Cardiovascular
New study reveals alarming cardiovascular risks
In a recent study published in the journal Nature Cardiovascular Research, a group of researchers determined whether Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) directly infects coronary vessels and atherosclerotic plaques to understand its role in inducing plaque inflammation. They assessed its contribution to acute cardiovascular complications and increased long-term cardiovascular risk in patients with coronavirus disease 2019 (COVID-19).
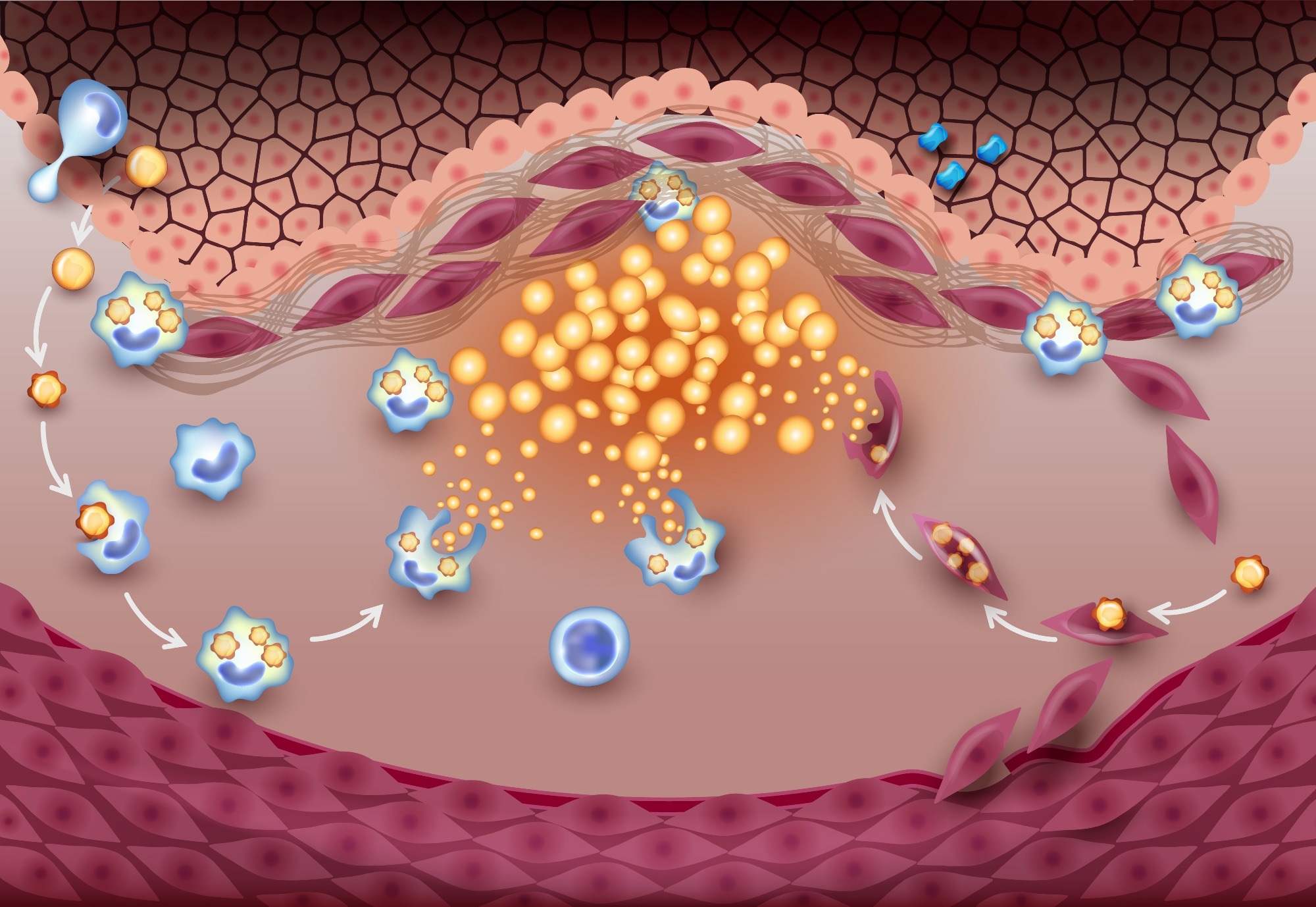
Study: SARS-CoV-2 infection triggers pro-atherogenic inflammatory responses in human coronary vessels. Image Credit: TimeLineArtist / Shutterstock
Silent Cardiovascular Threat of COVID-19
COVID-19, caused by SARS-CoV-2, exhibits varied symptoms, ranging from none to severe respiratory distress and multi-organ failure, sometimes leading to death. A significant concern is the heightened risk of cardiovascular events like heart attack and stroke, persisting up to a year post-infection, markedly more than in cases of influenza. These events are typically linked to the inflammation of arterial plaque. Analysis of autopsy specimens revealed that the virus infects infiltrating macrophages within coronary vessels, particularly lipid-laden ones, inducing substantial pro-atherogenic inflammatory responses. This suggests a direct link between the virus and observed cardiovascular complications in COVID-19 patients. Further research is crucial to comprehend these interactions thoroughly, fostering the development of targeted interventions to diminish long-term cardiovascular risks in survivors.
