Cardiovascular
Substance abuse in OSA raises odds for cardiovascular, cerebrovascular events
October 13, 2023
2 min read
Key takeaways:
- The odds for serious cardiovascular and cerebrovascular events went up in young patients with obstructive sleep apnea and substance abuse.
- Higher odds were found in women vs. men.
HONOLULU — Young patients with obstructive sleep apnea faced heightened odds for major adverse cardiovascular and cerebrovascular events if they abused drugs, according to an abstract presented at the CHEST Annual Meeting.
“Early screening of substance abuse in young OSA patients may reduce the risk of major adverse cardiovascular and cerebrovascular events (MACCE),” Laxman Yashwant Byreddi, MBBS, MD, assistant professor of medicine at Louisiana State University Health Sciences Center, and colleagues wrote. “This study can be helpful for clinicians to better counsel the targeted population against substance use and discuss alternative treatment options for sleeplessness in OSA.”
In a nationwide analysis, Byreddi and colleagues analyzed 175,915 hospital admissions of young patients aged 18 to 44 years with OSA from the National Inpatient Sample in 2020 to determine the sociodemographic characteristics and comorbidities seen among substance abusers, as well as the impact drug abuse has on MACCE.
Researchers observed drug abuse in 11,880 (6.8%) hospitalizations.
Looking at baseline demographics, the median age of the total cohort was 38 years, and substance abusers vs. nonabusers tended to be men (64% vs. 52.1%), white (57.9% vs. 55.3%) and Medicaid enrollees (51% vs. 31.8%). Patients who abused drugs also had a slightly longer median hospitalization duration (4 days vs. 3 days).
Between patients with and without substance abuse, researchers found significant differences in the prevalence of several comorbidities, including anxiety disorder (37.8% vs. 25.7%; P < .001), chronic pulmonary disease (35.1% vs. 27.5%; P < .001), psychosis (10.9% vs. 3.4%; P < .001), prior venous thromboembolism (9.3% vs. 7.2%; P < .001), prior myocardial infarction (4.2% vs. 2.7%; P < .001), prior transient ischemic attack (3.3% vs. 3%; P < .048), peripheral vascular disease (2.4% vs. 2.1%; P < .001) and AIDS (1.5% vs. 0.6%; P < .001).
Despite the greater prevalence of the above comorbidities in substance abusers, fewer patients from this cohort had obesity (63.1% vs. 73.5%), hyperlipidemia (23% vs. 27.9%), diabetes (29.3% vs. 32.6%) and hypothyroidism (8.8% vs. 10.7%; all P < .001).
Notably, more patients with vs. without substance abuse experienced in-hospital outcomes, such as acute myocardial infarction (4.4% vs. 2.7%), cardiac arrest (1.7% vs. 0.9%) and mortality (1.4% vs. 1.1%; all P < .001).
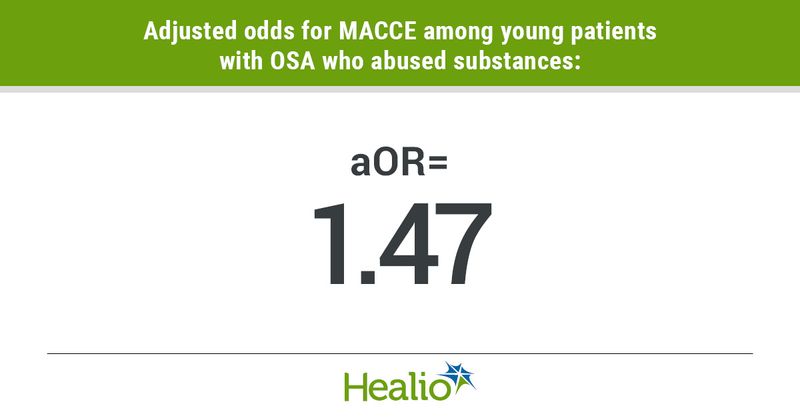
MACCE was also more prevalent in those who abused substances (7.1% vs. 5%; P < .001), equating to heightened odds for MACCE in this group of patients (adjusted OR = 1.47; 95% CI, 1.21-1.78) following adjustments for demographic, hospital and clinical variables.
Young women with substance abuse had a higher risk for MACCE than young men with substance abuse (OR = 2.38; 95% CI, 1.73-3.29), according to researchers. In terms of race, the risk for MACCE was high in both white patients who abused drugs (OR = 1.62; 95% CI, 1.25-2.1) and Black patients who abused drugs (OR = 1.54; 95% CI, 1.08-2.2).
“More studies are required to understand the role of gender and racial disparities,” Byreddi and colleagues wrote.