Infection
Risk predict model using multi-drug resistant organism infection from Neuro-ICU patients: a retrospective cohort study
Abstract
The aim of this study was to analyze the current situation and risk factors of multi-drug-resistant organism (MDRO) infection in Neuro-intensive care unit (ICU) patients, and to develop the risk predict model. The data was collected from the patients discharged from Neuro-ICU of grade-A tertiary hospital at Guizhou province from January 2018 to April 2020. Binary Logistics regression was used to analyze the data. The model was examined by receiver operating characteristic curve (ROC). The grouped data was used to verify the sensitivity and specificity of the model. A total of 297 patients were included, 131 patients infected with MDRO. The infection rate was 44.11%. The results of binary Logistics regression showed that tracheal intubation, artery blood pressure monitoring, fever, antibiotics, pneumonia were independent risk factors for MDRO infection in Neuro-ICU (P < 0.05), AUC = 0.887. The sensitivity and specificity of ROC curve was 86.3% and 76.9%. The risk prediction model had a good predictive effect on the risk of MDRO infection in Neuro ICU, which can evaluate the risk and provide reference for preventive treatment and nursing intervention.
Introduction
Intensive care unit (ICU) is a gathering place for patients with acute and critical illness. In recent years, with the increase in the incidence of stroke and traumatic brain injury (TBI), Neuro-ICU has gradually developed and become an ICU specialized in treating neurological problems1,2. Due to the higher antibiotic use rate and more invasive treatments in critically ill patients, the problem of multi-drug-resistant organism (MDRO) has become more prominent3,4,5.
Multidrug-resistant organisms refer to organisms resistant to one or more classes of antimicrobials, and these bacteria are often resistant to most available antimicrobial agents6,7. MDRO infection is complex and difficult to treat, and it is easy to cause an outbreak of nosocomial infection. MDRO nosocomial infection not only prolongs the number of hospitalization days for patients, but also increases the hospitalization costs of patients. These are bringing a huge economic burden to patients, and more serious nosocomial infection in the ICU affects the success rate of critically ill patients and increases the mortality rate of ICU patients8,9. Therefore, the management of MDRO has gradually become an important part of hospital infection control.
Due to its particularity, Neuro-ICU patients have longer recovery time and longer hospital stay. Studies have shown that the hospital stay of TBI patients was about 19.4 ± 13.9 days10. Studies have shown that there is a correlation between the length of stay in the ICU and the infection rate of MDRO11, the prevalence of infections acquired in Intensive Care Units (ICU) is higher than it is in other hospital units12, ICU MDRO infection rate can be as high as 50%13. The incidence of MDRO infections in the neuro ICU is high14, but studies are still relatively limited. Therefore, the prevention and control of Neuro-ICU MDRO infection become an urgent problem to be solved, and prevention is the most economical and effective way to control MDRO infection.
The purpose of this study was to explore the high-risk factors for MDRO infection, establish a Neuro-ICU MDRO nosocomial infection transmission risk model, propose targeted infection prevention and control measures, and reduce the transmission and infection of MDRO in a timely and effective manner, thus preventing an outbreak of MDRO infection.
Methods
Study design and population
Risk factors related to infection of multi-drug-resistant organism in Neuro-ICU patients were investigated by searching Chinese and foreign literatures, consulting critical care experts, conducting a group discussion, designing and modifying the data collection items, including: ①General demographic information, such as gender, age, etc. ②Treatment Circumstances, such as invasive operation, level of consciousness, etc. ③Laboratory indicator and the patient’s own physical conditions. Researchers grouped patients by whether they were infected or colonized with multi-drug resistant organism.
