Blood
These Startups Want You to Send Them Your Period Blood
The kit arrives in your mailbox in a cardboard box stamped with a modern, serif-font logo. It’s the kind of sleek, clean design so often associated with direct-to-consumer brands that fill your social media feeds with ads. A hip makeup line could easily be inside, or a set of razors with a cutesy name.
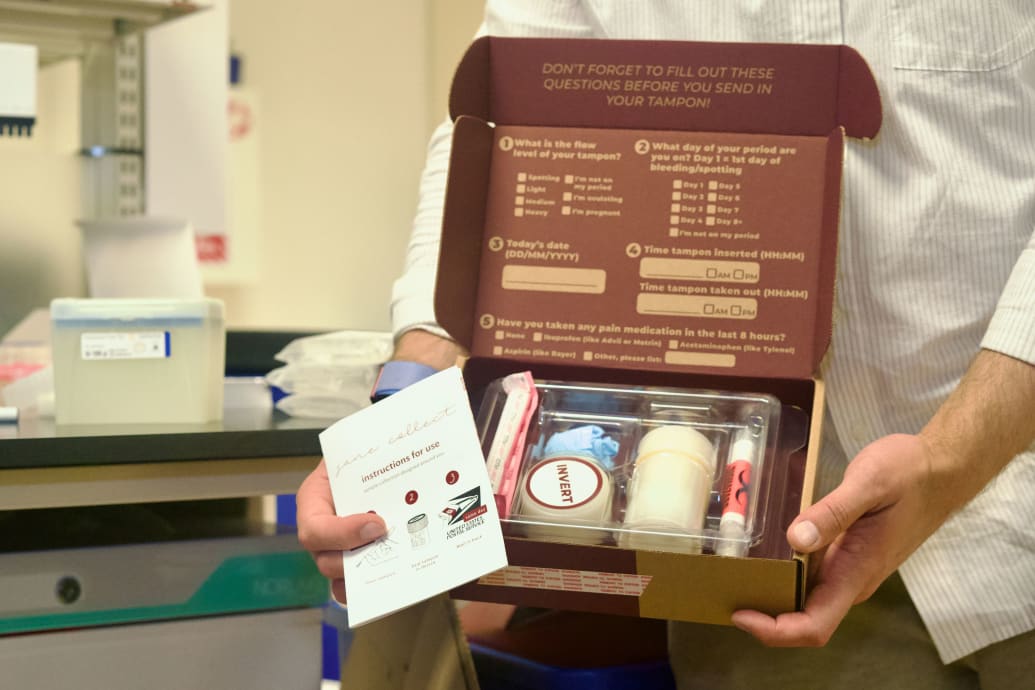
Instead, you open the box and find a pair of gloves, a specimen collection jar, and an organic cotton tampon.
NextGen Jane, a health tech startup founded in 2014, sends these kits to menstruators who volunteer to participate in one of the company’s clinical studies. Users wear the tampon for a specified amount of time before removing it and depositing it into the collection jar. Once the jar is sealed, a solution in the container activates to keep the sample’s DNA and RNA intact in ambient temperatures for up to two weeks. Users pack the jar in a supplied, self-addressed box, and drop it in the mail to be sent to NextGen Jane’s lab in Oakland, California for analysis.
The thought that menstrual blood is worthy of being sent anywhere other than the trash is revolutionary. For as long as people have been menstruating, menstrual blood has been seen as medical waste, Anna Villarreal, CEO and founder of LifeStory Health, told The Daily Beast. “Everybody was taught that there was no clinical utility to menstrual blood.”
NextGen Jane
LifeStory Health is a bioscience company researching how biomarkers—anything within the body that can be measured, such as a person’s pulse, blood pressure, or nutrient levels—in menstrual blood may be used as a medical screening tool. The startup, along with companies like NextGenJane, is helping turn the proverbial tide on menstrual effluent (the fluid comprising blood, vaginal secretions, and cells from the uterine lining that is shed during a person’s menstrual cycle) and see an opportunity to improve health-care for people with uteruses.
