years to assess knowledge, attitudes, perceptions related to HPV infection and HPV vaccination. The study highlights a positive attitude and a good level of knowledge in girls aged over 12, from the urban environment. The role of the family doctor and parents in the decision regarding vaccination is emphasized here as well.29 Vaidakis et al conducted a national study (Greece) involving 4547 adolescents with a mean age of 17 years; 42.8%, respectively 75.5% of them knew about HPV infection, respectively about cervical cancer, but 60.60% did not know that there is a link between infection and cancer. More than half (60.0%) of the participants had not heard of the HPV vaccine and only 10.2% of the girls were already vaccinated against HPV.30 Another study highlights a low level of knowledge among adolescents, as well as a low vaccination rate caused by fear of possible side effects and lack of information.31
Loke et al conducted a literature review to assess factors influencing the acceptability of HPV vaccination among adolescents.32–34 The main factors that affected the intention to vaccinate were parents’ attitude and opinion about vaccination, fear of potential side effects, lack of recommendation by a medical professional.26,32 Most teenagers have heard of cervical cancer (between 69% and 95.9%); also, 81% of the adolescent girls involved knew that HPV infection is a risk factor for cervical cancer.32,35 Restivo et al conducted a study on a sample that included young women with an average age of 19, to evaluate the factors that are associated with the refusal of HPV vaccination; 15.6% of the participants were vaccinated with at least one dose, and 11.3% declared that they had experienced a sexually transmitted infection. The pediatrician/family doctor was indicated as the main source of information regarding vaccination by 42.5% of the participants, the gynecologist by 33.3% and the parents by 24.8%. The main reasons that determined the refusal of vaccination were lack of information (39.5%), fear of adverse reactions (33.6%), lack of confidence in the effectiveness of vaccines and logistical reasons (vaccination center far from home, lack of time) – 11.8%.12 The systematic review by Iliadou et al included studies that assessed knowledge, attitude, willingness to vaccinate, among adolescents and young adults, in an attempt to identify interventions needed to increase vaccination acceptability and vaccination rates. Most studies (9 out of 10) show low to moderate levels of knowledge about vaccination, while one study shows increased levels of knowledge. Vaccination-related attitudes and intentions were generally positive.36 Another systematic review highlights that adolescents’ intention to get vaccinated is affected by lack of knowledge about HPV infection, HPV vaccination or cervical cancer; some adolescents reported some reluctance to discuss these matters with parents or medical staff; also, many feel that vaccination is not necessary because they do not consider themselves at risk of infection. Also, as in our study, the main reason why young people included in these studies show hesitant behavior or refuse HPV vaccination is represented by concerns about possible side effects. The negative attitude related to vaccination, namely the parents’ recommendation not to vaccinate, decisively influences the intention.37
Thanasas et al highlight the fact that adolescents from urban areas have a higher level of knowledge compared to those from rural areas and are more determined to get vaccinated.38 Kiener et al conducted a study that included participants between the ages of 15–26 years, to assess the effect of hesitant behavior on vaccination rates. The authors reported a significant association between hesitancy and low vaccination rates in the adolescent and young women included in the study.39 The systematic review carried out by Lopez et al highlights a very large difference between studies regarding the knowledge about vaccination of adolescents (from 5.2% to 94%);40–42 and of parents.40,43 Adolescents reported school as the main source of information regarding HPV infection, while parents turn to the pediatrician; if we talk about the HPV vaccine, both adolescents and parents trust the medical staff.40,44 Between 7.7% and 32.5% of adolescents, depending on the study, expressed concern about the safety of HPV vaccination; as for parents, between 7.9% and 68.1% of them were concerned about this aspect, as well as encouraging sexual activity through HPV vaccination (between 10.5% and 42%).40,45,46 Up to 43% of adolescents, respectively 73.4% of parents, consider the vaccine effective in preventing diseases associated with HPV infection.40,47
Similar studies published between 2021 and 2023 highlight the importance of national information and education campaigns addressed to parents, but also to the general population.48,49
Public health programs and health promotion campaigns that educate the target group have been shown to have a positive effect on adolescent attitudes, but must be matched with accurate and effective information.11–13,50–53
Limitations of the study: it was carried out on a sample from a single county, on a certain age group, in the absence of a standardized questionnaire to assess the attitude related to HPV vaccination. A national or multiregional approach would be preferred, because in other regions of Romania the level of awareness and education of teenagers could be different. On the other hand, the study can form the basis for the implementation of interventions to educate adolescents regarding the importance of HPV vaccination and its crucial role in preventing cervical cancer. The analysis was carried out not on a single sample, but on two groups and compared knowledge and attitude in adolescents with a hesitant behavior and in those that intent to get vaccinated or are already vaccinated.
