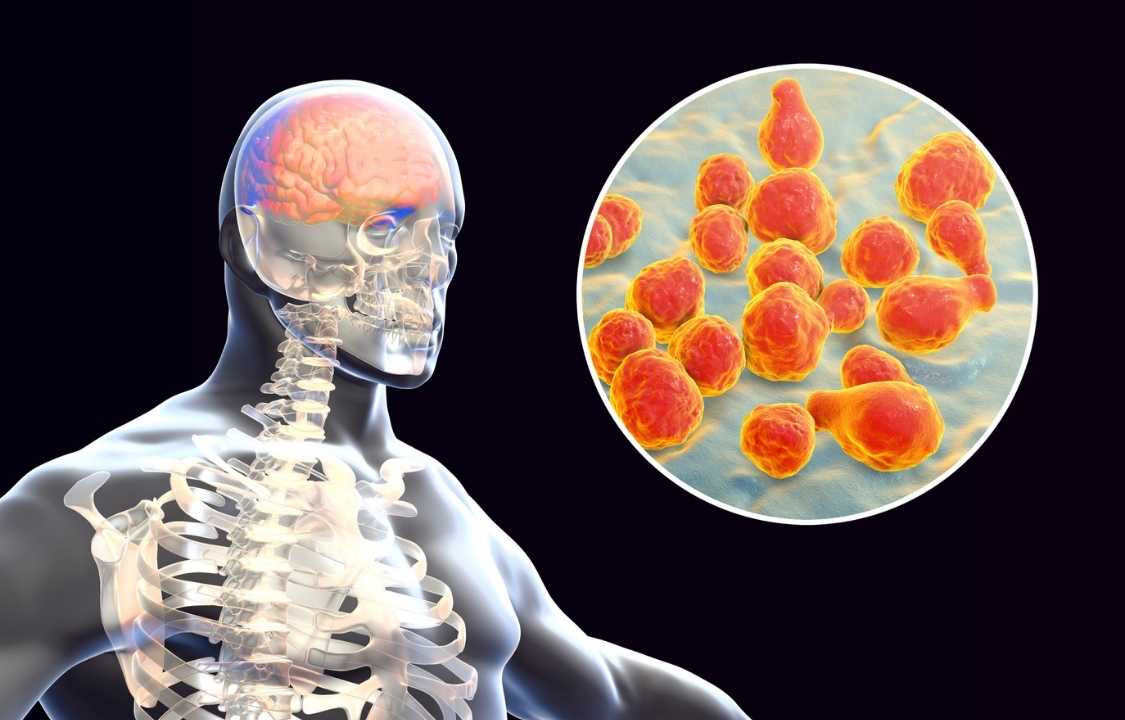
Brain, Disease, Inflammation
What Is Meningitis?
Meningitis, a term that encompasses the inflammation of the meninges, those crucial protective layers enshrouding the brain and spinal cord, is a medical condition of paramount significance. This ailment can be provoked by various pathogens, including bacteria, fungi, and viruses. According to global estimates, approximately 1.2 million individuals worldwide grapple with bacterial meningitis each year, underscoring the gravity of this medical concern.1
In this comprehensive exploration, we venture into the multifaceted realm of meningitis, delving into its diverse symptoms, causative factors, diagnostic modalities, treatment strategies, and preventive measures. Understanding meningitis in-depth is vital, as it empowers individuals to recognize the condition’s manifestations, seek timely medical intervention, and appreciate the pivotal role of vaccination in safeguarding against its perils.
The Myriad Faces of Meningitis: Symptoms and Their Evolution
Meningitis often unveils itself through a spectrum of symptoms that may initially masquerade as benign ailments, such as a common cold or influenza. However, over time, these symptoms can evolve into more grave neurological manifestations, signifying the escalation of the condition. Recognizing these symptoms is pivotal, as it dictates the urgency of medical intervention.
Common symptoms of meningitis encompass:
1. Infection Symptoms: Fever, fatigue, chills, and body aches – the body’s innate response to invading pathogens.
2. Neurological Symptoms: Confusion, double vision, dizziness, and seizures – indicative of the condition’s impact on brain function.
3. Stomach Symptoms: Loss of appetite, diarrhea, nausea, and vomiting – often due to the overall distress caused by the infection.
4. Pain Symptoms: Neck pain, muscle aches, joint discomfort, and abdominal pain – reflective of the systemic impact of meningitis.
5. Skin Symptoms: A skin rash characterized by red or purple pinpricks or splotches, typically emerging in the later stages of the disease.
A particularly alarming symptom associated with bacterial meningitis is the development of a rash, which can serve as a red flag signaling a medical emergency. This rash materializes when bacteria damage blood vessels, causing them to leak and produce the distinctive skin discolorations.1
Unmasking the Culprits: What Causes Meningitis?
Bacteria stand as the predominant culprits behind the onset of meningitis. This infection takes root when immune system cells or compromised blood vessels permit the entry of bacteria or other pathogens into the cerebrospinal fluid (CSF). The CSF, located within the confines of the brain and spinal cord, plays a pivotal role in cushioning these vital organs. When bacteria infiltrate the CSF and meninges, the clinical manifestations of meningitis ensue.2
Several strains of bacteria have been identified as triggers for meningitis, including Escherichia coli, Group B streptococcus, Listeria monocytogenes, Neisseria meningitidis, and Streptococcus pneumoniae. Although bacterial meningitis assumes the lion’s share of cases, other pathogens, such as enteroviruses, fungi, mumps, amoeba, parasites, and occasionally tuberculosis, can also precipitate the condition.