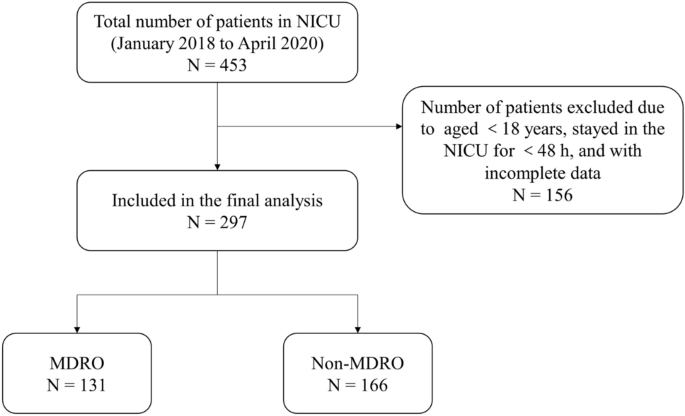
The study was a single-center, retrospective study. The cluster sampling method was used to collect relevant data of all consecutive patients of Neuro-ICU in the Third Affiliated Hospital of Zunyi Medical University from January 1, 2018 to April 30, 2020. Inclusion criteria included: ①Patients aged ≥ 18 years. ②Patients staying in the ICU for ≥ 48 h. ③Patients who were transferred to the general ward after being transferred from the ICU. Exclusion criteria: patients with incomplete data or an MDRO infection has occurred. In this study, univariate and multivariate analysis were used to screen risk factors. A total of 297 patients were included in this study (Fig. 1).
Patient enrollment flow chart.
Data Collection
In this study, we retrospectively investigated the hospital’s Neuro-ICU patient entry and exit registration form, electronic medical record system, nursing document system, and medical record file to obtain the required information. All data were collected before the diagnosis of MDRO infection, GCS score and albumin level were collected as the first test results of patients transferred to ICU. Combination of antibiotics refers to patients received two or more antibiotics at the same time. Antibiotics are drugs used to treat various bacterial or infections inhibit infection by pathogenic microorganisms, including all antibiotics such as sulfonamides, quinolones and β-lactam antibiotics. All data were double-entered using Excel2016 software. To determine whether patients are infected with MDROs, aseptically collected sputum, blood, cerebrospinal fluid, and midstream urine samples were collected from them conventionally. The criteria for determining MDROs have been developed according to the 2010 international standardized definition of MDROs jointly proposed by the United States and other countries15.
Ethical considerations
This study was approved by the Ethics Committee of The Third Affiliated Hospital of Zunyi Medical University (The First People’s Hospital of Zunyi) (2017–215). As the patient information was anonymized and deidentified before analysis, the ethics committee of the First People’s Hospital of Zunyi waived the need for informed consent. And all methods were performed following the Declaration of Helsinki.
Statistical analysis
SPSS 20.0 software was used for statistical processing, measurement data was expressed by independent sample t test or non-parametric rank sum test, count data was expressed by frequency and rate, and chi-square test was used; binary Logistics regression was used to obtain risk factors for MDRO infection and build a prediction model, the ROC curve was drawn with sensitivity as the ordinate and (1-specificity) as the abscess coordinate, and the prediction effect of the model was verified. P < 0.05 indicated that the difference was statistically significant.
Ethical approval and consent to participate
This research was approved by the Ethics Committee of the The Third Affiliated Hospital of Zunyi Medical University (The First People’s Hospital of Zunyi) (2017-215). As the patient information was anonymized and deidentified before analysis, informed consent was not needed.
Results
General data and MDRO infection
This study was included 297 patients’ information, including 206 patients (69.4%), 91 female (30.7%), age distribution at 18–95 (56.79 ± 16.057), of which 131 patients have MDRO infections. The infection rate was 44.11%. Among the 131 patients infected, 106 (80.92%) were infected with 1 bacterium, 25 (19.08%) infected 2 and more bacteria. The top five bacteria were detected as Acinetobacter baumannii (44, 33.59%), Klebsiella pneumoniae (39, 29.77%), Pseudomonas pyocyaneum (22, 16.79%), Methicillin-resistant Staphylococcus aureus (8, 6.1%), Escherichia coli (7, 5.34%).
