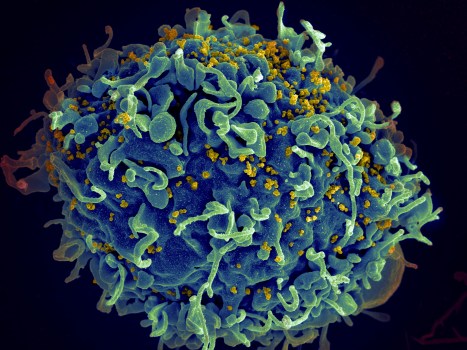
Infection
CRISPR gene editing could kill HIV. But is it a cure?
In a provocative first step toward an elusive end to a devastating disease that has claimed 40 million lives, three patients have received CRISPR gene-editing therapies in an effort to eradicate HIV from their bodies.
The results — whether the men are cured or not after the one-time intravenous infusions this year — have not yet been disclosed by the San Francisco biotech company that created the technology based on Nobel Prize-winning research by UC Berkeley’s Jennifer Doudna.
But the potential treatment, called EBT-101, is safe and caused no major side effects, Excision BioTherapeutics reported at a meeting in Brussels this week.
Six more men will be treated, perhaps some at UC San Francisco, with higher doses. Participating in the research program is potentially risky: Participants stop their protective anti-HIV drugs for 12 weeks after gene-editing treatment to see if the virus is gone. Data will be presented at a medical conference next year, according to the company.
“We are opening the door for how this new drug will work and what potential it has for people living with HIV,” said Dr. William Kennedy, Excision senior vice president of clinical development. “Ultimately, we see this as a fundamentally new approach.”
The novel strategy could potentially treat other chronic infections where the virus hides latent, such as hepatitis and herpes, he said. It leaves human DNA intact.
“We were super excited about this, and to get the chance to be among the first to do human studies of gene editing for a cure,” said Dr. Priscilla Hsue, professor of medicine and principal investigator for the study’s clinical trial site at UCSF. “If we can permanently remove viral DNA, the thought is, people would get this infusion and then be done.”
EBT-101 is designed to find the specific viral sequences so that it doesn’t cut human DNA. The CRISPR-based therapy uses an empty virus to deliver the “guide RNA” that marks where to cut. An enzyme called Cas9 acts like scissors. The therapeutic solution is given intravenously.
It received the FDA’s “fast track” designation last July after experiments showed success in animals. A single injection safely and efficiently removed SIV, a virus related to HIV, from the genomes of rhesus monkeys. In earlier work, it removed HIV from nine of 23 mice.
But there is a big leap from promising results in mice to success in humans. In addition to UCSF, patients will be recruited at Quest Clinical Research in San Francisco, Washington University in St. Louis and Cooper University in Camden, New Jersey.
In the four decades since the AIDS virus was isolated, treatment has transformed its care. If taken every day, powerful antiretroviral drugs can suppress the virus, controlling illness. Medicine can also prevent infection.
But a cure is needed to end the pandemic. Worldwide, nearly 39 million people are living with HIV. About 77% of them are receiving treatment.
There have only been three known cases of an HIV cure so far. Two were men who received bone marrow transplants from donors who carried a mutation that blocks HIV infection. The third was a woman who received a transplant of umbilical cord blood. But all three treatments were targeting cancer, so this is not a practical option for the average HIV patient.
“The future of so many lives depends on another breakthrough,” said Mark King, an Atlanta-based HIV/AIDS activist and author of the book My Fabulous Disease who has lived with the virus for nearly 40 years.
“A lot of people think that this was all rectified when we got successful treatments,” he said. “But the difference between a treatment and a cure, or a vaccine, is profound.”
Excision BioTherapeutics was founded on work in the lab of Kamel Khalili, a professor at Temple University in Philadelphia and director of its Center for NeuroVirology and Gene Editing.
Its research is supported, in part, by the taxpayer-supported California Institute of Regenerative Medicine. The early results of its study were presented at the European Society of Gene and Cell Therapy on Wednesday.
CRISPR gene editing, an ingenious system discovered by Jennifer Doudna, a biologist with UC-Berkeley’s Innovative Genomics Institute, can cure genetic disease by using little molecular scissors to cut out a piece of a person’s DNA. It is now being used to treat several diseases, such as sickle cell anemia, nerve disease and congenital blindness.
Scientists wondered: Could CRISPR cure HIV by cutting the virus’s DNA? Excision’s approach cuts the virus in two places, removing genes that are essential to replication.
“This is an exceptionally ambitious and important trial,” said Fyodor Urnov, professor of molecular and cell biology at UC-Berkeley and a gene editor at IGI, in an email. “It would be good to know sooner than later” if it works, he said, “including, potentially, no effect.”
Initial research in Khalili’s lab showed that CRISPR could find and destroy the HIV genes in cells.
The results were welcomed with caution by long-term survivors such as King. “Am I intrigued? Yes. Wary? Absolutely. We have been here before, many times. We’ve heard of a lot of promising developments over the years, only to have the rug pulled out from us — because of the vexing nature of how HIV operates in the body.”
The reason that HIV has been so tough to eradicate is that it hides in our cells, said Dr. Jyoti Gupta of the PACE Clinic at Santa Clara Valley Medical Center, which specializes in HIV care.
“The virus is very smart,” she said. “It integrates into the host genome of our immune cells, which are supposed to protect us from infection. It just lies there, hiding.”
“As soon as someone stops the therapy, the latent virus starts replicating again, within days,” said Gupta. “Then there’s virus everywhere.”
Patients in Excision’s trials will be monitored for 15 years, said Kennedy.
Even if it just stops replication for awhile, that’s a benefit, said Gupta. “Less is more. So if a patient can come in for an infusion once a year, for instance, and the virus won’t resurface for a year, that’s reasonable.”
The hope is that Excision’s therapy could become a lifelong cure, freeing patients from daily pill-popping
“Scientists tell me that this is going to be part of a cure some day,” said Berkeley-based AIDS activist Matt Sharp, 68, who has lived with the virus for 38 years. “And I shrug my shoulders and say, ‘Here we go again.’ ”
“Now we just have to get the research done,” he said. “We’ve got to have hope, because the epidemic isn’t over.”