“If menstrual blood has value, then it’s just not a waste product anymore,” Paul Blumenthal, director of the Stanford Program for International Reproductive Education and Services, told The Daily Beast. “And if it’s not a waste product anymore, then maybe we can do something about menstrual stigma.”
It’s this very same stigma that has contributed to a longstanding knowledge gap when it comes to understanding women’s health. “Women’s health research has been overlooked [and] underfunded,” Sara Naseri, CEO and co-founder of Qvin, another startup focused on medical uses for menstrual blood, told The Daily Beast in an email. “It was not until 1993 when women and minorities were, by law, included in clinical trials. However, there continues to be an ongoing lack of female representation and participation in medical research.”
Christine Metz, co-director of the Research OutSmarts Endometriosis (ROSE) clinical study at Northwell Health, wrote a 2022 op-ed in Scientific American that argued that menstrual blood is “one of the best sources of biological material for studying women’s reproductive help.” Despite this, it’s rarely studied due to what Metz calls an “ick factor.”
Far from grossed out, Metz is excited about the possibilities presented by using period blood in medical testing. For the past 10 years, she has used menstrual effluent in her research to develop noninvasive methods for diagnosing and treating endometriosis, a painful condition in which cells that are similar to the cells that line the uterus grow elsewhere in the body. Prior to the start of the ROSE study in 2013, the only way to diagnose endometriosis was by removing bits of this tissue via surgery for a biopsy, Metz said.
This didn’t make a ton of sense to her and her research partners, however, because lesions only formed once the disease had progressed. They wondered if there was a way to detect endometriosis earlier than the seven to 10 years it has historically taken doctors to diagnose the conditions.
“There was a lot in the literature at that time that the lining of the uterus, what we call the endometrium, is different in patients with and without endometriosis,” Metz told The Daily Beast. “So we theorized that we could study menstrual blood, [which contains] the shed endometrium, to look for those differences…No one had previously used menstrual blood in any way to study the endometrium.”
NextGen Jane
But developing a method to collect, transport, process, and analyze these samples safely and sanitarily proved to be an early challenge. Eventually, the ROSE team came up with the direct-to-consumer model: each of the study’s more than 5,000 participants receive a collection kit in the mail that includes either a menstrual cup donated by Diva International or a collection sponge (depending on user preference) as well as cold pack and gel pack to keep the sample at a stable temperature during its return journey. Just like with NextGen Jane, participants package their samples from the comfort of their own homes and ship them to the research facility.
While Northwell Health’s ROSE study focuses specifically on endometriosis, others in this space are exploring a host of areas where menstrual effluent could be a meaningful diagnostic tool that is less invasive and easier to access than existing options. NextGen Jane was the first to look at menstrual effluent on the molecular level in order to gain insights into what the company calls your “menstrualome,” or the collective set of data gathered about one’s menstrual cycle.
Knowledge of what’s happening at a molecular level in a person’s body is vital for understanding how diseases progress, Ridhi Tariyal, CEO and co-founder of NextGen Jane, told The Daily Beast. “You can’t actually arrive at that understanding unless you are doing molecular characterization of tissues of interest to female reproductive biology.”
Current clinical studies being undertaken by NextGen Jane include a baseline study to better understand what a “typical” menstrual cycle looks like in healthy people as well as studies looking at the diagnosis of uterine diseases and pregnancy health issues.
Meanwhile, the researchers at LifeStory Health analyze the levels of two proteins that are only found in menstrual blood. “Right now, we’ve explored infertility… We can [use menstrual blood to] definitively determine a female’s propensity for a normal pregnancy,” Villarreal explained. “We’re still trying to figure out which reproductive pathologies we can look at and detect.”