Construction of risk prediction model
In this study, 297 patients were used for the construction of risk prediction models. The results of single factor analysis showed that the difference between age, medical insurance, admission, diagnosis between two groups were significant, and the remaining factors were statistically significant (P < 0.05) (Table 1). In contrast, the variable was used as a variable in a single factor analysis, which uses binary logistics regression analysis. The results show that tracheal intubation, artery blood pressure monitoring, fever, antibiotics, pneumonia were found as independent risk factors of multiple drug-resistant bacteria infections, predictive model formulas: P = 1/1 + exp (−Z). This prediction model was used as z = 1.815 × tracheal inhibition + 2.012 × artery blood pressure monitoring + 1.650 × fever + 2.087 × antibiotics + 1.750 × pneumonia + (-0.83 × albumin) (Table 2).
Risk prediction model fitting test
The results of HOSMER and LEMESHOW test (P = 0.831) were indicated that the model can better interact with the actual occurrence of MDRO infections. The truncation value was calculated by the predictive model formula used as the test variable, and whether it returns to the state variable ROC curve. Figure 2 showed the area of the ROC curve (AUC) = 0.887, 95% CI (0.849, 0.925), P < 0.001 was indicated the predicted effect of this prediction model was very good. In this study, the maximum value of Youden index was used to judge the optimal critical value of the predictive model, the maximum value of Youden index was about 0.652, and the sensitivity was of ROC curve was 86.3%, the specificity was 78.9%, and the cutoff value was 0.476.

ROC curve of MDRO infection prediction model.
Discussion
This study aimed to clarify the influencing factors of MDRO infection in Neuro-ICU, and further construct predict models according to the influencing factors. A total of 297 patients admitted in Neuro-ICU were included in this study, our analysis identified risk factors for MDRO infection, and we developed predictive models using these risk factors.
Our study found that Acinetobacter baumannii, Klebsiella pneumoniae, and Pesudomonas pyocyaneum were the most common pathogens in Neuro-ICU. Recent study showed that Acinetobacter baumannii was found as most frequent bacteria16,17. Among nosocomial infection and colonization, 76% of the bacterial infections were due to Gram-negative bacteria. A. baumannii, Enterobacteriaceae species and P. aeruginosa strains were the main isolated bacteria12. Yang et al.18 also reported that gram negative (GN) bacteria were more common than gram positive (GP) bacteria predominated in central nervous system (CNS) infections, and our study was a little different from previous research results. Pseudomonas pyocyaneum was found as one of the main bacteria in Neuro-ICU. Our results showed that the incidence of MRSA was low, this was similar to the research results of El Mekes et al.12. There are many studies related to ICU MDRO infection rate, and the results have large value fluctuation range, a Chinese study stated MDRO prevalence rate on admission in ICU was 30.5%19.
The present study found that MDRO infections were not uncommon in Neuro-ICU, although this study did not clarify the specific MDRO infection rate, among the study subjects included, the number of patients infected or colonized with MDRO has exceeded 44%, which is extremely high. However, this data did not represent the overall situation of Neuro-ICU. The subjects of our study were patients who entered the ICU and were transferred out. Some patients had been transferred to other hospitals or died during the ICU hospitalization process, so in this study we could not calculate the exact infection rate. However, there is still insufficient evidence for the MDRO infection rate in the Neuro ICU, and more studies are needed to confirm it.
Our study resulted in good predictive models with accuracies of 86.3% using logistic regression. In our study, we found that tracheal intubation, artery blood pressure monitoring, fever, antibiotics, pneumonia are significant predictors for MDRO infection. The use of antibiotics (OR: 8.064) was the most important factor in MDRO infection. In the current state of knowledge, there are few predictive models of MDROs infections in neuro-intensive care units. Minhas et al.20 modeled prediction through decision trees, and our predictive efficacy is similar to this study. Our study differed significantly from another Chinese study21, which examined a model to predict pulmonary infection of multidrug-resistant Acinetobacter baumannii in Neuro-ICU. This may be because we pooled and analyzed a variety of infections rather than pulmonary infection in our study.