Conclusions
Most of the adolescent girls included in the present study (55.36%) show a hesitant behavior when faced with a decision regarding vaccination. The study also highlights the fact that teenage girls with a low level of knowledge and negative perceptions about vaccination are the ones prone to hesitating behavior. The large differences identified between the level of knowledge and the attitude regarding the HPV vaccination in the two groups underline the need for health education strategies addressed to the young generation. Improving the level of knowledge of adolescents about HPV infection and HPV vaccination, by training and involving school doctors, teachers, by introducing into the school curriculum of some courses on immunization in general and on HPV vaccination in particular, by organizing campaigns of information in schools, campaigns involving professionals in the field (epidemiologists, public health doctors, other specialists), is critical in order to address hesitant behavior and improve vaccination rates. This way, we can favorably influence attitudes and intentions related to HPV vaccination. Informed teenagers, in turn, will be able to positively influence their parents, and at the right time, they can make the right decisions about vaccinating their own children, the long-term benefits for the community being inestimable.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Oradea County Emergency Clinical Hospital – approval no. 1534 of 17.01.2019.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Consent for Publication
Authors have read and agreed to the published version of the manuscript.
Funding
This research received funding from the University of Oradea.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. World Health Organization. WHO updates recommendations on HPV vaccination schedule. Available from: https://www.who.int/news/item/20-12-2022-WHO-updates-recommendations-on-HPV-vaccination-schedule. Accessed August 1, 2023.
2. Bruni L, Serrano B. Putting HPV on the Map: The State of HPV Prevention Programs in the WHO European Region. Brussels: European Cancer Organization; 2022.
3. Health Ministry Order 1755 /2021 for the amendment of annex no. 2 to the technical norms for the realization of the national public health programs for the years 2017 and 2018, approved by the order of the Minister of Health no. 377/2017; 2022 Available from: https://legislatie.just.ro/Public/DetaliiDocumentAfis/246044. Accessed 4 September 2023.
4. Health Ministry Order no. 964 of March 31, 2022 regarding the approval of the technical norms for the implementation of national public health programs; 2023 Available from: https://legislatie.just.ro/Public/DetaliiDocument/253543. Accessed 4 September 2023.
5. Clarifications regarding the conduct of the HPV vaccination campaign – “The HPV vaccination campaign, without discontinuity”. Available from: http://www.ms.ro/. Accessed November 12, 2022.
6. The Ministry of Health starts the information campaign for cervical cancer prevention through vaccination. Available from: http://www.old.ms.ro/. Accessed November 12, 2022.
7. National Institute of Public Health. National center for the surveillance and control of communicable diseases: methodological letter on HPV vaccination; 2022.
8. Di Lorenzo A, Bianchi FP, Martinelli A, et al. Safety profile of recommended vaccinations in adolescents: data from surveillance of adverse events following immunization in Puglia (Italy), 2016–2020. Vaccines. 2021;9:1302. doi:10.3390/vaccines9111302
9. Cadeddu C, Castagna C, Sapienza M, et al. Understanding the determinants of vaccine hesitancy and vaccine confidence among adolescents: a systematic review. Hum Vaccin Immunother. 2021;17:4470–4486. doi:10.1080/21645515.2021.1961466
10. Yang YT, Olick RS, Shaw J. Adolescent consent to vaccination in the age of vaccine-hesitant parents. JAMA Pediatr. 2019;173:1123–1124. doi:10.1001/jamapediatrics.2019.3330
11. Galvão MPSP, Araújo TME, Rocha SSD. Knowledge, attitudes, and practices of adolescents regarding human papillomavirus. Rev Saude Publica. 2022;56:12. doi:10.11606/s1518-8787.2022056003639
12. Restivo V, Costantino C, Fazio TF, et al. Factors associated with HPV vaccine refusal among young adult women after ten years of vaccine implementation. Int J Environ Res Public Health. 2018;2018(15):770. doi:10.3390/ijerph15040770
13. Karafillakis E, Simas C, Jarrett C, et al. HPV vaccination in a context of public mistrust and uncertainty: a systematic literature review of determinants of HPV vaccine hesitancy in Europe. Hum Vaccin Immunother. 2019;15:1615–1627. doi:10.1080/21645515.2018.1564436
14. World Health Organisation. Cervical cancer. Available from: https://www.who.int/newsroom/factsheets/detail. Accessed November 12, 2022.
15. World Health Organization Regional Committee for Europe. 72nd session roadmap to accelerate the elimination of cervical cancer as a public health problem in the WHO European Region 2022–2030; 2022.
16. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71:209–249. doi:10.3322/caac.21660
17. Bruni L, Albero G, Serrano B, et al. ICO/IARC information centre on HPV and cancer (HPV information centre). Human Papillomavirus and Related Diseases in the World; 2021.
