Infection
Cancer center’s anti-COVID efforts reduced nosocomial infections
October 09, 2023
2 min read
Source/Disclosures
Published by:
Disclosures:
Chemaly reports no relevant financial disclosures.
Key takeaways:
- Infection prevention efforts at a cancer center reduced some health care-associated infections during the pandemic.
- Infection rates that did not go down remained similar to pre-pandemic rates.
Enhanced infection prevention and control efforts during COVID-19 reduced the rates of some hospital infections at a comprehensive cancer center, including Clostridioides difficile and multidrug-resistant infections, according to a study.
After the onset of the pandemic, health facilities instituted a slew of infection prevention and control procedures in an effort to prevent the spread of SARS-CoV-2 in hospital wards. Although lab-confirmed C. difficile infections declined nationally in the United States, that was not the case across the board. Studies have shown that many health care facilities experienced a reversal in a years-long downward trend in hospital-acquired infections (HAIs).
“Previous large-scale studies revealed an alarming increase in some HAIs during the pandemic, which may be partly attributed to the necessary, dramatic shift in institutional [infection prevention and control] priorities,” Roy F. Chemaly, MD, MPH, chair of infectious diseases, infection control and employee health at the University of Texas MD Anderson Cancer Center, said in a press release.
“Our findings suggest that enhanced and targeted [infection prevention and control] measures enabled our facility to avoid these increases and, in several cases, significantly reduce the incidence of HAIs among our patient population during the pandemic,” he said.
Chemaly and colleagues analyzed surveillance data on monthly HAI rates for the roughly 30,000 patients per year admitted to the University of Texas MD Anderson Cancer Center from September 2016 to March 2022, comprising 42 months before the start of the pandemic and 25 months after its onset in March 2020.
They analyzed the data for rates of hospital-associated lab-identified C. difficile and multidrug-resistant organisms, device-related infections — catheter-associated UTIs (CAUTIs), central line-associated bloodstream infections (CLABSIs) and ventilator-associated events (VAEs) — and several nosocomial respiratory viral infections.
According to the study, MD Anderson employed mitigation strategies that included placing patients with COVID-19 in negative-pressure rooms in wards where contact and airborne isolation precautions were implemented; requiring all staff to wear N95 respirators, face shields, isolation gowns and gloves when entering a room for a patient with COVID-19; requiring face masks facilitywide for all employees, patients and visitors; and requiring all staff to wear face shields during periods of COVID-19 surge. Alcohol-based hand sanitizer was also widely available throughout the facility.
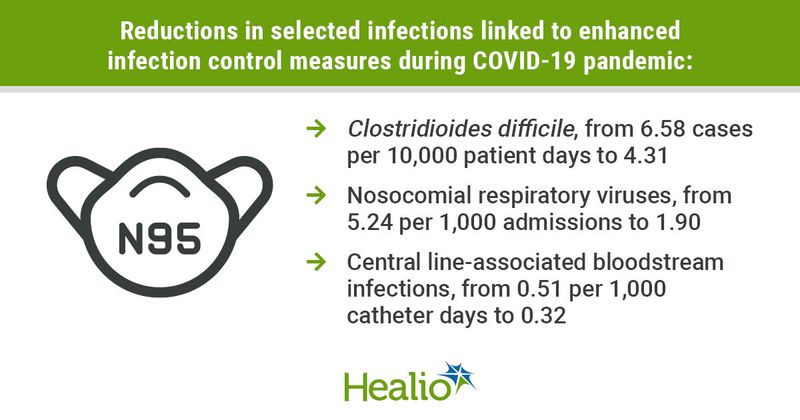
The data showed that MD Anderson’s C. difficile case rate decreased from 6.58 cases per 10,000 patient days to 4.31 cases per 10,000 patient days. For device-related infections, the incidence of CLABSIs declined from 0.51 to 0.32 per 1,000 catheter days, although the rates of CAUTIs and VAEs saw no significant change, according to the study.
The overall incidence rate of nosocomial respiratory virus infection also decreased significantly from 5.24 to 1.90 per 1,000 admissions, with a decrease seen for individually evaluated viruses, including influenza, metapneumovirus, parainfluenza, respiratory syncytial virus and rhinovirus, according to the study.
Additionally, the study found that overall incidence rates of multidrug-resistant infections were similar to that of the pre-pandemic to pandemic periods outside of COVID-19 wards but that rates in the wards were roughly five times higher than before the pandemic.
Chemaly and colleagues noted that although their analysis detected decreases in many types of HAIs, they were not able to determine the impact of individual infection prevention measures, adding that whether enhanced prevention methods should be used at all times during respiratory season — such as masking — requires more research.
Some experts, however, have already pointed to low rates of non-SARS-CoV-2 viral respiratory infections in 2020 and 2021 when universal masking was required at health care facilities as a reason to recommend that clinicians consider masking during elevated respiratory viral activity.