Blood
The Army is planning for a conflict with China—including shoring up blood supply
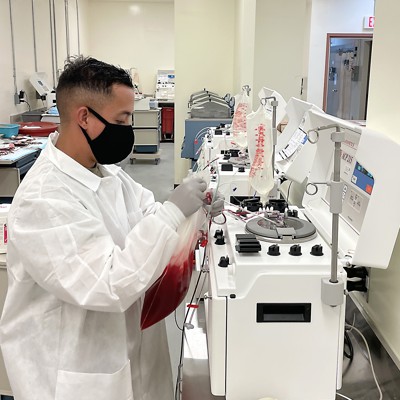
For the U.S. Army, preparing for war with China means more than training to fight—it also means making sure there is enough blood to keep soldiers and civilians alive across the Indo-Pacific.
“Blood supply and blood logistics is already challenging. And even coming out of COVID, we’re still facing a lot of manufacturing shortages, supply shortages,” said Maj. Nekkeya McGee, who runs a donation center for the Armed Services Blood Program and is a joint blood program officer 18th Medical Command, which serves the Indo-Pacific region.
Those shortages include the bags the blood is collected and stored in. So the military blood program is looking at alternate manufacturers to avoid a “single point of failure” during an emergency.
It’s just one part of a series of complicated things Army Medical Command must consider as it rehearses and plans for logistical challenges that could arise during a conflict in the Pacific region, an effort called Operation Pathways.
McGee, who is also the Army’s chief of transfusion medicine services, is in charge of figuring out how to move blood across the Indo-Pacific.
“A casualty is more likely to survive if they can receive blood products within an hour of injury,” McGee said, which means it’s crucial to have blood products available to increase survival rates.
One thing that can help with storage and supply to first aid stations is a battery-powered refrigerator prototype, McGee said.
The Armed Services Blood Program is also designing a new data collection system, called Theater Blood Mobile, which would replace the current legacy system. Once finalized, Theater Blood Mobile could improve how data is collected for pre-screening donation qualifications, infectious diseases, and blood transfusions downrange.
“We do a lot of data collection just to figure out how we can predict the need,” in an operational setting, she said. For example, when a surgical team is being deployed to a specific area, the Armed Services Blood Program can look at how many units of blood have been sent to and stored at that location in the past.
When working with partner nations to supply blood, the program must also look at the type of blood and how it was collected. They can do that through blood comparability studies that look at how collection and testing procedures in foreign countries match up to those in the U.S., which has guidelines set by the Food and Drug Administration.
“I take that information and that helps me determine should I establish a blood sharing agreement and try to pursue that route? Or do I try to pursue the route of training them how to safely collect blood products?” McGee said.
The challenge is compounded by blood donation shortages. The U.S. is in the midst of a blood shortage crisis—which includes the military—because it relies on civilian donations for backup supplies. The military donations are also affected by lack of staff, low donation numbers, and manufacturing problems, McGee said.
“Coming out of COVID, we have not been able to get the staffing that we need, including civilian facilities and civilian hires. The other part is the manufacturing, getting the products that we need, and people are just not coming out to donate,” McGee said. “I’m still meeting my quota. It’s difficult not because the arms aren’t out there. I don’t have the staff…I can send out five, but really, I would love to send out a team of seven because I could collect more units.”
The blood McGee’s center collects is primarily sent to areas the military operates, but the military can also use blood collected by civilian blood donation organizations, like the Red Cross, as a backup.
“We’ve been finding out that we have to rely on them a lot less, so you’ve got to make sure that what we’re collecting, we collect enough to send down range and take care of our facilities,” she said.
The goal is to make sure the Army is in the best position possible to fill blood supply needs in the event of a war with China. But getting there is a delicate balance of policy, cultural norms, relationships, and science and technology.
“We’ve got a range of things that we’re doing with blood from research and development with blood products, to blood sharing agreements with our partners, to innovative ways on how to deliver and distribute and store blood on the battlefield, to protocols for expeditionary blood and our walking blood bank programs,,” Maj. Gen. Paula Lodi, commanding general of the 18th Medical Command, said on Monday at the AUSA conference. “All four of those are pillars of how we’re getting after what we know is going to be a significant challenge for us in our theater.”
The Army is also looking at blood sharing agreements with partners in the region, though navigating associated policy challenges “is a big hurdle for us,” she told reporters.
“There are some nations where they want women to donate to women, men to donate to men. And you also gotta look at the blood types. The United States has a very heavy O-blood type,” McGee said. That’s not necessarily the case for other countries.
The military often relies on low-titer O whole blood for trauma transfusions because it’s easier to use and has a low risk of complications, but that isn’t the best fit for every type of injury.
“We have to be cognizant of that… we have to tailor it to whatever nation, that host nation we’re operating in,” she said. “That’s where those blood comparability studies come into play, because it covers all of that. And those are usually done by the Armed Services Blood Program now that the Indo-Pacific is becoming more important, a lot of those Asian countries are moving farther up as far as priority to get those things finished,” she said.
The Army is also looking at how to expand freeze-dried blood products to bolster blood supply. Right now, the military uses freeze-dried plasma that is collected and “spun down” domestically before it’s sent to France to be freeze-dried and returned to the U.S., McGee said.
Freeze-dried plasma is shelf-stable for up to a year, but manufacturing it in the U.S. still needs FDA approval.
The Armed Service Blood Program is looking into manufacturing and owning the whole process for freeze-dried blood products “and attaching it to a donor center, but that’s a few steps down the road.”
The plan is to test and experiment with U.S.-made freeze dried plasma in fiscal year 2024 as part of Operation Pathways exercises, McGee said. Researchers would look at how it carries, how it can be reconstituted, and how easy it is to use—but would stop short of transfusing it into a person.