Health Care, Infection, Insight, Medical Care
What Is Pneumonia?
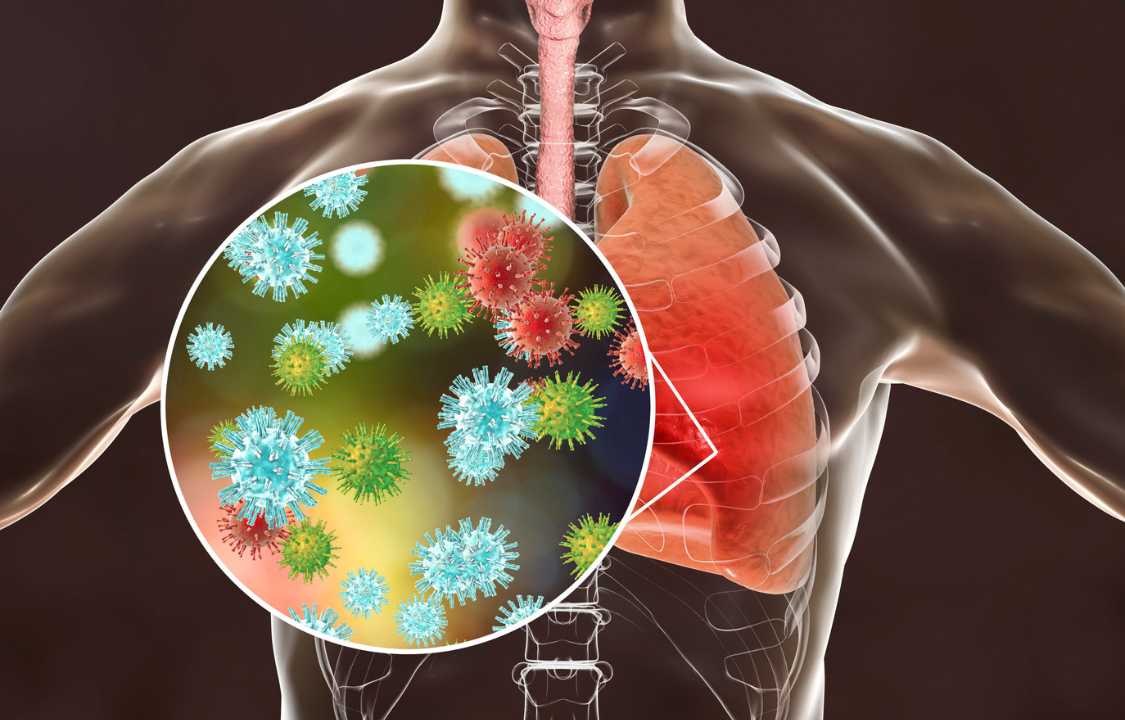
Pneumonia, a prevalent lung infection, encompasses a spectrum of diseases triggered by bacterial, viral, and fungal agents. This multifaceted ailment manifests as the infiltration of air sacs within the lungs with fluid or pus, leading to a wide range of symptoms, which can vary from mild to life-threatening. These symptoms encompass shortness of breath, cough, fever, chest pain, and fatigue. Accurate diagnosis necessitates a combination of physical examinations and laboratory and imaging tests. The choice of treatment hinges on the underlying cause of pneumonia and the severity of symptoms.
Pneumonia is not restricted by age, although certain populations, such as children, older adults, and individuals with weakened immune systems, are at higher risk. Disturbingly, in the United States, pneumonia casts a substantial healthcare burden, with over 120 million children under the age of 5 diagnosed with pneumonia annually, and approximately 1.5 million adults requiring hospital care for pneumonia each year.
The Diverse Types of Pneumonia
Pneumonia exhibits its diversity through classification based on the causative pathogen (germ). Broadly, pneumonia types include:
1. Bacterial Pneumonia: Numerous bacterial species can incite pneumonia, with Streptococcus pneumoniae emerging as the predominant bacterial agent associated with pneumonia in the U.S.