The amount of antibiotic use of severe patients is significantly higher than those of ordinary ward. Due to the resistance or infection, antibiotics are often used in combination. It was found that antibiotics and combination of antibiotics are related to MDRO infection in univariate analysis. However, only antibiotic therapy is an independent risk factor of MDRO infection in the multiple logistic regression model. In Neuro-ICU, the majority patient’s primary disease types are traumatic brain injury or stroke, and the pneumonia incidence of two diseases is high22,23. Using mechanical ventilation will aggravate the incidence of pneumonia24.
The use of antibiotics to treat pneumonia is prone to the occurrence and propagation of multi-drug resistant organism25,26,27. A Meta-analysis has clearly been applying antibiotics in advance to risk factors for MDRO infection28. Our research further verified this view. In order to increase the cure rate of multi-drug bacteria, medical staff tend to use antibiotics to enhance the utility of drugs27. It may exacerbate this process. In addition, in this study, fever was also one of the risk factors of MDRO infection, critically ill patients may have a variety of reasons, and fever may be caused by patient’s pneumonia. Among the patients with MDRO infection or planting, 89.31% of patients had pneumonia, while non-MDRO patients were also as high as 56.02%.
Recent studies have shown that the severity of trauma does not affect the incidence of MDRO, the incidence of MDRO in severely injured patients is lower than in ICU29,30,31. The type of admission and disease can indicate the severity of patients, in our results, GCS scores cannot ultimately predict MDRO infection, so our research indicates that MDRO infection is not associated with the severity of disease, this may be caused by autoimmune and early application of antibiotics in patients with acute trauma32.
The results for risk factors were consistent with previous studies in the use of invasive operation24,33,34. In our study, persistent artery blood pressure monitoring and tracheal intubation were two invasive appliances associated with MDRO infection, such invasive operations destroy normal physiological integrity and local immune function. Our research results were different from the past. In the past, urinary tube and feeding tubes were the main indwelling instruments of MDRO infection34,35. Due to the particularity of neurological patients, almost all patients will remain in these two types of piping, so we did not incorporate these two invasive operations.
Furthermore, we found an association between positive MDRO and albumin level, there is a literature pointed out that the lower the serum albumin level, the higher the risk of patient infection36, our research further verified this conclusion. The average age of the patients included in our study was older, and both the patients themselves and the disease caused malnutrition and hypoproteinemia. Despite the study showed allogenic blood transfusions cause immune modulation and have a negative influence on the immune system and may result in increased infections with MDRO37. However, blood transfusion still cannot be used as a predictive variable, although patients with anemia or low nutritious states are worthy of attention, because this type of patient is a high-risk population of MDRO infection.
However, in our study, there were no correlation between the gender, age, medical insurance with MDRO infection. There were many studies had shown that age and gender were not associated with acquired MDRO38,39. A recent research indicated MDRO that infections were numerically associated with the female sex, greater age, and comorbidities40. These factors may require more research to further confirm the correlation.
Future clinical practice should reinforce multidisciplinary coordination so that physicians, pharmacists, and nurses play a more active role in patient care. The screening of patients for multidrug-resistant bacteria in the neurologic intensive care unit should be a routine part of the treatment of patients after admission. In the process of stepping and standardizing the medication regimen of patients, pharmacists should serve as a guide. Physicians and pharmacists will work together in the future to pursue and develop therapeutic medications41,42,43. Nurses are essential components of clinical practice and should play a full role in preventing MDROs and managing them on a daily basis. A high incidence of MDROs in Neuro-ICU makes multidisciplinary work necessary for effective prevention and management of MDRO infections.
