Infection
Babies, toddlers living in urban areas experience more respiratory infections
September 25, 2023
2 min read
Source/Disclosures
Brustad N, et al. Abstract PA2721. Presented at: European Respiratory Society International Congress; Sept. 9-13, 2023; Milan.
Disclosures:
Brustad reports no relevant financial disclosures.
Key takeaways:
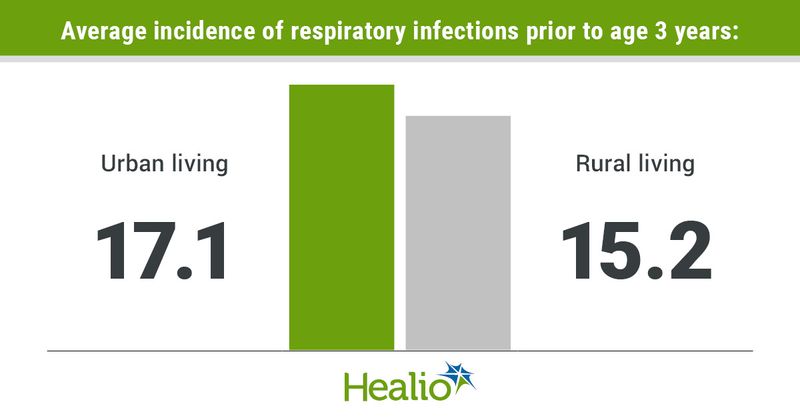
- Incidence of respiratory infections during early childhood was higher in urban vs. rural areas.
- Differences in airway immune and metabolomic profiles may explain this relationship.
Respiratory infections occurred more frequently among babies and toddlers living in urban vs. rural areas, according to a presentation at the European Respiratory Society International Congress.
“Our findings suggest that urban living is an independent risk factor for developing infections in early life when taking account of several related factors such as exposure to air pollution and starting day care,” Nicklas Brustad, MD, PhD, postdoctoral researcher and physician on the Copenhagen Prospective Studies on Asthma in Childhood (COPSAC), said in a press release from the European Respiratory Society. “Interestingly, changes in the blood of pregnant mothers and newborn babies, as well as changes in the newborn immune system, seem to partly explain this relationship.”
Using the COPSAC2010 cohort that includes data on mother-child pairs from pregnancy until age 3 years, Brustad and colleagues assessed 663 children to determine if there is a difference in risk for infections during childhood based on rural vs. urban residence.
Researchers used the CORINE land cover database to classify areas as rural or urban, and they relied on parental reporting of infection symptoms to track infection prevalence in each living environment.
Overall, children had a mean 16.3 infection episodes, which researchers noted were primarily respiratory in nature.
Following adjustment for several variables, researchers observed more early childhood respiratory infections in urban vs. rural areas (mean, 17.1 vs. 15.2; adjusted incidence rate ratio [IRR] = 1.15; 95% CI, 1.05-1.26). This increase in infections at age 3 years was, in turn, associated with an increase in asthma at age 6 years (OR = 1.15; 95% CI, 1.11-1.19).
Different airway immune profiles at age 4 weeks associated with urban living — which researchers described as principal component 1 (IRR = 1.03; 95% CI, 1-1.06) and principal component 2 (IRR = 1.04; 95% CI, 1.01-1.07) — appeared to mediate the greater risk for infections among these children.
Notably, in the 24th week of pregnancy and 2 to 3 days following birth, researchers conducted maternal and child metabolomics profiling using blood tests.
Similar to airway immune profiles, mothers and children residing in urban areas had altered metabolomic profiles vs. those living in rural areas, and this contributed to a heightened risk for infections, according to researchers, who describe the risk as “borderline mediated through” differences in a mother’s metabolomic profile.
“We continue to investigate why some otherwise healthy children are more prone to infections than others and what the implications are for later health,” Brustad said in the release. “We have several other studies planned that will look for risk factors and try to explain the underlying mechanisms using our large amount of data.”