Bleeding under the skin that produces a blotchy or pinprick-like rash may signal a serious bacterial infection.
If you ever happen upon a peculiar rash, resembling pink or purple pinpricks on your skin, it’s paramount not to disregard it. This seemingly innocuous rash can be a telltale symptom of bacterial meningitis, a grave medical condition that demands immediate attention. Dr. Frank Esper, a pediatric infectious disease specialist at Cleveland Clinic Children’s Hospital, aptly emphasizes the severity of bacterial meningitis, explaining that it incites profound inflammation in and around the brain, thereby classifying it as a dire concern.
It is worth noting that while a rash can indeed signal bacterial meningitis, various factors, including less severe health conditions, chemicals, cosmetics, dyes, and even poison ivy, can also give rise to similar rashes, as asserted by Penn Medicine. In the following discourse, we will delve into bacterial meningitis, offering insights into its nature, symptoms, causes, identification of a meningitis rash, and preventive measures, underscoring the significance of prompt and informed action.
Understanding Bacterial Meningitis
Bacterial meningitis ensues when specific bacteria infiltrate the cerebrospinal fluid, triggering severe swelling within a cluster of protective membranes known as the “meninges,” which envelop and safeguard the brain and spinal cord, as delineated by Nemours Children’s Health. The Centers for Disease Control and Prevention (CDC) further elucidate that the transmission of bacteria responsible for meningitis can occur through various means. These include transmission from mother to infants during childbirth, via saliva exchange (such as through kissing or coughing), or even via the consumption of food prepared by individuals who failed to practice proper hand hygiene after using the restroom.
In comparison to viral meningitis, which is more prevalent and often self-resolves without intervention, bacterial meningitis poses a more imminent threat. The CDC underscores the rapid progression of bacterial meningitis, which can prove fatal within a few hours. Furthermore, survivors of this condition may grapple with long-term consequences, including hearing impairment, brain damage, and learning disabilities.
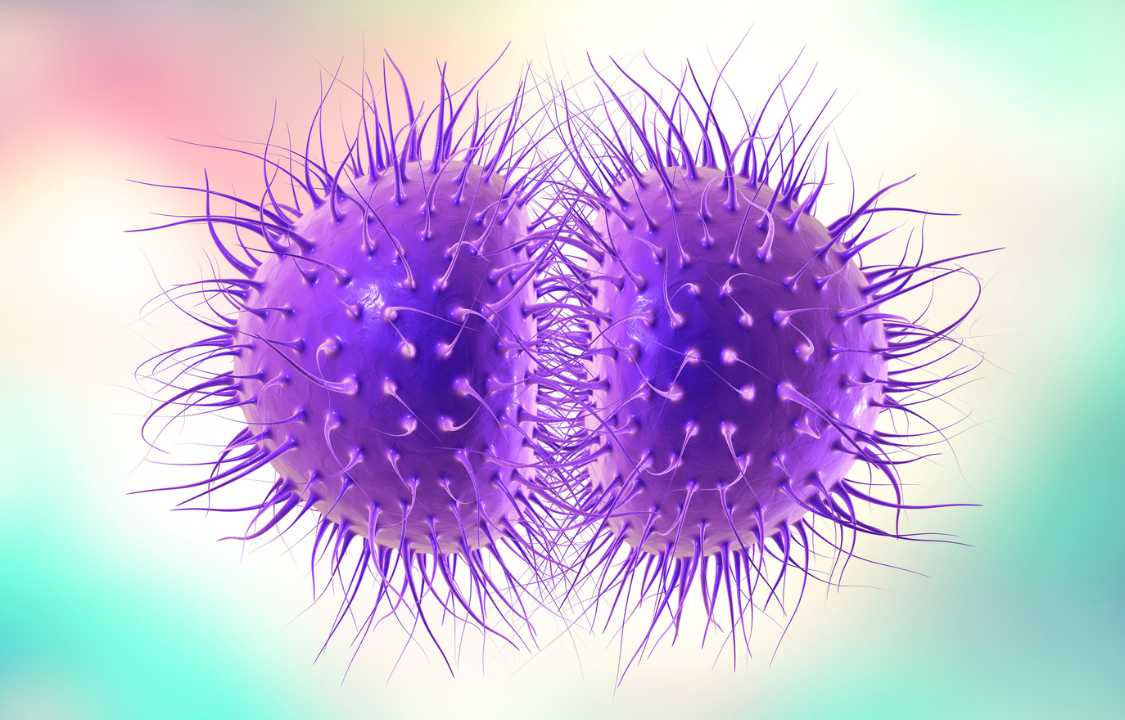
Notably, several types of bacteria have the potential to cause meningitis. However, the National Organization for Rare Disorders (NORD) reports that three specific types are responsible for the majority of cases, including Hemophilus influenzae (type b), Streptococcus pneumoniae (pneumococcus), and Neisseria meningitidis (meningococcus). It is the latter, meningococcus, that often manifests as the meningitis rash, as expounded by the Meningitis Research Foundation. Dr. Esper underscores the unsettling nature of meningococcus, noting that it is the pathogen that most healthcare professionals find particularly worrisome.