There were several limitations in our study. First, this was a retrospective study of a single center, the researchers only collected patient data in a tertiary, a hospital in one province, and the data cannot represent the actual situation in the region or the whole country, and there may be bias. Second, there were less research samples, compared with the comprehensive ICU, Neuro-ICU has a smaller patient population, and the researchers only collected data for the past two years. Finally, although there was established a predictive model based on risk factors, there was no further verification of prediction model, and the impact of the risk prediction model on the actual incidence of MDRO infection in Neuro-ICU patients was not investigated.
Conclusion
This study constructed a predictive model with 6 variables, and the patients with higher risk would be screened (Fig. 3). The establishment of an ICU MDRO infection risk prediction model can eliminate the blindness of MDRO infection or colonization treatment, so that medical staff can more rationally and effectively use relevant resources, and timely, accurately and comprehensively grasp the changes of patients. Targeted implementation of preventive measures for patient use, and ultimately prevent MDRO nosocomial infection.

A simplified schematic diagram representing risk predict model using multi-drug resistant organism infection from Neuro-ICU patients.
Data availability
The original contributions presented in the study are included in the supplementary material, further inquiries can be directed to the corresponding author.
References
-
Badenes, R., Robba, C., Taccone, F. S. & Bilotta, F. Neuro-ICU patient disposition: Optimal venue for acute needs. Curr. Opin. Crit. Care 24, 65–71. https://doi.org/10.1097/mcc.0000000000000482 (2018).
Google Scholar
-
Beghi, E. et al. Acute and post-acute neurological manifestations of COVID-19: Present findings, critical appraisal, and future directions. J. Neurol. 269, 2265–2274. https://doi.org/10.1007/s00415-021-10848-4 (2022).
Google Scholar
-
Jarrell, A. S., Kruer, R. M., Berescu, L. D., Pronovost, P. J. & Trivedi, J. B. Factors associated with in-hospital mortality among critically ill surgical patients with multidrug-resistant gram-negative infections. J. Crit. Care 43, 321–326. https://doi.org/10.1016/j.jcrc.2017.10.035 (2018).
Google Scholar
-
Al-Sunaidar, K. A., Aziz, N. A., Hassan, Y., Jamshed, S. & Sekar, M. Association of multidrug resistance bacteria and clinical outcomes of adult patients with sepsis in the intensive care unit. Trop. Med. Infect. Dis. https://doi.org/10.3390/tropicalmed7110365 (2022).
Google Scholar
-
Thoma, R. et al. The challenge of preventing and containing outbreaks of multidrug-resistant organisms and Candida auris during the coronavirus disease 2019 pandemic: Report of a carbapenem-resistant Acinetobacter baumannii outbreak and a systematic review of the literature. Antimicrob. Resist. Infect. Control 11, 12. https://doi.org/10.1186/s13756-022-01052-8 (2022).
Google Scholar
-
Siegel, J. D., Rhinehart, E., Jackson, M. & Chiarello, L. Management of multidrug-resistant organisms in health care settings, 2006. Am. J. Infect. Control 35, S165-193. https://doi.org/10.1016/j.ajic.2007.10.006 (2007).
Google Scholar
-
Hidron, A. I. et al. NHSN annual update: Antimicrobial-resistant pathogens associated with healthcare-associated infections: Annual summary of data reported to the National Healthcare Safety Network at the Centers for Disease Control and Prevention, 2006–2007. Infect. Control Hosp. Epidemiol. 29, 996–1011. https://doi.org/10.1086/591861 (2008).
Google Scholar
-
Huang, J. et al. Impact of multicenter unified enhanced environmental cleaning and disinfection measures on nosocomial infections among patients in intensive care units. J. Int. Med. Res. 48, 300060520949766. https://doi.org/10.1177/0300060520949766 (2020).
Google Scholar
-
Maia, M. O. et al. Multidrug-resistant bacteria on critically ill patients with sepsis at hospital admission: Risk factors and effects on hospital mortality. Infect. Drug Resist. 16, 1693–1704. https://doi.org/10.2147/idr.S401754 (2023).
