Blood
New blood test could improve diagnosis & management of concussion
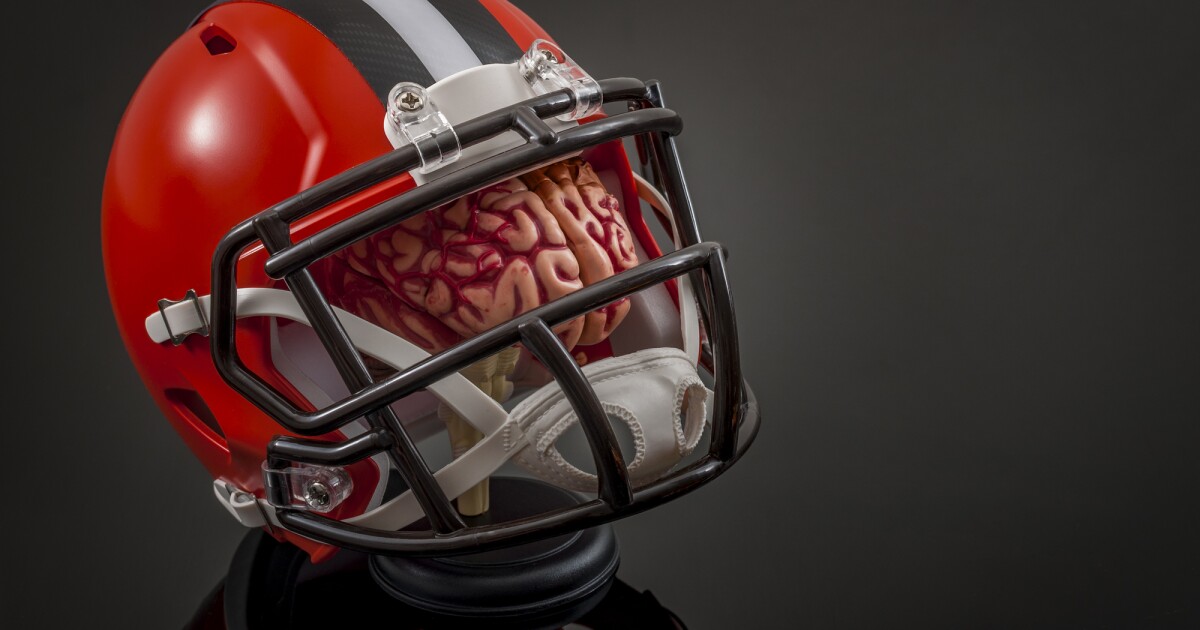
Researchers have found a way to determine whether someone has suffered a concussion by measuring the blood levels of three biomarkers within six hours of the injury. The blood test could be used alongside existing tests for a more accurate diagnosis of the condition and to aid management and recovery.
Accurately diagnosing concussion, also called mild traumatic brain injury (mTBI), can be tricky because the signs and symptoms associated with it can be subtle. There’s no obvious observable injury – such as with a broken bone or dislocation – and unless there’s been a bleed in the brain, brain imaging often cannot detect the condition.
Now, researchers led by Monash University have discovered that three proteins, specific biomarkers that occur following concussion, could be used as a global blood test for the condition.
“Concussion diagnosis is notoriously challenging in many cases because clinicians rely on subjective observations of physical signs and self-reported symptoms, neither of which are specific to concussion and often exhibit subtlety and rapid evolution,” said Stuart McDonald, corresponding author of the study. “Consequently, even in the ED [emergency department], individuals can be discharged without a definitive diagnosis. Our findings showed that the panel of biomarkers we assessed performed really well even in patients that lacked the more overt signs of concussion, such as loss of consciousness or post-traumatic amnesia.”
The researchers found that blood levels of three proteins – interleukin-6 (IL-6), glial fibrillary acidic protein (GFAP), and ubiquitin C-terminal hydrolase-L1 (UCH-L1) – each reflecting different aspects of the biology of brain trauma, could be used to precisely diagnose concussion in otherwise healthy patients under 50 who presented to the emergency department within six hours of injury.
There were 118 participants enrolled in the study, 74 with mTBI and 44 uninjured controls. Concussed patients self-reported the duration of memory loss immediately post-injury and were tested for intellectual functioning, memory performance and speed. Blood was taken to test plasma levels of IL-6, GFAP and UCH-L1 at under six hours post-injury and seven days post-injury.
The researchers then used software to determine the accuracy of each of the biomarkers.
They found that GFAP levels before six hours demonstrated good accuracy in distinguishing mTBI from controls and in participants with and without loss of consciousness or post-traumatic amnesia. At seven days, GFAP provided moderate/acceptable diagnostic utility. Under six hours, UCH-L1 had moderate/acceptable accuracy for distinguishing mTBI from controls and in participants with and without loss of consciousness or post-traumatic amnesia. At seven days, the biomarker provided moderate/acceptable utility. IL-6 was shown to have excellent utility for distinguishing mTBI from controls at under six hours and in patients with and without loss of consciousness or post-traumatic amnesia. By seven days, the diagnostic utility was restricted to female participants and those with loss of consciousness/post-traumatic amnesia.
The researchers found that when IL-6, an inflammatory biomarker, was measured alongside GFAP and UCH-L1, two proteins exclusive to the brain, this combination showed “incredible sensitivity and specificity” in distinguishing patients with a concussion from those without. They say the blood test could be used in different situations to improve diagnosis and enable earlier management of the condition.
“Within the ED, we believe the test might prove useful in providing certainty in difficult-to-assess cases, especially when a patient may be unwilling or unable to communicate their symptoms,” said Biswadev Mitra, one of the study’s co-authors. “One example could be in cases of domestic violence, where the test might reveal a mild brain injury that could otherwise go unnoticed.”
And, of course, the test would be useful for managing sport-related concussions, which occur regularly, especially in contact sports.
“While at this stage it might not be feasible to conduct a test that alters decisions within a match, players with a potential or suspected concussion that are removed from play could feasibly be tested soon after the match, with a more definitive diagnosis helping with many aspects of the player’s recovery and return-to-play process,” McDonald said.
In addition to the trio of biomarkers identified here, the researchers found that another – neurofilament light (NfL) – was elevated in the blood a week after the concussion and had comparable diagnostic properties.
“Beyond the ED, measures of blood NfL may be most beneficial when individuals consult a GP multiple days after an impact, especially in situations where diagnostic certainty is crucial for making safe return-to-work or return-to-play decisions, such as in military or sports settings,” said McDonald.
The study was published in the journal Neurology.
Source: Monash University