2. Viral Pneumonia: Viruses targeting the respiratory tract, such as influenza and respiratory syncytial virus (RSV), can instigate pneumonia.
3. Fungal Pneumonia: Fungi, exemplified by pneumocystis pneumonia (PCP), can provoke pneumonia, especially in individuals with chronic health conditions and weakened immune systems.
4. Walking Pneumonia: Mycoplasma pneumoniae bacteria give rise to this form of pneumonia, which typically allows individuals to continue their daily routines due to its mild nature.
5. Aspiration Pneumonia: This condition arises when mouth secretions, stomach contents, or food are inadvertently inhaled into the lungs instead of being swallowed.
Healthcare providers also categorize pneumonia based on the location of infection acquisition:
1. Community-Acquired Pneumonia: This occurs outside of healthcare facilities, often resulting from bacterial, viral, or fungal infections.
2. Hospital-Acquired Pneumonia: Contracted during hospitalization, it poses a higher degree of severity because hospital-acquired germs are often more resilient to treatment.
Deciphering Pneumonia Symptoms
The symptoms of pneumonia span a broad spectrum of severity, with greater risks of severe symptoms and complications among young children, older adults, and immunocompromised individuals. Common pneumonia symptoms include:
- Cough, with or without mucus
- Chest pain or tightness, intensified during coughing or deep breaths
- Fever
- Chills
- Shortness of breath
- Fatigue
- Loss of appetite
Less common symptoms encompass headache, muscle aches, extreme fatigue, nausea, vomiting, and diarrhea. Older adults and individuals with compromised immune systems may exhibit atypical symptoms, including a low body temperature rather than fever, along with abrupt changes in mental awareness and confusion.
Infants and young children with pneumonia may display additional symptoms, such as bluish-colored skin and lips, rapid breathing, grunting, widened nostrils, inward pulling of rib muscles during breathing, and irritability.
Pneumonia’s Etiology
Pneumonia typically stems from pathogens like bacteria, viruses, and fungi. This condition can also manifest when liquids or food are inhaled, rather than being swallowed. As the immune system wages a battle against these germs, the lungs become inflamed, causing fluid or pus to accumulate within the tiny air sacs, known as alveoli.
Among the bacterial causes of pneumonia, Streptococcus pneumoniae is the most common in the United States. Conversely, viruses targeting the respiratory tract, such as influenza, respiratory syncytial virus (RSV), and the common cold, rank as the primary culprits behind viral pneumonia. Fungi, exemplified by Pneumocystis jirovecii, can trigger pneumonia, particularly in immunocompromised individuals.
Unearthing Risk Factors
Pneumonia’s onset can affect anyone, but certain risk factors elevate one’s susceptibility to this condition:
1. Age: Both infants and children under two and older adults aged 65 and above face a higher vulnerability to pneumonia.
2. Environment: Inhabitants of crowded places like homeless shelters, prisons, nursing homes, or dormitories are at an increased risk.
3. Occupation: People exposed to chemical fumes, dust, or animal environments (e.g., meat processing centers, veterinary clinics) face elevated risks.
4. Weakened Immune System: Immunocompromised individuals, such as those with HIV/AIDS or undergoing chemotherapy, have a heightened likelihood of pneumonia.
5. Hospitalization: Hospital care, especially in cases of sedation, unconsciousness, immobility, or ventilator use, can elevate the risk of hospital-acquired pneumonia.
6. Smoking: The cumulative damage inflicted by smoking on the lungs amplifies the pneumonia risk over time.
7. Other Medical Conditions: Lung diseases and medical conditions affecting coughing or swallowing can heighten pneumonia risk.
Pneumonia Diagnosis: A Complex Endeavor
Diagnosing pneumonia can prove intricate, given its symptom overlap with influenza and the common cold. Healthcare providers employ a multifaceted approach, inquiring about medical history, symptoms, travel history, and exposure to illness and animals. A physical examination, including lung auscultation with a stethoscope, is conducted.