Google Scholar
-
Lazaridis, C., Yang, M., DeSantis, S. M., Luo, S. T. & Robertson, C. S. Predictors of intensive care unit length of stay and intracranial pressure in severe traumatic brain injury. J. Crit. Care 30, 1258–1262. https://doi.org/10.1016/j.jcrc.2015.08.003 (2015).
Google Scholar
-
Phu, V. D. et al. Burden of hospital acquired infections and antimicrobial use in Vietnamese adult intensive care units. PLoS ONE 11, e0147544. https://doi.org/10.1371/journal.pone.0147544 (2016).
Google Scholar
-
El Mekes, A., Zahlane, K., Ait Said, L., Tadlaoui Ouafi, A. & Barakate, M. The clinical and epidemiological risk factors of infections due to multi-drug resistant bacteria in an adult intensive care unit of University Hospital Center in Marrakesh-Morocco. J. Infect. Public Health 13, 637–643. https://doi.org/10.1016/j.jiph.2019.08.012 (2020).
Google Scholar
-
Viderman, D. et al. An observational case study of hospital associated infections in a critical care unit in Astana, Kazakhstan. Antimicrob. Resist. Infect. Control 7, 57. https://doi.org/10.1186/s13756-018-0350-0 (2018).
Google Scholar
-
Kuzina, E. S. et al. Rectal and tracheal carriage of carbapenemase genes and class 1 and 2 integrons in patients in neurosurgery intensive care unit. Antibiotics (Basel) https://doi.org/10.3390/antibiotics11070886 (2022).
Google Scholar
-
Magiorakos, A.-P. et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 18, 268–281 (2012).
Google Scholar
-
Ayobami, O. et al. The incidence and prevalence of hospital-acquired (carbapenem-resistant) Acinetobacter baumannii in Europe, Eastern Mediterranean and Africa: A systematic review and meta-analysis. Emerg. Microbes. Infect. 8, 1747–1759. https://doi.org/10.1080/22221751.2019.1698273 (2019).
Google Scholar
-
Teerawattanapong, N. et al. A systematic review of the burden of multidrug-resistant healthcare-associated infections among intensive care unit patients in Southeast Asia: The rise of multidrug-resistant Acinetobacter baumannii. Infect. Control Hosp. Epidemiol. 39, 525–533. https://doi.org/10.1017/ice.2018.58 (2018).
Google Scholar
-
Yang, W. et al. Trends of intra-cranial bacterial infection in patients requiring emergency neurosurgery. Surg. Infect. (Larchmt) 21, 677–683. https://doi.org/10.1089/sur.2019.317 (2020).
Google Scholar
-
Ma, X. et al. First multicenter study on multidrug resistant bacteria carriage in Chinese ICUs. BMC Infect. Dis. 15, 358. https://doi.org/10.1186/s12879-015-1105-7 (2015).
Google Scholar
-
Minhas, P. et al. Risk factors for positive admission surveillance cultures for methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci in a neurocritical care unit. Crit. Care Med. 39, 2322–2329. https://doi.org/10.1097/CCM.0b013e3182227222 (2011).
Google Scholar
-
Wu, D. et al. Evaluating the efficiency of a nomogram based on the data of neurosurgical intensive care unit patients to predict pulmonary infection of multidrug-resistant Acinetobacter baumannii. Front. Cell Infect. Microbiol. 13, 1152512. https://doi.org/10.3389/fcimb.2023.1152512 (2023).
Google Scholar
-
Hu, P. J., Pittet, J. F., Kerby, J. D., Bosarge, P. L. & Wagener, B. M. Acute brain trauma, lung injury, and pneumonia: More than just altered mental status and decreased airway protection. Am. J. Physiol. Lung Cell Mol. Physiol. 313, L1-l15. https://doi.org/10.1152/ajplung.00485.2016 (2017).
