Infection
COVID-19 increases Alzheimer’s risk
In a recent review published in the Journal of Neurochemistry, researchers evaluate the impact of the coronavirus disease 2019 (COVID-19) on Alzheimer’s disease (AD) pathology.
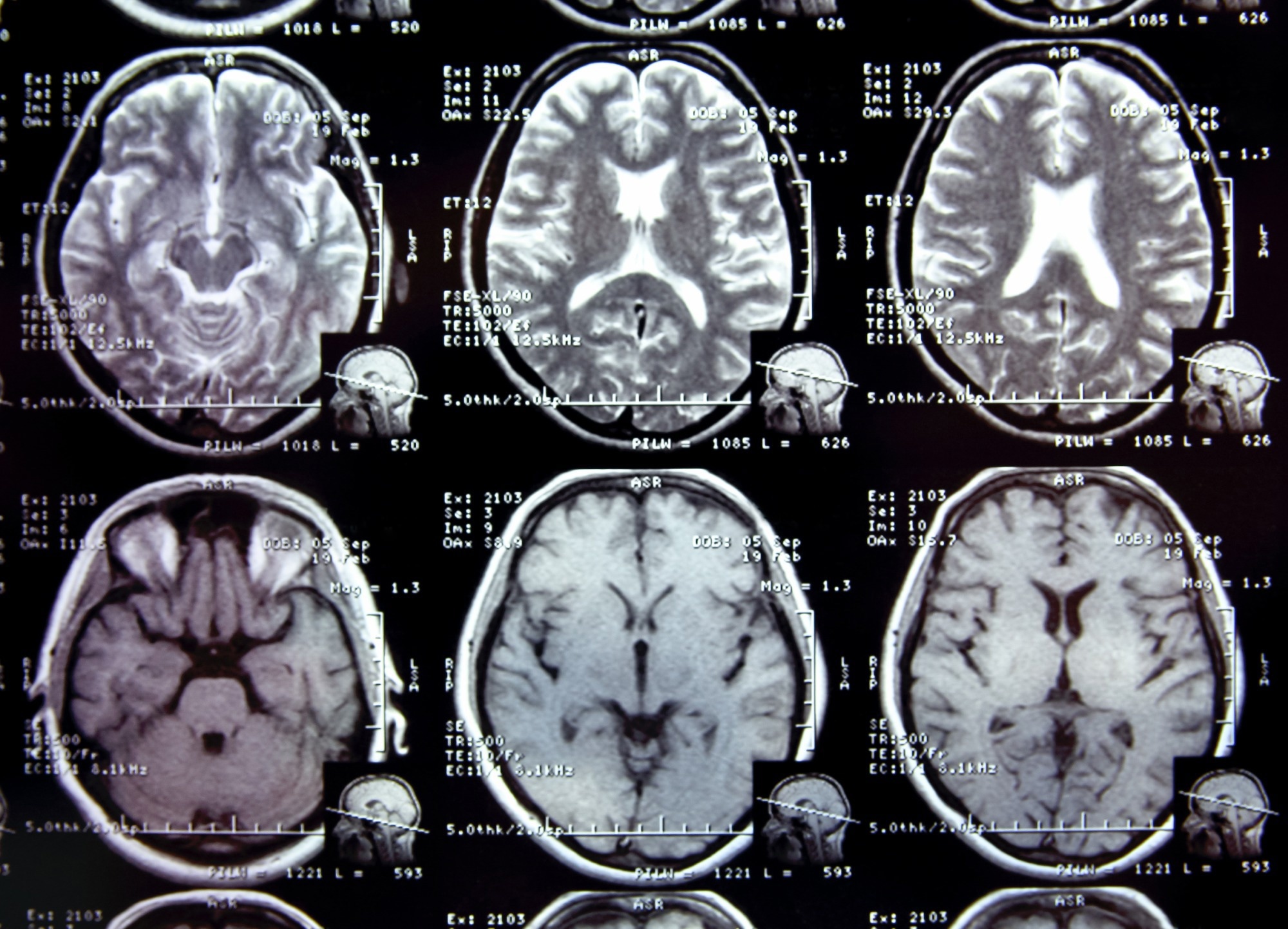
Study: COVID-19 and the impact on Alzheimer’s disease pathology. Image Credit: alexialex / Shutterstock.com
Background
COVID-19 primarily affects older individuals with medical disorders that compromise their immunity. The varied neurological manifestations of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection indicate that the virus could impact the brain in several ways.
