Infection
Can CRISPR Crack the Code to Treating HIV Infections?
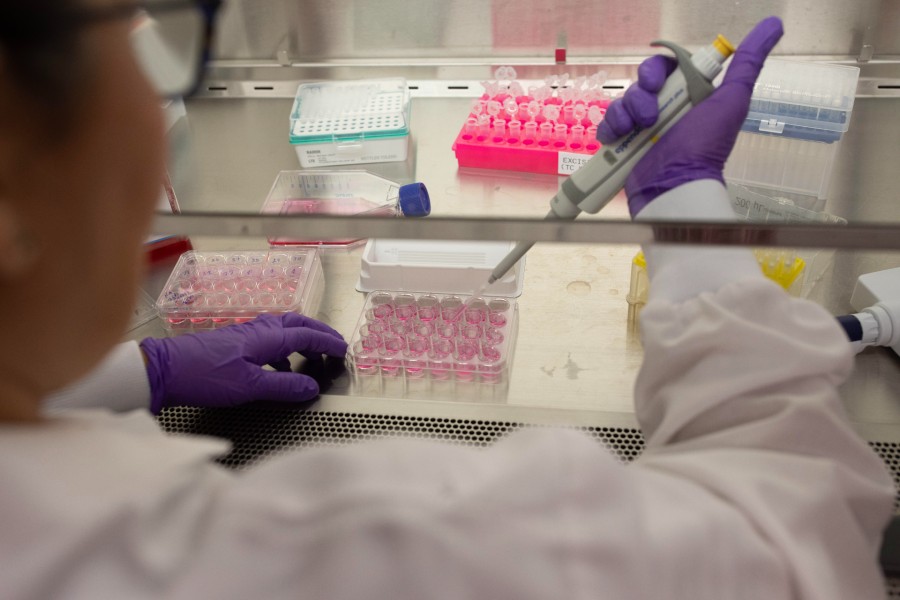
Scientists at Excision BioTherapeutics are running a human clinical trial for a new CRISPR-based drug called EBT-101 which targets human immunodeficiency virus (HIV) infections. There are many tests that a treatment has to pass before it can truly be called a cure and it’s much too soon to tell if EBT-101 will be successful in that regard. But results from preclinical studies of a close analogue of EBT-101 that was tested in monkeys are extremely promising, offering hope that CRISPR-Cas9 may be the key to eliminating HIV infections.
EBT-101 is the fruit of a collaboration between scientists from the Lewis Katz School of Medicine at Temple University and Excision BioTherapeutics, a clinical-stage biotechnology company that develops CRISPR-based therapies for viral diseases. Excision, which spun out of Temple, is currently running a Phase I/II trial to evaluate the safety and tolerability of EBT-101 in HIV-positive patients.
The decision to move EBT-101 into a clinical trial was bolstered by the success of an analogue of the drug—EBT-001—in rhesus macaques infected with simian immunodeficiency virus (SIV). Details of that study, which provided evidence of the safety and biodistribution in macaques as well as the results were published last month in a paper in Gene Therapy.
Antiretroviral drugs have helped millions infected with HIV but they are toxic to the body and can induce several comorbidities. Patients often struggle with cardiovascular disease and brain dysfunction among other health issues, and the drugs have to be taken daily to keep viral replication at bay. “The pace that studies are progressing from preclinical to clinical trials is really exciting. It is an exciting time but how long it will take for a clinical trial to progress to commercialization? It’s hard to put a definitive number,” Excision’s CSO TJ Cradick, PhD, said in a conversation with GEN.
Finding a cure for HIV has long been the goal of researchers, clinicians, patients, and caregivers. For Kamel Khalili, PhD, a virologist and senior investigator on the EBT-001 study, the discovery of CRISPR was a much-needed breakthrough in the search for a potential cure. Khalili is the chair of the department of microbiology, immunology, and inflammation, director of the Center for Neurovirology and Gene Editing, and director of the Comprehensive NeuroAIDS Center at Temple’s School of Medicine. He has spent much of his career studying HIV’s mechanisms and thinking of strategies for curing the disease that work either by eliminating copies of integrated viral DNA in the host genome or by finding cells that harbor viral genomes and removing them from the body.
Before CRISPR, Khalili and his team considered various gene editing approaches for excising viral DNA from host genomes including zinc-finger nucleases, but it wasn’t until CRISPR, and its precise way of genome editing, came along that he finally found a system that had the potential to work HIV.
Cradick expressed similar sentiments. He has worked with gene editing technologies like zinc-finger nucleases (ZFNs), transcription activator-like effector nucleases, as well as CRISPR in both academia and industry throughout his career including at institutions like Georgia Tech and companies like CRISPR Therapeutics prior to joining Excision.
For example, he has designed ZFNs to target and cut the genome of hepatitis B virus to treat infections. Their approach involved designing two nucleases that cut the target viral sequence which was then repaired with edits like insertions and deletions that inactivated the virus. But there was a chance for viral escape. The error-prone polymerases would sometimes make bad copies and correct the mutation, he explained. CRISPR’s multiplexed approach to editing using multiple guides gets around these challenges. “When we go in with multiple guides as described in [the CRISPR study] … we have three different chances to cut the viral sequence and three different inactivating excisions. We have a much greater chance of inactivating the virus.”