Google Scholar
-
Quyet, D. et al. Risk factors for stroke associated pneumonia. Open Access Maced. J. Med. Sci. 7, 4416–4419. https://doi.org/10.3889/oamjms.2019.873 (2019).
Google Scholar
-
Zhou, Y., Yu, F., Yu, Y., Zhang, Y. & Jiang, Y. Clinical significance of MDRO screening and infection risk factor analysis in the ICU. Am. J. Transl. Res. 13, 3717–3723 (2021).
Google Scholar
-
Luyt, C. E. et al. Imipenem, meropenem, or doripenem to treat patients with Pseudomonas aeruginosa ventilator-associated pneumonia. Antimicrob. Agents Chemother. 58, 1372–1380. https://doi.org/10.1128/aac.02109-13 (2014).
Google Scholar
-
Elsorady, K. E., Hassan, R. A., Abdelhamid, D. H. & Abd El-Mohsen, M. Antibiotics use and its association with multi-drug resistance in a tertiary care geriatrics hospital in Egypt. J. Infect. Dev. Ctries. 16, 1860–1869. https://doi.org/10.3855/jidc.17257 (2022).
Google Scholar
-
Mei-Sheng Riley, M. & Olans, R. Implementing an antimicrobial stewardship program in the intensive care unit by engaging critical care nurses. Crit. Care Nurs. Clin. North Am. 33, 369–380. https://doi.org/10.1016/j.cnc.2021.07.001 (2021).
Google Scholar
-
Raman, G., Avendano, E. E., Chan, J., Merchant, S. & Puzniak, L. Risk factors for hospitalized patients with resistant or multidrug-resistant Pseudomonas aeruginosa infections: A systematic review and meta-analysis. Antimicrob. Resist. Infect. Control 7, 79. https://doi.org/10.1186/s13756-018-0370-9 (2018).
Google Scholar
-
Rai, I., Stephen, A. H., Lu, Q. & Heffernan, D. S. Impact of multi-drug-resistant pneumonia on outcomes of critically ill trauma patients. Surg. Infect. (Larchmt) 21, 422–427. https://doi.org/10.1089/sur.2019.240 (2020).
Google Scholar
-
Mader, M. M., Grensemann, J., Kluge, S., Westphal, M. & Czorlich, P. Rate and impact of multidrug-resistant organisms in patients with aneurysmal subarachnoid hemorrhage. Acta. Neurochir .(Wien) 160, 2049–2054. https://doi.org/10.1007/s00701-018-3637-2 (2018).
Google Scholar
-
Magira, E. E., Islam, S. & Niederman, M. S. Multi-drug resistant organism infections in a medical ICU: Association to clinical features and impact upon outcome. Med. Intensiva 42, 225–234. https://doi.org/10.1016/j.medin.2017.07.006 (2018).
Google Scholar
-
Kollef, M. H. et al. The intensive care medicine research agenda on multidrug-resistant bacteria, antibiotics, and stewardship. Intensive Care Med. 43, 1187–1197. https://doi.org/10.1007/s00134-017-4682-7 (2017).
Google Scholar
-
Doganci, M., Izdes, S. & Cirik, M. O. The evaluation of risk factors for vancomycin-resistant enterococcus colonization and infection among mixed adult intensive care unit patients. Cureus 15, e33210. https://doi.org/10.7759/cureus.33210 (2023).
Google Scholar
-
Han, Y., Zhang, J., Zhang, H. Z., Zhang, X. Y. & Wang, Y. M. Multidrug-resistant organisms in intensive care units and logistic analysis of risk factors. World J. Clin. Cases 10, 1795–1805. https://doi.org/10.12998/wjcc.v10.i6.1795 (2022).
Google Scholar
-
Mody, L. et al. A targeted infection prevention intervention in nursing home residents with indwelling devices: A randomized clinical trial. JAMA Intern. Med. 175, 714–723. https://doi.org/10.1001/jamainternmed.2015.132 (2015).