Previous studies have reported that viral infections may result in neurodegeneration. Since COVID-19 and AD share risk factors and pathological characteristics, there have been significant public health concerns regarding the neurological impact of SARS-CoV-2 infection and its probable contribution to AD onset and progression through inflammation.
Pathogenesis and risk factors of AD and COVID-19
AD is characterized by increases in amyloid plaques, neurofibrillary tangles (NFTs), neuroinflammation, and neuronal loss. Extracellular amyloid plaques, which are predominant in the hippocampus and neocortex, develop due to amyloid beta (Aβ) peptide accumulation, which results from amyloidogenic processing and amyloid precursor protein (APP) cleavage by proteolytic enzymes such as beta- and gamma-secretase.
NFTs are abnormal filaments comprising misfolded and abnormally hyperphosphorylated tau proteins that accumulate in axons and dendrites and lead to neuronal loss. NFT accumulation occurs in the entorhinal cortex, CA1, and subiculum hippocampal regions. Aβ accumulation results in glial cell activation and inflammation.
Astrocytes are the most abundant glial cell type in the central nervous system (CNS). Upon activation, astrocytes and microglia secrete pro-inflammatory cytokines such as tissue necrosis factor-alpha (TNF-α), interferon-gamma (IFN-γ), interleukin-1 (IL-1), and IL-6. The release of these cytokines can induce neuronal damage and Aβ production, which is associated with elevated Aβ42/Aβ40 ratios, tau pathology, and neurotoxicity.
Risk factors for COVID-19 include age and certain comorbidities like diabetes, obesity, cardiovascular disease, and hypertension. Previous studies have indicated pre-existing dementia is a prominent risk factor for COVID-19 severity and mortality. Apolipoprotein E4 (APOE4), the strongest genetic risk factor for AD, can also enhance COVID-19 risk.
SARS-CoV-2 infections, neurodegeneration, and Alzheimer’s disease
Viral infections such as COVID-19 are associated with an increased risk of cognitive decline and neurodegenerative diseases. SARS-CoV-2 has amyloidogenic properties and can initiate amyloid aggregation. SARS-CoV-2 infection can increase Aβ42 protein neurotoxicity in brain cells, impair Aβ42 clearance from the blood, and enhance amyloid protein aggregation in the cerebrospinal fluid (CSF).
The presence of Aβ42 can enhance SARS-CoV-2 spike (S) protein-angiotensin-converting enzyme 2 (ACE2) interactions, thus facilitating entry into the host and stimulating the release of inflammatory cytokines like IL-1β and IL-6, which are linked to Aβ deposition and impaired neurogenesis in the hippocampus.
ACE2 elevation in AD murine models reduces Aβ42 accumulation in the hippocampus, reduces hyperphosphorylated tau protein and inflammatory cytokine levels in brain cells, and improves cognition. Therefore, ACE2 inhibition, which has been observed during SARS-CoV-2 infection, may worsen AD-related neuroinflammation and pathology.
ACE2 regulates brain-derived neurotrophic factor (BDNF) levels, essential for neurogenesis, cognition, and development. Reduced BDNF can increase tau protein phosphorylation, neuroinflammation, and neurodegeneration among SARS-CoV-2-infected individuals. Researchers have identified ACE2-expressing CNS cells such as microglia, neurons, astrocytes, and oligodendrocytes as probable interventional targets.
Experimental coronavirus infections in the CNS of mice have stimulated astrocytes and microglia related to pro-inflammatory cytokine and chemokine release that activate both the innate and adaptive immunological systems. SARS-CoV-2-induced microglial activation, partly regulated by the NLR family pyrin domain containing 3 (NLRP3) inflammasome, impairs Aβ protein clearance and increases neuroinflammation-related gene expression.
Post-mortem analysis of brains from SARS-CoV-2-infected individuals exhibits gliosis and immune cell accumulation associated with axonal injury and blood-brain barrier (BBB) disruption and, as a result, increased capillary permeability and endothelial damage. Elevated serological neurofilament light chain (NfL) and glial fibrillary acidic protein (GFAP) levels among moderate-to-severe COVID-19 patients indicate neuronal and astrocytic injury.
One year after severe COVID-19, reduced axonal density has been reported in the superior longitudinal fasciculus corpus callosum and corona radiata of the brain. Alterations in the olfactory cortical and limbic systems, including tissue injury and reduced gray matter thickness, have also been reported.
Conclusions
Overall, the study findings highlight the link between COVID-19 and AD, with SARS-CoV-2 infections linked to neuroinflammation, neurodegeneration, and long-term cognitive impairment. These findings indicate that both COVID-19 and AD have synergistic effects; however, further research is required to elucidate their long-term implications.