Blood
$6 million grant from the Department of Defense awarded to UAB to study the use of whole blood resuscitation in trauma patien
Grant will further investigate the recent evidence from military and civilian medicine that suggests outcomes may be better when trauma patients receive whole blood, instead of previously separated blood products.
Media contact: Anna Jones
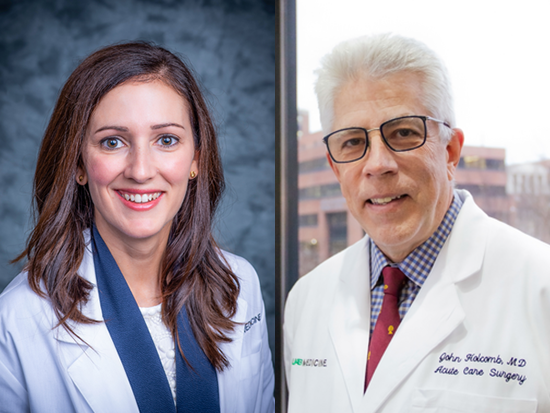
Jillian Richter, Ph.D., and John Holcomb, M.D., from UAB’s Center for Injury Science will use this grant to conduct a mechanistic study called bioTROOP.Traumatic injury is a leading cause of death, and about one-third of injury-related deaths are caused by bleeding. Researchers at the University of Alabama at Birmingham Marnix E. Heersink School of Medicine have received a $6.38 million grant from the Department of Defense to examine how trauma patients respond to different resuscitation strategies using whole blood.
Jillian Richter, Ph.D., and John Holcomb, M.D., from UAB’s Center for Injury Science will use this grant to conduct a mechanistic study called bioTROOP that will be conducted alongside the NHLBI-funded, $8.2 million, multicenter randomized clinical trial called “Trauma Resuscitation with Group O Whole Blood or Products,” also known as TROOP.
The TROOP trial, which began in 2022, is led by CIS director Jan Jansen, Ph.D., and evaluates the effectiveness of whole blood, compared to component therapy, in trauma patients predicted to require large-volume blood transfusions. TROOP is the first large-scale randomized clinical trial to evaluate whole blood in injured patients, and its findings could change the standards of care of injured patients.
The traditional approach for treating injured patients who are bleeding is to transfuse multiple separate units of red blood cells, plasma and platelets. However, recent evidence from military and civilian medicine suggests outcomes may be better when patients receive whole blood, instead of previously separated blood products.
The newly funded bioTROOP study will evaluate mechanistic aspects of whole blood resuscitation. It will leverage the TROOP trial’s existing infrastructure to collect blood samples from enrolled subjects. Specifically, bioTROOP will determine whether resuscitation with whole blood affects blood coagulation and clot formation. Richter and her team will measure metabolic and immune responses after injury to determine whether whole blood may reduce complications such as organ damage or sepsis.
The bioTROOP study will enroll 400 TROOP trial subjects over a two-year period at seven sites within the 14-site clinical TROOP network.
Richter, bioTROOP’s principal investigator and associate director of the Basic Science and Translational Research Unit for the CIS, says the bioTROOP study is an unprecedented opportunity to gain new insights into transfusion strategies.
“Findings from this study will contribute new knowledge regarding the human response to trauma, bleeding and resuscitation,” said Richter, an associate professor in the UAB Division of Trauma and Acute Care Surgery. “This information will benefit patients worldwide and help doctors, in both military and civilian settings, to optimize transfusion approaches to increase survival from severe bleeding caused by traumatic injury.”
The CIS was founded in 1999 and conducts research to improve trauma care. Its mission is to promote injury prevention and improve outcomes from injury at all stages of care, from the pre-hospital setting to resuscitation, acute care and rehabilitation. Clinicians from many specialties — including trauma surgeons, emergency medicine physicians, anesthesiologists, intensivists and rehabilitation specialists — work closely with epidemiologists, basic scientists, biostatisticians, health economists, health psychologists and methodologists.
The TROOP trial and bioTROOP study are run by the center’s Clinical Trials Unit and the Basic Science and Translational Research Unit.