To confirm a pneumonia diagnosis, diagnostic tests are often ordered, including:
- Chest X-ray: This procedure captures images of the lungs, unveiling signs of inflammation or fluid accumulation.
- Blood Tests: These ascertain the presence of infection and identify the specific pathogen responsible for pneumonia.
- Pulse Oximetry: It gauges oxygen levels in the blood, which may decrease during pneumonia.
- Sputum Culture: This test analyzes a mucus sample from the lungs, aiding in identifying the causative pathogen.
In cases of heightened risk for pneumonia complications or hospitalization, additional tests like computed tomography (CT) scans, bronchoscopy, arterial blood gas analysis, and pleural fluid culture may be employed.
Treatment Modalities
Treatment for pneumonia is predicated on symptom severity, the underlying cause, and the patient’s overall health. Medications assume a pivotal role in treatment:
- Antibiotics: These are prescribed for bacterial pneumonia, and patients often experience symptom improvement within days. Completing the full antibiotic course is essential to prevent reinfection.
- Antiviral Medications: Viral pneumonia can be treated with antiviral drugs when applicable. However, these drugs may not be effective against all viruses, and rest and symptom management may be recommended.
- Antifungal Medicines: Fungal pneumonia calls for antifungal drugs.
- Over-the-Counter Pain Relievers: Medications like Tylenol (acetaminophen) and Advil (ibuprofen) can alleviate pain, discomfort, and fever.
For those with mild pneumonia, management at home is typically feasible. Rest, hydration, warm beverages, hot showers or baths, and the use of humidifiers can help ease symptoms. Avoiding lung irritants like cigarette smoke, chemicals, wood smoke, and allergens during the recovery period is essential.
Severe cases of pneumonia, or those with complications, may necessitate hospitalization. Hospital-based treatments can encompass oxygen therapy, intravenous fluids and medications, mechanical ventilation, and, in extreme cases, surgery to remove infected lung tissue.
Preventing Pneumonia: A Proactive Approach
Preventing pneumonia is achievable through a proactive stance on health and hygiene:
- Vaccination: Vaccines targeting common pneumonia-causing pathogens, such as influenza, COVID-19, and pneumococcus bacteria, play a pivotal role in reducing the risk of certain pneumonia types and complications.
- Good Hygiene: Regular handwashing with soap and water and refraining from face touching in public spaces can mitigate germ transmission.
- Smoking Cessation: Abandoning smoking is crucial, as it not only damages the lungs but also weakens the immune system, rendering infections harder to combat.
- Healthy Lifestyle: Maintaining a balanced diet, engaging in regular exercise, and ensuring sufficient sleep bolster the immune system.
- Managing Chronic Conditions: Adhering to treatment plans for chronic conditions such as heart disease, diabetes, or COPD reduces pneumonia risk.
Managing Comorbid Conditions
Certain health conditions increase the susceptibility to pneumonia and its associated complications. These comorbid conditions encompass obesity, diabetes, high blood pressure, cardiovascular disease, chronic obstructive pulmonary disease (COPD), alcohol use disorder, and malnutrition.
Living with Pneumonia: Recovery and Beyond
Upon exhibiting pneumonia symptoms, seeking prompt medical attention is paramount. Early diagnosis and treatment can avert complications and expedite recovery. Complementing treatment plans with adequate rest and hydration is crucial to a full recovery, which may take several weeks.
Follow-up care with healthcare providers is essential, especially if symptoms persist or worsen. Physical therapy and pulmonary rehabilitation may be recommended to regain strength and lung function. Additionally, adopting a healthier lifestyle by quitting smoking, staying up-to-date on vaccinations, and managing chronic conditions diminishes the risk of future infections and enhances overall well-being.
In summary, pneumonia is a complex respiratory ailment with diverse causes, symptoms, diagnostic approaches, and treatment modalities. Prevention through vaccination, hygiene, lifestyle choices, and the management of underlying conditions plays a pivotal role in reducing pneumonia risk. Timely diagnosis, adherence to treatment, and post-recovery care are crucial steps in the journey to combat this common lung infection effectively.