18. European Centre for Disease Prevention and Control. Guidance on HPV Vaccination in EU Countries: Focus on Boys, People Living with HIV and 9-Valent HPV Vaccine Introduction, 2020. Stockholm: ECDC; 2020.
19. Zur Hausen H. Papillomaviruses in the causation of human cancers – a brief historical account. Virology. 2009;384:260–265. doi:10.1016/j.virol.2008.11.046
20. World Health Organisation. Weekly Epidemiological Record (WER). Wkly Epidemiol Rec. 2022;97:453–464.
21. Leung SOA, Akinwunmi B, Elias KM, Feldman S. Educating healthcare providers to increase Human Papillomavirus (HPV) vaccination rates: a qualitative systematic review. Vaccine X. 2019;3:100037. doi:10.1016/j.jvacx.2019.100037
22. Schwendener CL, Kiener LM, Jafflin K, et al. HPV vaccine awareness, knowledge and information sources among youth in Switzerland: a mixed methods study. BMJ Open. 2022;12:e054419. doi:10.1136/bmjopen-2021-054419
23. Zhang X, Wang Z, Ren Z, et al. HPV vaccine acceptability and willingness-related factors among Chinese adolescents: a nation-wide study. Hum Vaccin Immunother. 2021;17:1025–1032. doi:10.1080/21645515.2020.1812314
24. Gomes JM, Silva BM, Santos EFS, et al. Human Papillomavirus (HPV) and the quadrivalent HPV vaccine among Brazilian adolescents and parents: factors associated with and divergences in knowledge and acceptance. PLoS One. 2020;15:e0241674. doi:10.1371/journal.pone.0241674
25. Ramanadhan S, Fontanet C, Teixeira M, Mahtani S, Katz I. Exploring attitudes of adolescents and caregivers towards community-based delivery of the HPV vaccine: a qualitative study. BMC Public Health. 2020;20:1531. doi:10.1186/s12889-020-09632-2
26. Stocker P, Dehnert M, Schuster M, Wichmann O, Delere Y. Human papillomavirus vaccine uptake, knowledge and attitude among 10th grade students in Berlin, Germany, 2010. Hum Vaccin Immunother. 2013;9:74–82. doi:10.4161/hv.22192
27. Maier C, Maier T, Neagu CE, Vledereanu R. Romanian adolescents’ knowledge and attitudes towards human papillomavirus infection and prophylactic vaccination. Eur J Obstet Gynecol Reprod Biol. 2015;195:77–82. doi:10.1016/j.ejogrb.2015.09.029
28. Fernandes R, Potter BK, Little J. Attitudes of undergraduate university women towards HPV vaccination: a cross-sectional study in Ottawa, Canada. BMC Womens Health. 2018;18:134. doi:10.1186/s12905-018-0622-0
29. Dal Col Barthès S, Dumoitier N, Rudelle K. Perceptions and feelings of young girls regarding vaccination against papillomavirus. Med Mal Infect. 2020;50:723–726. doi:10.1016/j.medmal.2020.02.007
30. Vaidakis D, Moustaki I, Zervas I, et al. Knowledge of Greek adolescents on human papilloma virus (HPV) and vaccination: a national epidemiologic study. Medicine. 2017;96:e5287. doi:10.1097/MD.0000000000005287
31. Anagnostou PA, Aletras VH, Niakas DA. Human papillomavirus knowledge and vaccine acceptability among adolescents in a Greek region. Public Health. 2017;152:145–152. doi:10.1016/j.puhe.2017.07.033
32. Loke AY, Kwan ML, Wong YT, Wong AKY. The uptake of human papillomavirus vaccination and its associated factors among adolescents: a systematic review. J Prim Care Community Health. 2017;8:349–362. doi:10.1177/2150131917742299
33. Lee A, Ho M, Cheung CK, Keung VM. Factors influencing adolescent girls’ decision in initiation for human papillomavirus vaccination: a cross-sectional study in Hong Kong. BMC Public Health. 2014;14:925. doi:10.1186/1471-2458-14-925
34. Johnson KL, Lin MY, Cabral H, Kazis LE, Katz IT. Variation in human papillomavirus vaccine uptake and acceptability between female and male adolescents and their caregivers. J Community Health. 2017;42:522–532. doi:10.1007/s10900-016-0284-5
35. Mollers M, Lubbers K, Spoelstra SK, et al. Equity in human papilloma virus vaccination uptake? Sexual behaviour, knowledge and demographics in a cross-sectional study in (un)vaccinated girls in the Netherlands. BMC Public Health. 2014;14:288. doi:10.1186/1471-2458-14-288
36. Iliadou M, Sahini K, Sakellari E, et al. What do Young people think about HPV and HPV vaccination? The role of health education interventions and health professionals. Mater Sociomed. 2021;33:219–224. doi:10.5455/msm.2021.33.219-224
37. Zheng L, Wu J, Zheng M. Barriers to and facilitators of human papillomavirus vaccination among people aged 9 to 26 years: a systematic review. Sex Transm Dis. 2021;48:e255–e262. doi:10.5455/msm.2021.33.219-224
38. Thanasas I, Lavranos G, Gkogkou P, Paraskevis D. The effect of health education on adolescents’ awareness of HPV infections and attitudes towards HPV vaccination in Greece. Int J Environ Res Public Health. 2022;19(503):503. doi:10.3390/ijerph19010503
39. Kiener LM, Schwendener CL, Jafflin K, et al. Vaccine hesitancy and HPV vaccine uptake among male and female youth in Switzerland: a cross-sectional study. BMJ Open. 2022;12:e053754. doi:10.1136/bmjopen-2021-053754
40. López N, Garcés-Sánchez M, Panizo MB, et al. HPV knowledge and vaccine acceptance among European adolescents and their parents: a systematic literature review. Public Health Rev. 2020;41:10. doi:10.1186/s40985-020-00126-5
41. Hoglund AT, Tyden T, Hannerfors T, Larsson M. Knowledge of HPV and attitudes to HPV vaccination among Swedish high school students. Eur J Contracept Reprod Heal Care. 2010;15:53.