Building up to human testing
In addition to the Gene Therapy paper, scientists from Excision and Temple have published other papers documenting their research into a CRISPR-based HIV drug. Some of their earliest tests of the EBT-001 treatment were published in Nature Communications in 2020. That study, which also involved macaques was a source of some of the early evidence that a CRISPR-based treatment could work safely and effectively. That was a much smaller-scale study involving only three animals. And the researchers assessed the effectiveness of the drug three weeks post-treatment.
But before they could be approved by the FDA to begin testing EBT-101 in humans, they needed more evidence of the treatment’s safety. This meant providing evidence of the effects of different drug dosing levels at several time points in nonhuman primates.
EBT-001 is identical to the human version of the gene therapy except that it uses gRNAs that are specific to SIV sequences. For the preclinical trial, the Temple researchers packaged an SIV-specific CRISPR gene-editing construct that included the Cas9 endonuclease and the guide RNAs into an adeno-associated virus 9 (AAV9) carrier that could be injected intravenously into SIV-infected animals. Other studies have validated the use of AAV9 as a delivery vehicle for gene therapies in both animal models and clinical trials. The gRNAs in the construct target viral long terminal repeats (LTR) and the Gag gene. Once there, the treatment makes one of three possible deletions: 5′LTR to Gag, Gag to 3′LTR, and 5′LTR to 3′LTR. The team also manipulated the construct in such a way that once the viral genome is excised, the fragment can’t simply reintegrate back into the genome.
“We [tried] to target regions of the virus that don’t mutate as much,” Tricia Burdo, PhD, an expert in nonhuman primate HIV-1 models and one of the authors of the paper, explained to GEN. Burdo is a professor and vice chair in the department of microbiology, immunology, and inflammation and the Center for Neurovirology and Gene Editing at Temple’s medical school. She began working on SIV during her post-doctoral studies at Scripps Research Institute and took the lead on the team’s current studies in macaques.
LTR and Gag are highly conserved meaning that even though SIV, much like HIV, mutates, the target regions should remain largely the same. However, the treatment will still work even if the conserved regions change. For example, if LTR mutates, the construct will still cut the Gag gene and that is enough to prevent the virus from replicating. Furthermore, “because we are using two gRNAs, and the gRNA for LTR can cut in two spots, any of those cuts will render the virus incapable of replication,” Burdo explained. “It’s kind of a fail-safe.”
According to the Gene Therapy paper, the team selected 12 monkeys for two studies. For one study, Burdo and her team randomized 10 monkeys into a control group and two treatment groups. The animals in the treatment group received an injection containing one of three doses of EBT-001. The researchers also tested even higher doses of the drug in two additional monkeys as part of a second study and tested those participants at six months.
In the study involving 10 monkeys, three months after their treatment, the researchers analyzed blood and tissue from known viral reservoirs in the body such as the lymph nodes and the spleen to assess the effect of EBT-001. They also collected data on the biodistribution of the different doses that they tested in the study. They repeated the analysis six months post-treatment.
The results showed that EBT-001 was broadly distributed throughout the monkeys’ tissue samples, and there was evidence of edited SIV proviral DNA in the monkeys’ cells and tissues. Importantly, there was no evidence indicating that the drug was toxic at any of the doses tested in the monkeys and there were no off-target effects observed. Some monkeys even put on a little weight. Burdo and Khalili plan to continue working on applying CRISPR to treat SIV. For example, they plan to study what happens when they withdraw ARTs and just treat the monkeys with CRISPR. The goal would be to assess whether the virus rebounds post-treatment in the absence of the drugs.
The successful trial of EBT-001 in macaques was the final bit of evidence that Excision needed to secure federal approval to test EBT-101 in human patients. The company is currently enrolling patients in the Phase I/II study which officially launched in 2022, and will test three doses of EBT 101. Each participant will have to have been on ARTs prior to starting EBT-101, and will receive a single dose of the drug. Each person will be followed over a four-year period. Excision plans to enroll nine patients in total.
One open question that the clinical trial will hopefully answer is whether the CRISPR strategy can successfully eliminate all the single copies of the virus from the host genome without requiring additional drugs. “We have a hypothesis that if we eliminate the majority of the integrated virus, that may increase the immune system and that can wipe out the remaining infected cells,” Khalili said. “That’s what the clinical trial will tell us.”
If it is as successful as it was in nonprimates, a single shot of EBT-101 could be enough to provide relief for millions of people living with HIV. Furthermore, since the participants will not be on antiretrovirals during the trial, clinicians can assess whether the virus rebounds after treatment, and if so, exactly when that happens. Information like this would be useful for refining the treatment so that it works even better than before. “We are approaching 40 years of the HIV AIDS pandemic. A cure is long overdue,” Khalili said. “We are on our way, but we are not there yet. We are not going to stop until we get there.”