Navigating Risk Factors: Who is Prone to Meningitis?
Meningitis does not discriminate based on age, but certain factors can heighten an individual’s susceptibility to the condition. These risk factors encompass:
1. Age: Being under the age of 5 places individuals at a heightened risk, as their immune systems are still developing and may not effectively combat infections.
2. Immune System Vulnerability: Individuals with weakened immune systems or autoimmune diseases face an increased risk. Additionally, those taking immunosuppressive medications like steroids or undergoing chemotherapy may be more susceptible.
Diagnosing Meningitis: The Journey to Certainty
Diagnosing meningitis necessitates a meticulous evaluation by a healthcare provider. The diagnostic process typically encompasses:
1. Medical History: A comprehensive inquiry into an individual’s personal and familial medical history to uncover potential predispositions or prior occurrences.
2. Physical Examination: Scrutiny of presenting symptoms and physical signs that may hint at meningitis.
3. Lumbar Puncture: A critical procedure involving the extraction of cerebrospinal fluid (CSF) to detect the presence of pathogens.
4. Imaging Tests: CT scans or MRIs to visualize the brain and identify signs of inflammation or damage.
5. Blood Tests: Assessment of blood samples to identify specific proteins or pathogens that may be indicative of the infection.
In certain cases, healthcare providers may perform specialized physical assessments targeting the central nervous system. These include:
- Brudzinski’s Sign: A test for severe neck stiffness, where pain is elicited when the knees are tucked into the chest as the neck flexes.
- Kernig’s Sign: Evaluation for discomfort when the hips are flexed to a 90-degree angle and pain is experienced upon extending the knee from that position.
These tests collectively form a comprehensive diagnostic approach that enables healthcare providers to ascertain the presence of meningitis and its underlying cause, facilitating the formulation of an appropriate treatment plan.2
Crafting a Path to Recovery: Meningitis Treatment Strategies
The choice of treatment for meningitis hinges on the severity of the condition and the identity of the causative pathogen. Treatment modalities include:
1. Antibiotics: Employed in cases of bacterial meningitis to combat the bacterial infection effectively.
2. Antifungal Medication: Administered when fungal meningitis is identified as the culprit.
3. Antiviral Medication: Utilized for viral meningitis to curtail the viral infection.
4. Pain Relievers: Prescribed to alleviate the discomfort associated with meningitis.
5. Steroid Medication: Employed to reduce swelling, especially when neurological symptoms are severe.
The selection of the appropriate treatment strategy underscores the importance of a timely and accurate diagnosis.
Guardians of Health: Preventing Meningitis
Prevention serves as the most formidable weapon against meningitis, and vaccination emerges as the cornerstone of this defense. The meningococcal vaccine stands as a stalwart shield, with the Centers for Disease Control and Prevention (CDC) recommending its administration at key junctures in life:
- Meningococcal Conjugate Vaccine (MenACWY): Administered during adolescence, with a booster dose at age 16.
- Serogroup B Meningococcal Vaccine (MenB): Recommended for individuals aged 16 to 23.
Moreover, other vaccines offer protection against bacteria that can trigger meningitis, including Haemophilus influenzae serotype B (Hib), influenza (flu) vaccines, and pneumococcal vaccines. Embracing these immunizations fortifies the collective defense against meningitis. Additionally, prudent preventive measures include:
- Limiting Close Contact: Avoiding proximity to individuals with meningitis or other contagious infections.
- Hand Hygiene: Practicing frequent handwashing with soap and water, especially after using the toilet, coming into contact with stool, changing diapers, or touching contaminated surfaces.
- Respiratory Hygiene: Covering one’s mouth when sneezing or coughing to prevent the spread of infection.
Related Conditions and Meningitis: A Complex Interplay
Certain underlying medical conditions can elevate an individual’s vulnerability to meningitis. These conditions encompass:
- Cerebrospinal Fluid (CSF) Leak: A breach in the protective CSF barrier.
- Splenectomy: Surgical removal of the spleen.
- HIV Infection: A compromised immune system can heighten susceptibility.
- Behcet’s Disease: An autoimmune disorder that can contribute to increased risk.
- Sarcoidosis: An inflammatory condition.
- Sjogren’s Syndrome: An autoimmune disorder.
- Systemic Lupus Erythematosus (Lupus): Another autoimmune disorder.
Moreover, specific medications, such as non-steroidal anti-inflammatory drugs (NSAIDs), antibiotics, and intravenous immunoglobulins (IVIG), can also elevate the risk of developing meningitis.7
Navigating Life with Meningitis: A Path to Recovery
For individuals grappling with symptoms of meningitis, timely communication with a healthcare provider is paramount. Swift medical intervention ensures an accurate diagnosis and the initiation of appropriate treatment regimens to alleviate symptoms.
Unfortunately, approximately 30% of individuals affected by meningitis may encounter neurological complications, including memory problems, seizures, and hearing loss. However, early intervention and treatment can significantly mitigate these challenges. The advent of meningitis vaccines has played a pivotal role in reducing the overall incidence of this condition and its associated complications, underscoring the profound impact of preventive measures in preserving health and well-being.
In conclusion, meningitis is a multifaceted medical condition that warrants meticulous attention and understanding. The ability to recognize its diverse symptoms, appreciate its underlying causes, seek timely diagnosis and treatment, and embrace preventive measures through vaccination empowers individuals to safeguard themselves against the formidable threat posed by meningitis. With knowledge and vigilance, we can collectively navigate the complex landscape of this condition, reducing its impact and improving the prospects of those affected.