Unraveling COVID’s Heart Connection
The present study strictly conformed to ethical standards, examining autopsy specimens from eight COVID-19 patients to investigate the presence of SARS-CoV-2 ribonucleic acid (RNA) in coronary macrophages, utilizing advanced methodologies such as RNAscope in situ hybridization and spatial artificial intelligence (AI). The findings disclosed the presence and replication of viral RNA in each section analyzed, highlighting an increased susceptibility of coronary macrophages to the virus, notably in Pathological Intimal Thickening (PIT). This implies an elevated risk of cardiovascular complications in those infected.
In the study, scientists quantified infectious particles using plaque assays and explored the impact of silencing Neuropilin-1(NRP1) in human macrophages and foam cells, utilizing advanced molecular biology techniques. Sophisticated protein quantification, Western blot analysis, and Reverse Transcription Quantitative Polymerase Chain Reaction (RT–qPCR) were employed to elucidate the intricate interplay of cellular and viral components. Rigorous RNA-seq data processing, analysis, and visualization were undertaken to understand the nuances of gene expression, and cytokine secretion was assessed to study immune responses. Transmission electron microscopy was utilized to examine infected atherosclerotic samples in detail.
The study implemented rigorous statistical analyses, with significant results highlighting the multi-faceted interactions between SARS-CoV-2 and cellular structures, pointing to critical insights into the pathogenesis of the virus and potential therapeutic targets. The comprehensive approach in methodology and analysis underscores the thoroughness and significance of the research in understanding the implications of SARS-CoV-2 infection in human cells.
Why COVID-19 is a Game-Changer for Heart Health
The study uncovered pivotal data about the susceptibilities of vascular smooth muscle cells (VSMCs) and macrophages to SARS-CoV-2, showing a higher vulnerability in macrophages. The research disclosed that both macrophages and foam cells, which are associated with atherosclerosis, could host the virus. Notably, foam cells demonstrated more susceptibility and a slower virus clearance process. Infected macrophages had heightened interferon responses, enabling quicker viral clearance, while foam cells revealed modified lipid metabolism routes, potentially aiding viral entry and replication.
A deeper study of the Type I Interferon (IFN-I) response underscored kinetic disparities in IFN response and SARS-CoV-2 gene expression between macrophages and foam cells. The results imply that enduring IFN response in macrophages may lead to diminished viral persistence, while the decline in IFN-I score in foam cells affects the infection and replication processes of SARS-CoV-2, showcasing the varying responses and impacts on different cell types.
Investigation into the inflammatory profiles of infected macrophages and foam cells revealed secretion of pro-inflammatory and pro-atherogenic cytokines such as Interleukin 6 ( IL-6) and IL-1β, intensifying ischemic cardiovascular risks. A unique release of IL-18 and IFN-α2 by infected macrophages and foam cells, respectively, were identified, indicating differential inflammatory reactions to viral infection.
Additionally, the study illustrated how SARS-CoV-2 can intensify inflammation within atherosclerotic lesions by infecting human atherosclerotic vascular explants, highlighting the possible increase in ischemic cardiovascular events in individuals with pre-existing atherosclerosis. An examination of various arteries disclosed high expression of SARS-CoV-2 entry receptors and factors in myeloid subclusters, with NRP1 being predominant in Triggering Receptor Expressed on Myeloid cells 2 (TREM2+) macrophages, suggesting its crucial role in mediating infection within the atherosclerotic vasculature. Elevated numbers of NRP1+ macrophages expressing the antisense strand of the S gene in PIT lesions were detected, confirming the increased susceptibility of these lesions to infection.
Pathways to Therapeutic Breakthroughs
The thorough exploration, utilizing silencing RNA to inhibit NRP-1 expression, provided profound insights into its significant impact on SARS-CoV-2 infection and unveiled the nuanced inflammatory and viral response dynamics within various cell types and vascular tissues. These revelations are paramount in understanding the interactions between SARS-CoV-2 and the host and open new possibilities for therapeutic interventions targeting vascular inflammation and atherosclerosis in the context of COVID-19, reinforcing the importance of understanding the direct impact of the virus on cardiovascular tissues, particularly in individuals with existing cardiovascular conditions. This research is foundational for developing strategies to mitigate cardiovascular complications in COVID-19 patients.