Remarkably, about one in ten individuals harbor meningococcal bacteria in their nasal passages or throat without experiencing any illness. Yet, these asymptomatic carriers can still transmit the bacteria to others through close contact or respiratory secretions, potentially resulting in infection. The CDC highlights that particular demographics, such as infants and college students, face elevated risk levels. In fact, Claire Wright, an evidence and policy manager at the Meningitis Research Foundation, draws attention to the heightened transmission rates among college students residing in close quarters and engaging in social activities.
Nevertheless, bacterial meningitis can affect anyone, regardless of age or lifestyle. Consequently, it is imperative that individuals exhibiting symptoms, such as a potential meningitis rash, seek immediate medical attention.
Deciphering the Meningitis Rash
Identifying a meningitis rash can be a nuanced task, as its appearance can vary from person to person. The Meningitis Research Foundation outlines two primary categories of meningitis rashes: the “petechial” rash, characterized by red or purple pinpricks reminiscent of flea bites, and the “purpuric” rash, which resembles a bruise and manifests as reddish-purple blotches on the skin.
These rashes, often erroneously referred to as true rashes, tend to appear initially on the arms, legs, or trunk, as reported by NORD. Notably, they may also cluster in areas prone to pressure, such as the waistband of underwear or socklines, as highlighted by the Meningitis Research Foundation.
It is crucial to comprehend that the so-called meningitis rash is not a traditional rash but rather the result of bleeding beneath the skin’s surface. This occurs when pathogens, frequently Meningococcal bacteria, infiltrate the bloodstream and inflict damage on blood vessels and organs, as elucidated by the Meningitis Research Foundation.
In cases where a meningitis rash spreads rapidly, it may indicate a severe condition necessitating immediate medical intervention. The Meningitis Research Foundation underscores that as the infection advances, blood vessels may begin to leak. Consequently, the body initiates clotting processes to stem the bleeding. However, this can lead to oxygen deprivation in extremities like the hands and feet, ultimately causing severe scarring and potentially necessitating amputation.
Identifying a Meningitis Rash: The Tumbler Test
A valuable tool for discerning a meningitis rash is the “tumbler test,” also known as the “glass test,” as proposed by the Meningitis Research Foundation. This straightforward method entails gently pressing a clear glass tumbler, akin to those commonly found in kitchen cabinets, onto the suspected rash.
Should the rash fail to fade and remain visible through the glass, immediate medical attention is imperative, as articulated by Claire Wright. Rashes that maintain their visibility upon pressure are classified as “non-blanching” rashes. While the meningitis rash typically begins as a “blanching” rash, it frequently progresses to the non-blanching stage, as described by the Meningitis Research Foundation.
Moreover, it is essential to appreciate that the manifestation of a meningitis rash can exhibit variations across different skin types. Furthermore, in some instances, individuals with the disease may not develop a meningitis rash at all. Hence, it remains crucial to remain vigilant regarding other symptoms and promptly seek medical care if meningitis is suspected.
Symptoms of Bacterial Meningitis
The presence of a rash is merely one facet of bacterial meningitis, which presents a constellation of symptoms. Dr. Esper emphasizes the uniformity of symptoms among individuals with meningitis, characterizing the experience as one dominated by intense headache, heightened sensitivity to light, and discomfort due to heightened brain agitation. According to the CDC, bacterial meningitis can also elicit symptoms such as fever, stiff neck, nausea, vomiting, and confusion.
In the case of newborns and infants, the manifestations of bacterial meningitis differ somewhat. The CDC advises parents and caregivers to remain vigilant for signs including sluggish movements, irritability, vomiting, reduced appetite, bulging in the “soft spot” (fontanelle) of the infant’s head, abnormal reflexes, and other atypical behaviors.
Furthermore, it is crucial to recognize that specific types of bacterial meningitis can also instigate sepsis. Sepsis occurs when bacteria enter the bloodstream and commence replication, resulting in damage. Toxins produced by these bacteria can weaken capillaries, leading to blood leakage, which ultimately manifests as the meningitis rash, as elucidated by the Meningitis Research Foundation.
Preventing Bacterial Meningitis
The most effective method of averting bacterial meningitis is vaccination, as highlighted by the CDC. Vaccines are available for several of the most perilous strains of bacterial meningitis, encompassing pneumococcal, Haemophilus influenzae, and meningococcal varieties. Claire Wright underlines the paramount importance of obtaining available vaccines, asserting that it constitutes the most critical preventive measure.
While vaccines offer robust protection, it is essential to recognize that no vaccine, regardless of the disease it targets, guarantees complete immunity. Therefore, the CDC advocates for the practice of additional healthy habits to safeguard oneself and others from bacterial meningitis. These measures encompass maintaining physical distance from individuals displaying illness symptoms, refraining from exposure to cigarette smoke, ensuring adequate sleep, meticulous hand hygiene, and the use of tissues when coughing or sneezing.
In Conclusion
Bacterial meningitis is a formidable adversary, affecting between 600 and 1,000 individuals each year, as reported by the National Meningitis Foundation. Of those afflicted, a devastating 10-15% succumb to its dire consequences, while one in five survivors grapple with lifelong disabilities, including brain impairment, hearing loss, or even amputations. Consequently, it is incumbent upon individuals to remain vigilant, promptly recognize symptoms such as a rash, and undertake necessary measures to curtail the spread of bacterial meningitis.