Cardiovascular
Cardiovascular and VTE Risk With JAK Inhibitors in Immune-Mediated Inflammatory Skin Diseases
Key Points
Question
Are Janus kinase (JAK) inhibitors associated with higher risk of all-cause mortality, major adverse cardiovascular events (MACE), and venous thromboembolism (VTE) when used for a dermatologic indication?
Findings
In this systematic review and meta-analysis of 35 randomized clinical trials containing over 20 000 patients with dermatologic conditions, no significant difference was found between JAK inhibitors and placebo/active comparator in composite MACE and all-cause mortality or VTE.
Meaning
Short-term (<5 months) use of JAK inhibitors for a dermatologic indication likely is not associated with an increased risk of all-cause mortality, MACE, and VTE.
Importance
Janus kinase (JAK) inhibitors are an effective treatment option for patients with certain skin-related conditions, such as atopic dermatitis, alopecia areata, and vitiligo, but there is a current US Food and Drug Administration (FDA) boxed warning label for oral and topical JAK inhibitors regarding increased risk of major adverse cardiovascular events (MACE), venous thromboembolism (VTE), serious infections, malignant neoplasm, and death. However, this boxed warning was precipitated by results of the Oral Rheumatoid Arthritis Trial (ORAL) Surveillance study, which only included patients with rheumatoid arthritis, and the same association may not be observed in dermatologic conditions.
Objective
To determine the risk of all-cause mortality, MACE, and VTE with JAK inhibitors in patients with dermatologic conditions.
Data Sources
PubMed and ClinicalTrials.gov were searched from database inception to April 1, 2023.
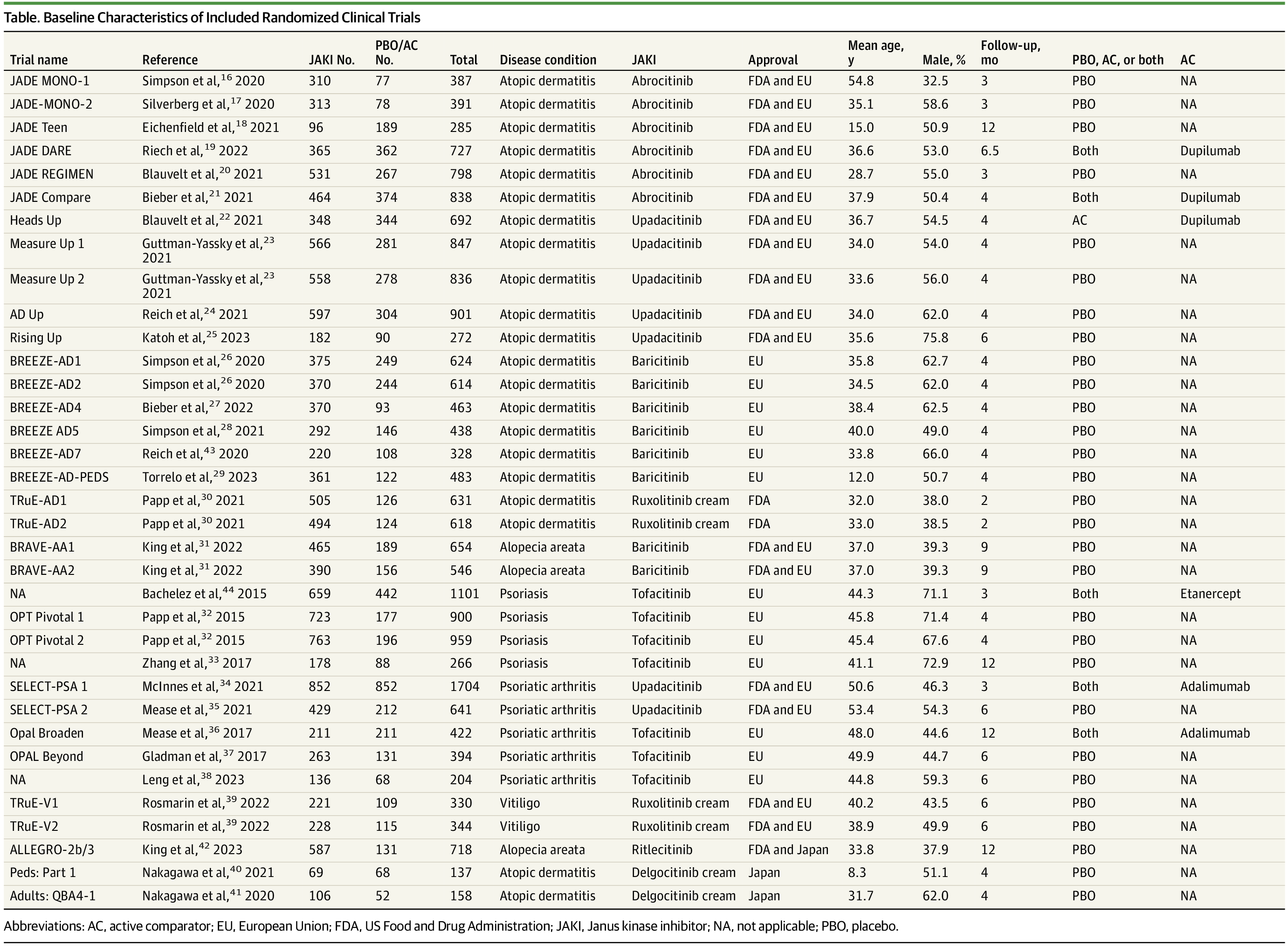
Study Selection
This review included phase 3 randomized clinical trials with a placebo/active comparator group of JAK inhibitors used for a dermatologic indication with FDA approval or pending approval or with European Union or Japanese approval. Studies without a comparison group, case reports, observational studies, and review articles were excluded.
Data Extraction and Synthesis
This study was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines. Adverse events using odds ratios (ORs) and 95% CIs were calculated using a random-effects model and the DerSimonian-Laird method. Studies were screened, data abstracted, and quality assessed by 2 independent authors. The protocol was prospectively registered with PROSPERO.
Main Outcomes and Measures
Primary outcomes were a composite of adjudicated MACE and all-cause mortality, and VTE.
Results
The analysis included 35 randomized clinical trials with 20 651 patients (mean [SD] age, 38.5 [10.1] years; male, 54%) and a mean (SD) follow-up time of 4.9 (2.68) months. Findings did not show a significant difference between JAK inhibitors and placebo/active comparator in composite MACE and all-cause mortality (OR, 0.83; 95% CI, 0.44-1.57) or VTE (OR, 0.52; 95% CI, 0.26-1.04).
Conclusions and Relevance
In this systematic review and meta-analysis, use of JAK inhibitors was not associated with increased risk of all-cause mortality, MACE, and VTE compared to the placebo/active comparator groups. Additional trials with long-term follow-up are needed to better understand the safety risks of JAK inhibitors used for dermatologic indications.