Infection
Understanding the Risk of Infection Associated With Neutrophils and Alcohol-Related Hepatitis
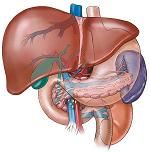
Alcohol-related hepatitis (AH) represents a significant health issue within the United States, resulting in thousands of hospitalizations a year. Presentation and severity of AH can vary from patient-to patient. The 30-day mortality rate is less than 5% in patients without encephalopathy, jaundice, or coagulopathy.1 However, the mortality rate increases significantly for inpatients. The 1-year mortality rate after hospitalization for AH is approximately 40%.1
Understanding the mechanisms for which this hepatitis impacts the body and in particular, the role of neutrophils, is critical to addressing the health burden.
AH is a major liver disease that causes significant morbidity and mortality, in addition to healthcare and economic burdens on a global scale. Causing an acute inflammatory form of alcohol-related liver disease, it has been noted to have short-term mortality and easily leading to deadly infections. Often associated with an increased number of neutrophils, researchers have worked to understand their role during AH and how the role of these infection-fighting white blood cells might be impacted.
A new study in the Journal of Hepatology sought to assess this relationship as patients with AH have high rates of mortality, including 20% at 4 weeks following prognosis and 30% at 90 days. The authors emphasized that mortality rates climb to 50% at a year and infections are the common cause as a result of AH, which is why there is a need to understand how the increased circulating neutrophil counts impact patient outcomes. As neutrophils can mount pretty potent antimicrobial responses, their activation during AH occurs at baseline, while exhibiting impaired phagocytotic and oxidative burst responses to pathogens like E coli, could have a negative impact on infection risk.2
The authors noted that, “Neutrophil recruitment and excess hepatic infiltration contributes to inflammatory injury in AH, and experimental strategies to limit neutrophil recruitment/infiltration are associated with reduced liver injury, although such findings are limited to animal models. Neutrophils are also important for timely resolution of tissue damage in AH, particularly through cross-talk with activated Kupffer cells. Thus, they act as a double-edged sword in AH.” 2
What You Need to Know
Alcohol-related hepatitis is a major liver disease that causes substantial morbidity and mortality, leading to a significant healthcare and economic burden, not only in the United States but on a global scale.
Neutrophils, a type of white blood cell responsible for fighting infections, play a critical role in AH. Patients with AH often exhibit an increased number of neutrophils.
Researchers are exploring the potential of targeted therapies to correct neutrophil dysfunction in AH. There is a focus on understanding the detailed transcriptional mechanisms of neutrophil dysfunction and the role of miR-223 in regulating the effects of neutrophils in liver disease.
In the face of the increased neutrophils (both circulating and hepatic) during AH, patients do experience an increased risk of infection due to the impaired function of the neutrophils.
Specifically, “Whilst increasing evidence suggests the importance of neutrophil miR-223 in beneficially regulating the effects of neutrophils in liver disease, this is again dysfunctional in patients with AH. Advances in our understanding of the detailed transcriptional mechanisms of neutrophil dysfunction in AH, and of neutrophil subsets in health and disease, will hopefully guide the development of targeted therapies to correct neutrophil dysfunction in AH.”2
To reduce mortality for severe cases of AH, corticosteroids are recommended despite short-lived benefits. However, therapeutic interventions using neutrophils are unlikely to involve simple strategies to promote or inhibit neutrophil mobilization from the bone marrow but rather may need to manipulate key functions within tissue.” 2
Ultimately, the authors stressed the need for additional research and the potential benefits of correcting gut dysbiosis to help avoid excessive neutrophil activation while also enhancing miR-223 function during AH.
References
1. Alcoholic Hepatitis. Medscape. Updated September 19, 2019. Accessed October 24, 2023. https://emedicine.medscape.com/article/170539-overview?form=fpf
2.Khan RS, Lalor PF, Thursz M, Newsome PN. The role of neutrophils in alcohol-related hepatitis. J Hepatol. 2023;79(4):1037-1048. doi:10.1016/j.jhep.2023.05.017