42. Samkange-Zeeb F, Spallek L, Klug SJ, Zeeb H. HPV infection awareness and self-reported HPV vaccination coverage in female adolescent students in two German cities. J Community Health. 2012;37:1151–1156. doi:10.1007/s10900-012-9589-1
43. Navarro-Illana P, Caballero P, Tuells J, Puig-Barberá J, Diez-Domingo J. Aceptabilidad de la vacuna contra el virus del papiloma humano en madres de la provincia de Valencia (España). Ann Pediatr. 2015;83:318–327. Spanish. doi:10.1016/j.anpedi.2014.11.018
44. Bianco A, Pileggi C, Iozzo F, Nobile CGA, Pavia M. Vaccination against human papilloma virus infection in male adolescents: knowledge, attitudes, and acceptability among parents in Italy. Hum Vaccin Immunother. 2014;10:2536–2542. doi:10.4161/21645515.2014.969614
45. Grandahl M, Tydén T, Westerling R, et al. To consent or decline HPV vaccination: a pilot study at the start of the national school-based vaccination program in Sweden. J Sch Health. 2017;87:62–70. doi:10.1111/josh.12470
46. Voidazan S, Tarcea M, Morariu S-H, Grigore A, Dobreanu M. Human papillomavirus vaccine—knowledge and attitudes among parents of children aged 10–14 years: a cross-sectional study, Tirgu Mures, Romania. Cent Eur J Public Health. 2016;24(24):29–38. doi:10.21101/cejph.a4287
47. Oddsson K, Gudmundsdottir T, Briem H. Attitudes and knowledge among parents or guardians of 12-year-old girls about HPV vaccination—a population-based survey in Iceland. Eur J Gynaecol Oncol. 2016;37:837–841. doi:10.12892/ejgo3310.2016
48. Aimagambetova G, Babi A, Issa T, Issanov A. What factors are associated with attitudes towards HPV vaccination among Kazakhstani women? Exploratory analysis of cross-sectional survey data. Vaccines. 2022;10(5):824. doi:10.3390/vaccines10050824
49. Issa T, Babi A, Issanov A, et al. Knowledge and awareness of human papillomavirus infection and human papillomavirus vaccine among Kazakhstani women attending gynecological clinics. PLoS One. 2021;16(12):e0261203. doi:10.1371/journal.pone.0261203
50. Russu OM, Strnad G, Jakab-Farkas L, et al. Electrochemical synthesis of nanostructured oxide layers on threaded surfaces of medical implants. Rev Chim. 2018;69(7):1636–1639. doi:10.37358/RC.18.7.638
51. Pop TS, Pop AM, Miron ADT, Brinzaniuc K, Gurzu S, Trambitas C. In vivo evaluation of a collagen scaffold preconditioned with adipose-derived mesenchymal stem cells used for bone regeneration A histological study. Mater Plast. 2018;55(4):691–695. doi:10.37358/MP.18.4.5102
52. Popa Z, Chiriac VD, Cobec IM, et al. HPV cervical cancer screening. An analysis over HPV markers between worldwide statistics and Romanian reality. Rev Chim. 2017;68(10):2459–2462. doi:10.37358/RC.17.10.5905
53. Mensch K, Szarka K, Mensch H, et al. PCR technique assisting the early diagnosis of human papillomavirus A retrospective clinical study. Rev Chim. 2018;69(10):2781–2787. doi:10.37358/RC.18.10.6624