Cardiovascular
Pregnancy complications increase and unmask cardiovascular risks in obese patients in NIH study
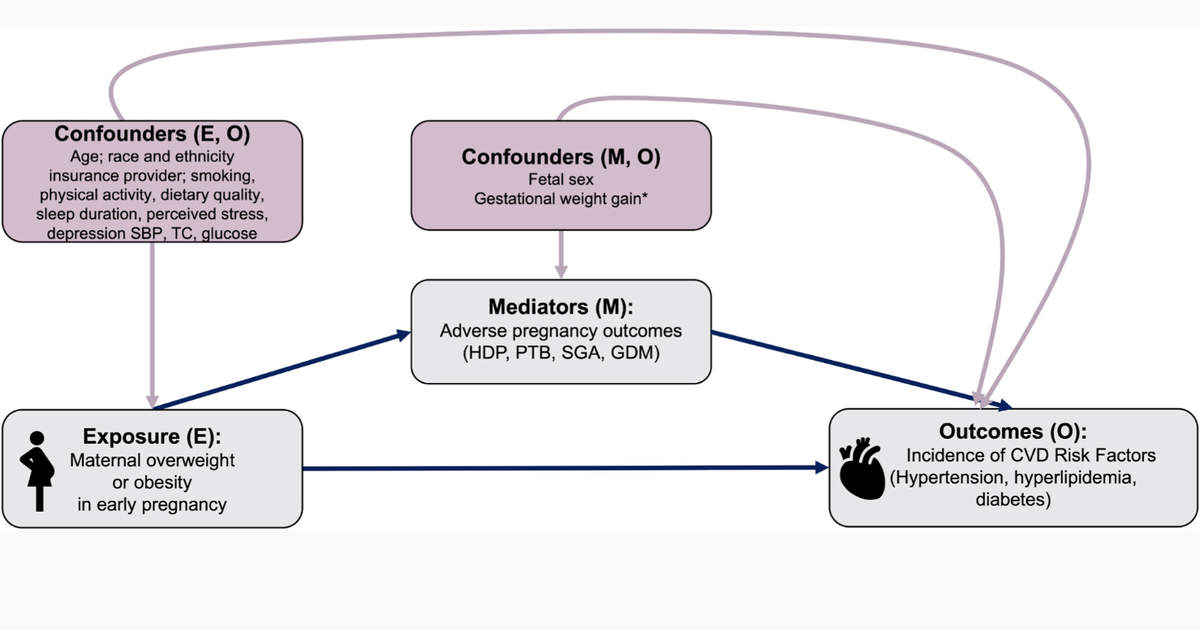
National Institutes of Health (NIH) supported research is providing a broader understanding of how cardiovascular disease risk manifests following pregnancy. Having obesity before and during early pregnancy appears to be a strong indicator of risk for developing future cardiovascular disease. It also was significantly linked with adverse outcomes during pregnancy, such as high blood pressure, preeclampsia and gestational diabetes, according to the study published in Circulation Research.[1]
There was heterogeneity across apolipoprotein (APO) subtypes in their association with postpartum CVD risk factors and mediation of the association between early pregnancy obesity and postpartum CVD risk factors. However, only a small or nonsignificant proportion of the association between obesity and CVD risk factors was mediated by any of the APOs, suggesting APOs are a marker of prepregnancy CVD risk and not a predominant cause of postpartum CVD risk.
While having adverse pregnancy outcomes was linked with increased cardiovascular disease risks during pregnancy, the complications accounted for a small percentage of increased cardiovascular disease risks in the years following pregnancy for people with obesity. Researchers have known obesity is a risk factor for cardiovascular disease and pregnancy complications related to blood pressure. However, they did not know which factors – obesity or the pregnancy complications – played larger roles in influencing a person’s cardiovascular disease risk years after pregnancy.
“We’re finding that certain pregnancy complications are unmasking and then increasing cardiovascular disease risks, such as obesity, that were already present. This study provides insight into potential timing for interventions for people with overweight or obesity who are thinking about pregnancy,” said Victoria Pemberton, RNC, a study author and researcher in the Division of Cardiovascular Sciences at the National Heart, Lung, and Blood Institute (NHLBI), part of NIH, said in a statement.
The researchers analyzed data collected from on 4,216 patients in the Nulliparous Pregnancy Outcomes Study: Monitoring Mothers-To-Be (nuMoM2b) Heart Health Study. These were first-time mothers and about half were overweight or obese. They compared the participants’ pregnancy experience to their health two to seven years later. They found mothers who were overweight or had obesity during the first trimester of pregnancy had about twice the risk for developing gestational diabetes or having a pregnancy complicated by high blood pressure, compared to participants with a normal body weight. These mothers also had increased risks for developing cardiovascular disease risks after pregnancy.
The sample included adults with an average age of 27. Early pregnancy prevalence of overweight was 25%, and obesity was 22%. Hypertensive disorders of pregnancy occurred in 15%, preterm birth in 8%, small-for-gestational-age birth in 11%, and gestational diabetes in 4%. Early pregnancy obesity, compared with normal body mass index, was associated with significantly higher incidence of postpartum hypertension, hyperlipidemia and diabetes, even after adjustment for baseline CVD risk factor levels.
In comparison, pregnancies complicated by high blood pressure explained just 13% of future risks for developing high blood pressure if a person had obesity. Likewise, gestational diabetes explained only 10% of future risks for diabetes.
“We want to do everything we can to support a person’s heart health, but especially around the time of pregnancy – before, during, and in early pregnancy,” said Sadiya Khan, MD, the study’s lead investigator, a preventive cardiologist, and an associate professor of medicine at Northwestern University Feinberg School of Medicine, said in the same NIH statement. “That includes achieving and maintaining a healthy body weight, knowing your heart health numbers, and finding ways to stay physically active.”
For some complications the researchers found body weight did not factor into risks. For example, people with overweight or obesity did not have increased risks for having a preterm birth or a baby with a low birthweight. They also found among all participants, those experiencing preterm births had increased risks for having high blood pressure, high blood sugar, or high cholesterol a few years after pregnancy. Having a baby born with a low birthweight was not found to increase risks, the authors said.
“Looking for ways to support and optimize a person’s cardiovascular health is still of the utmost importance if someone has had an adverse pregnancy outcome,” said Khan. “However, if we really want to make a difference in improving cardiovascular health and preventing these pregnancy outcomes, we have to shift to the pre-pregnancy and early pregnancy space.”