Infection
Device strategies to prevent healthcare-associated infections

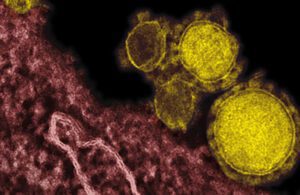
[Image courtesy of the National Institute of Allergy and Infectious Diseases]
Device design, sterilization before use and proper cleaning of reusable equipment can prevent infections and save lives.
By Ted Eveleth, AvantGuard
Nosocomial infections, also commonly known as healthcare-associated infections (HAIs), are a multibillion-dollar problem and a leading cause of morbidity and mortality around the world. On any given day, about 1 in 31 hospital patients has at least one HAI, according to the Centers for Disease Control and Prevention.
A significant cause for many of these HAIs are medical devices that touch or are implanted in the body, such as surgical implants, catheters and endoscopy devices.
For example, 75% of urinary tract infections in healthcare settings are associated with urinary catheters. Central line-associated bloodstream infection (CLABSI), another category of HAIs associated with medical devices, results in thousands of deaths and billions of dollars of added costs to the healthcare system. Surgical site infections and infections from cross contaminated surgical devices and noninvasive devices are additional sources of nosocomial infections, as are infections caused by permanent medical devices such as knee implants.
Several measures can help minimize the risk of HAIs caused by medical devices. Many medical devices, such as urinary and central-line catheters, are manufactured, packaged and sterilized as single-use devices. This ensures the device is pathogen-free during shipment and storage, until the device is opened. However, the device itself offers no protection against pathogens once opened and used on a patient.
For reusable devices, proper reprocessing (which includes cleaning and disinfection) is critical for protecting the patient. Reusable flexible endoscopes have long been associated with patient infections. Because they can cost upwards $90,000 and due to their complexity (multi-channel, intricate with exacting dimensions that require labor-intensive assembly), replacing a scope for each procedure is likely to significantly change the economics of some procedures.
Endoscopes are challenging to reprocess because their thin, narrow tubes are hard to access, mechanically scrub and get dry after reprocessing, and their plastic parts need to avoid degradation due to chemical attack to maintain life expectancy.
The FDA plays a critical role in helping healthcare settings reduce the risk of infection from reusable devices, focusing on three areas; device design, the science of reprocessing, and improving collaboration between key stakeholders, including health care providers, device manufacturers, accrediting organizations and government agencies. The CDC offers guidance for the disinfection of healthcare equipment including medical devices, though it is the FDA that regulates and approves chemical formulations for achieving medical device disinfection.
In standard manual cleaning practices, the use of disinfectants is prone to potential errors: lack of adherence to directions for use, incorrect dilutions, or solutions not left on surfaces for enough time. A serious shortcoming of disinfectants is that they provide one-time, short-term disinfection of the surface not continuous residual antimicrobial protection. The drawbacks of existing cleaning practices, disinfectants and other technologies leave room for improvement and a need for new and innovative technologies for protecting surfaces and medical devices.
Antimicrobial medical devices can play a crucial role in reducing the risk HAIs and improving patient outcomes. Antimicrobial devices are designed to limit the spread of infectious diseases by incorporating materials or coatings that inhibit the growth and spread of microorganisms such as bacteria, viruses or fungi. This lowers the risk of surface contamination and subsequent spread to healthcare workers or patients. Antimicrobial devices can impede or disrupt biofilm formation, which is crucial as biofilms can serve as reservoirs for infectious agents and make cleaning and disinfection more challenging.
Antimicrobial medical devices work in a variety of ways. Many medical devices are designed to slowly release antimicrobial chemicals such as silver ions from the device surface. These chemicals can interact with microorganisms, damaging their cell membranes or interfering with their metabolic processes, effectively killing them or preventing their growth.
Modifying the surface of the medical device with a coating or surface chemistry can also make the surface less suitable for microbial attachment and growth. By limiting the ability of microorganisms to adhere to the device, antimicrobial coatings reduce the chances of device-associated infections. This is particularly important for medical devices that are implanted in the body or catheters, implants, or prosthetics that come into contact with bodily fluids.
Some antimicrobial devices employ electrochemical processes to kill microorganisms. These methods include using a small electric current or generating specific electrochemical agents that are lethal to microbes.
Antimicrobial medical devices should be viewed as one component of a comprehensive infection control strategy. Although antimicrobial medical devices can play a crucial role in reducing the risk of healthcare-associated infections and improving patient safety, it is important to note that no medical device can eliminate all microorganisms, and proper cleaning and sterilization procedures still need to be followed.
Technologies in development
New technologies being developed for general surface disinfection can potentially be repurposed to better protect medical devices from becoming a source of nosocomial infections through chemistries that are continuously active and can provide efficacy between regular cleaning and disinfection. These types of products are intended to reduce the level of recontamination of high-touch surfaces.
The Environmental Protection Agency (EPA) divides products with residual efficacy claims into two categories: (1) disinfectants that also have residual efficacy, and (2) supplemental residual antimicrobial products that do not meet the EPA’s standard for disinfection claims but can be used as a supplement to standard disinfection practices to protect surfaces between disinfections. To date there are few products that can meet the EPA’s standard for these categories, but standards now exist and are a target for new product development.
The good news is that new chemistries that can provide supplemental antimicrobial protection for days and weeks are coming. These technologies should help protect patients treated with medical devices by killing pathogens and preventing biofilm formation on medical device surfaces between regular cleaning and disinfection.
And unlike current antimicrobials that cannot pass the EPA’s standard for supplemental residual efficacy, these new chemistries will meet EPA’s standard and will protect not just surfaces, but patients from device-associated infections.


AvantGuard CEO Ted Eveleth [Photo courtesy of AvantGuard]
Ted Eveleth is CEO at AvantGuard, which is creating innovative solutions that manage surfaces and provide long-term protection against viruses, bacteria, and fungi/mold in a variety of applications. The company’s proprietary combinations of specialty molecules and polymers are customized to provide prolonged, residual, antimicrobial efficacy to a wide range of surfaces and materials.
How to submit a contribution to MDO
The opinions expressed in this blog post are the author’s only and do not necessarily reflect those of Medical Design & Outsourcing or its employees.