With Qvin, Naseri began her research on the uses for menstrual blood by asking a basic—but surprisingly unanswered—question: Is menstrual blood the same as the systemic blood that runs through your veins? If the answer is yes—meaning, biomarkers in the two types of samples are known to be consistent—then menstrual blood could be used for medical screening in place of blood samples that need to be drawn from a vein (with a needle) at the doctor’s office.
In 2019, Naseri and Blumenthal co-authored a study published in the Journal of Clinical and Laboratory Medicine. In it, the authors compared the levels of nine different biomarkers (including cholesterol, triglycerides, and certain hormones) in both menstrual blood and systemic blood. For seven of the nine, levels were consistent in samples from both types of blood
Naseri said that she and her team have proven that menstrual blood can be used to access biomarkers associated with thyroid health, average blood sugar levels for diabetes and pre-diabetes management, inflammation, and ovarian reserve and other fertility and perimenopause hormones.
Qvin has also received FDA approval in Thailand for its Q-Pad—basically, a menstrual pad with a removable collection strip that users mail in for analysis—to be used to test for high-risk human papillomavirus (HR-HPV), a potential precursor to cervical cancer. The Q-Pad is awaiting FDA approval in the U.S..
Across the pond, European companies are taking advantage of menstrual-blood testing’s at-home collection methods and going direct-to-consumer with their products. Theblood, a German fem-tech company founded in 2022, sells a “Cycle Check” kit for €30. Users can send in a sample of their menstrual blood (using their own menstrual cup) and receive a 15-page report with “understandable, scientific advice on your cycle.” report with information regarding their cycle—such as an analysis of the sample’s color and consistency—that the company claims can be used to “optimize your cycle for maximum well-being,” including to “manage pain and discomfort more effectively to improve your daily life.” (Theblood’s website offers little specifics about the information it sends its users, but does include a disclaimer that says the report is not medical advice and does not contain biomarker analysis.)
MyPeriodTest, another Berlin-based initiative, is currently part of the research institution Fraunhofer-Gesellschaft’s AHEAD Accelerator program. Founder Sabine Richter hopes to test menstrual blood for specific biomarkers and then deliver the results to the consumer through an app. “The data belongs to the customer, she decides whether and with which doctor she wants to share the results,” Richter told The Daily Beast in an email.
NextGen Jane
At-home health tests of different types, such as tests for food sensitivities or gut health, are already a big business. The market is estimated to be worth more than $45 million globally by 2031. But many professionals in the menstrual-blood testing space are hesitant to pursue a testing model for menstrual blood that cuts the health-care practitioner out of the equation.
Empowering patients—particularly people in populations that are traditionally overlooked and underserved, such as women—with information about their bodies could help them better advocate for themselves and achieve better health outcomes. But giving people health data without the appropriate amount of guidance could cause unnecessary stress and confusion.
“I don’t want somebody to be detecting ovarian cancer early and then not being under the care of a physician,” Villarreal said.
Instead, many professionals envision a tomorrow where menstrual-blood tests become a staple in people’s preventative care routines. Patients could send their OB/GYN a sample prior to their annual checkup to have labs run before they arrive. Then, valuable face-time with their doctor could be spent discussing solutions rather than exploring issues, Blumenthal said.
To make this a reality, menstrual-blood research needs to continue—and the experts are excited about how wide-reaching new applications for menstrual-blood could be.
For instance, Metz has partnered with scientists at Harvard to explore menstrual blood as a means for assessing people’s exposure to “forever chemicals” (PFAs). The folks at Qvin, meanwhile, haves identified a slate of additional biomarkers to test against venous blood. And the LifeStory Health team has their sights set on using their technology for early detection of female-specific cancers; they’re currently enrolling for a clinical study on the use of biomarkers in menstrual blood for detecting breast, endometrial, and lung cancer.
“Menstrual blood could be the broad platform to every single reproductive pathology that you can think of,” Villarreal said. The period, it’s clear, is just the beginning of this story.