Infection
Fungal Infections in The Brain May Cause Alzheimer’s-Like Symptoms
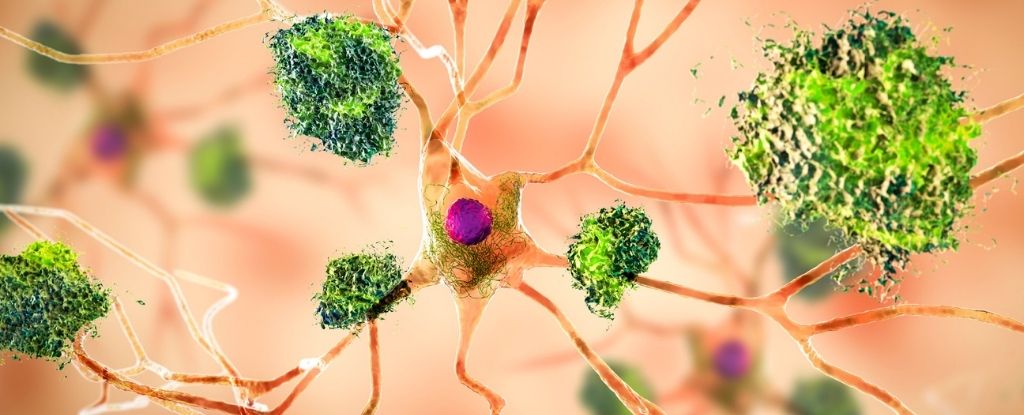
A common type of fungi has now been shown to penetrate the mammal brain and trigger toxic amyloid plaques like those associated with Alzheimer’s disease.
The findings were made among mice, but the research suggests that a key hallmark of some neurodegenerative conditions could originate from sources outside the brain.
Amyloid protein clumps that show up between neurons are strongly associated with Alzheimer’s disease, and are generally thought to be the result of intrinsic stress or inflammation in the brain.
In recent years, however, scientists have detected signs of a common fungus, known as Candida albicans, in the autopsied brains of people with Alzheimer’s and other neurodegenerative disorders, like Parkinson’s.
This has led some to argue that external infections can invade the mammal brain and elicit an innate immune response, which can help destroy pathogens but which may also trigger Alzheimer’s-like symptoms if it goes wrong.
To explore that idea further, an international team of researchers, led by experts at Baylor College of Medicine in the United States, has turned to mice.
Previously, the same lab at Baylor found that mice infected with C. albicans showed impairments in memory, but these resolved when the fungus was cleared.
Now, their new research explores the molecular basis of that effect, mostly through ‘test-tube’ experiments.
First, researchers injected C. albicans straight into the brains of mice. Four days later, the mice were euthanized and their brains were used for further analysis.
Several brain slices were imaged and some cells were cultured on plates.
The findings suggest that once in the brain, C. albicans can trigger two neuroimmune mechanisms, one which activates immune cells that suppress the fungi, and another that triggers them into removing the intruder altogether.
The first mechanism involves a fungal enzyme called Saps, which makes the blood-brain barrier extra leaky. This allows any fungal cells that may be flowing through the body’s bloodstream into the brain.
At the same time, Saps also breaks apart amyloid beta-like proteins similar to the ones that form plaques in Alzheimer’s brains, which in turn activate clean-up cells called microglia.
The second mechanism involves another fungal secretion, which also triggers microglia, this time into targeting the fungi for removal.
Together, both immune pathways are “highly effective in resolving acute C. albicans” infections in healthy mice brains, usually doing so in about 10 days.
But not all brains are young and healthy. When researchers purposefully disrupted the microglia response in mouse brains, they found that C. albicans infections became markedly prolonged.
“If we take away this pathway, fungi are no longer effectively cleared in the brain,” says Yifan Wu from Baylor College of Medicine.
The amyloid beta-like clumps found in mouse brains appear to be sentinels against pathogen invasion, but if these clumps aren’t cleaned up properly by microglia, it’s possible their presence could prove harmful in the long run.
For now, that is just a hypothesis, but it does align with recent findings that indicate amyloid beta plaques are latecomers in Alzheimer’s disease, not the original triggers of cognitive decline.
This could be why treatments that target these plaques in humans mostly prove unsuccessful.
“This work potentially contributes an important new piece of the puzzle regarding the development of Alzheimer’s disease,” says immunologist David Corry, who led the research at Baylor.
“The dominant thinking is that these peptides are produced endogenously, our own brain proteases break down the amyloid precursor proteins generating the toxic amyloid beta peptides.”
But that may not be the case after all.
Far more research needs to be done, both on living animal models and on human cells, but researchers at Baylor are hopeful that their initial experiments can lead to innovative therapies for cognitive decline in the future.
The study was published in Cell Reports.