Google Scholar
-
Gupta, T. et al. Prediction of 28-day mortality in acute decompensation of cirrhosis through the presence of multidrug-resistant infections at admission. J. Gastroenterol. Hepatol. 35, 461–466. https://doi.org/10.1111/jgh.14788 (2020).
Google Scholar
-
Osterhoff, G. et al. Role of pre-operative blood transfusion and subcutaneous fat thickness as risk factors for surgical site infection after posterior thoracic spine stabilization. Surg. Infect. (Larchmt) 16, 333–337. https://doi.org/10.1089/sur.2014.081 (2015).
Google Scholar
-
Sreeramoju, P. V., Tolentino, J., Garcia-Houchins, S. & Weber, S. G. Predictive factors for the development of central line-associated bloodstream infection due to gram-negative bacteria in intensive care unit patients after surgery. Infect. Control Hosp. Epidemiol. 29, 51–56. https://doi.org/10.1086/524334 (2008).
Google Scholar
-
Chelazzi, C., Pettini, E., Villa, G. & De Gaudio, A. R. Epidemiology, associated factors and outcomes of ICU-acquired infections caused by gram-negative bacteria in critically ill patients: An observational, retrospective study. BMC Anesthesiol. 15, 125. https://doi.org/10.1186/s12871-015-0106-9 (2015).
Google Scholar
-
Karruli, A. et al. Clinical characteristics and outcome of MDR/XDR bacterial infections in a neuromuscular semi-intensive/sub-intensive care unit. Antibiotics (Basel) https://doi.org/10.3390/antibiotics11101411 (2022).
Google Scholar
-
Katip, W. & Oberdorfer, P. Clinical efficacy and nephrotoxicity of colistin alone versus colistin plus vancomycin in critically ill patients infected with carbapenem-resistant Acinetobacter baumannii: A propensity score-matched analysis. Pharmaceutics https://doi.org/10.3390/pharmaceutics13020162 (2021).
Google Scholar
-
Katip, W., Uitrakul, S. & Oberdorfer, P. A comparison of colistin versus colistin plus meropenem for the treatment of carbapenem-resistant Acinetobacter baumannii in critically ill patients: A propensity score-matched analysis. Antibiotics (Basel) https://doi.org/10.3390/antibiotics9100647 (2020).
Google Scholar
-
Katip, W., Rayanakorn, A., Oberdorfer, P., Taruangsri, P. & Nampuan, T. Short versus long course of colistin treatment for carbapenem-resistant A. baumannii in critically ill patients: A propensity score matching study. J. Infect. Public Health 16, 1249–1255. https://doi.org/10.1016/j.jiph.2023.05.024 (2023).
Google Scholar
Funding
This work was supported by the Research Fund of Guizhou Provincial Health Commission (gzwjkj2019-1-030), Science and Technology Joint Funds of Zunyi Science and Technology Bureau & The First People’s Hospital of Zunyi (2020-118, 2020-119).
Author information
Authors and Affiliations
Contributions
H. J. and N. Q. completed the research design. H. J. and H. P. performed the experiments. H. J. and N. Q. conducted the literature search and data collection. H. J. and N. Q. performed the statistical analysis and interpretation of the data. H. J. and N. Q. were responsible for writing the manuscript. All the authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary Information.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
Reprints and Permissions
About this article
Cite this article
Jiang, H., Pu, H. & Huang, N. Risk predict model using multi-drug resistant organism infection from Neuro-ICU patients: a retrospective cohort study.
Sci Rep 13, 15282 (2023). https://doi.org/10.1038/s41598-023-42522-2
-
Received: 20 June 2023
-
Accepted: 11 September 2023
-
Published: 15 September 2023
-
DOI: https://doi.org/10.1038/s41598-023-42522-2
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.