Infection
The Impact on Non-Alcohol Fatty Liver Disease With Previous Hepatitis Infections
What You Should Know
Infectious diseases, including hepatitis infections, can have a significant impact on chronic health conditions like non-alcoholic fatty liver disease (NAFLD).
Assessing the interplay between previous infections and NAFLD can be challenging due to potential interactions between treatments for NAFLD and antiviral therapies.
The intricate pathways and mechanisms through which viral infections exacerbate NAFLD’s metabolic disruptions and inflammatory processes highlight the critical role of understanding this interplay.
Too often we neglect to discuss the larger impact of infectious diseases on chronic health conditions. Such relationships aren’t new though – simply under-appreciated and poorly recognized. COVID-19 has shed light on this a bit more, but what about other infectious diseases? Specifically, the effects of hepatitis infections.
The 2021 viral hepatitis surveillance report from the CDC notes a few important findings during 2021, including
- 5728 hepatitis A cases reported leading to 11,500 estimated infections, across 47 states
- 2045 acute cases of hepatitis B and thus 13,300 infections and 14,229 newly reported chronic hepatitis b cases
- 5023 acute cases of hepatitis C across 42 states; there were a total of translating to 69,800 estimated infections and a total of 107,540 newly reported chronic hepatitis C cases.
- For hepatitis E, which is not commonly acquired in the United States, there were sporadic cases reported, caused by HEV genotype 3, which impacted older men over the age of 40 years.
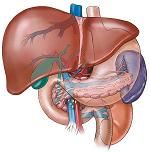
With this in mind, a research team recently sought to address the dynamics between previous HBV, HAV, and HEV infections, and non-alcoholic fatty liver disease. Non-alcoholic fatty liver disease (NAFLD), caused by a build-up of fat in the liver, is often a result of obesity, and impacts 10-20% of Americans. While lifestyle changes can often control or reverse the fat buildup, the most common complication if left unattended is cirrhosis.
The authors broke down each infection and the impact on liver through a review study, underscoring the intricate relationships and convergence of many factors. “Viral infections, acting in synergy with the metabolic disruptions intrinsic to NAFLD, can accelerate the transition from benign hepatic steatosis to more severe conditions such as non-alcoholic steatohepatitis (NASH) and fibrosis. The intricate interplay between viral factors and the underlying metabolic perturbations can amplify the inflammatory cascade, hastening the progression toward fibrogenesis and more advanced liver pathologies.”
Determining the interplay of previous infection and NAFLD though is hard from a diagnostic perspective as treatments for NAFLD can often interact with antiviral therapies, which can impact efficacy. Such viral infections can complicate assessing the severity of NAFLD, making determinations of liver damage exceedingly difficult to truly know.
As such, the authors noted that treatment decisions thus become difficult as the dynamics between antiviral therapy and NAFLD management is nuanced and unique for each patient. Viral loads can vary depending on the viral infection, with higher levels leading to worsening NAFLD metabolic disturbances and medical management must also consider immune responses that can lead to cascading situations such as inflammation around the liver. In short—the relationship is complicated on the best of days.
“The interconnected pathways and mechanisms through which viral infections can exacerbate NAFLD’s metabolic disruptions and inflammatory processes. As we navigate the intersection of these two domains, it becomes abundantly clear that this interplay extends beyond mere academic curiosity, emerging as a pivotal determinant of disease progression, diagnostic complexities, and therapeutic strategies for individuals grappling with viral infections and NAFLD,” the authors wrote.