Cardiovascular
Impact of cardiac rehabilitation on cardiovascular event in Korea
Abstract
This study aimed to evaluate the effects of cardiac rehabilitation (CR) on major adverse cardiac events (MACE) among patients who underwent PCI procedure. We used data from the electronic medical records (EMR) of a tertiary hospital in Seoul, Korea, from January 2014 to February 2020. Data from 2988 patients who had experienced their first acute coronary syndrome (ACS) and had undergone percutaneous coronary intervention (PCI) were included during the study period. we classified patients into CR participants and non-participants based on their participation in the cardiac rehabilitation (CR) program within 30 days after discharge. And the outcome was the incidence of myocardial infarction (MI) and stroke within 1 year after discharge. The association between participation in CR and risk of developing MACE was evaluated using the Cox proportional hazards model. Patients who achieved CR after undergoing PCI were at a lower risk of developing MI (HR 0.68, CI 0.53–0.86). There was no significant association between participation in CR and the incidence of stroke. Among patients who had more than three stenotic vessels, the risk of developing MI within 1 year of discharge was reduced in CR users compared to non-users (3 or more stenosis vessels: HR 0.55, CI 0.35–0.86). Among patients who used two and more stents during PCI procedures, the risk of developing MI within 1 year of discharge was reduced in CR users compared to non-users (2 and more stents: HR 0.54, CI 0.35–0.85). Among people diagnosed with ACS and receiving PCI, patients who participated in CR within one month of discharge reduced risk of developing MI. Our study reinforced the current evidence on the effect of CR among patients receiving PCI and presented the expansion and enhancement of the CR program.
Introduction
Heart disease is a major cause of premature mortality and an important cause of disability globally1,2. In Korea, heart disease is the second major cause of death. Ischemic heart disease, which accounts for approximately half of the deaths from all heart diseases, increased from 12,893 in 2009 to 13,699 in 20193. According to the World Heart Federation, the global cost of cardiovascular disease (CVD) in 2010 was approximately US $863 billion, which is expected to rise to more than US $1 trillion by 20304.
Most treatments for severe heart disease involve cardiac surgery or medication. Postoperative complications include pulmonary complications, delirium, and arrhythmias5,6,7. Furthermore, restenosis of heart disease occurs in approximately 30–50% of patients undergoing percutaneous coronary intervention8. These complications are linked to a long period of hospitalization, increased adverse events, and higher healthcare costs9,10,11,12.
To minimize and prevent the possibility of disease recurrence after percutaneous coronary intervention, the 2011 American Heart Association recommends participation in pre-discharge cardiac rehabilitation (CR) at the Class I level and published the relevant guideline13. The goal of CR is to improve the preoperative and postoperative status of patients undergoing CVD14. CR is a program designed to minimize recurrence and related complications of CVD through proper medication, improvement of lifestyle for diabetes, high blood pressure, hyperlipidemia, exercise, diet, smoking cessation, and stress15.
Previous studies have shown that CR programs for coronary artery disease patients have reduced mortality and increased survival rates through exercise, diet, smoking cessation, weight control, diabetes, and hypertension management16,17,18. As the effectiveness of CR was proven, the demand for heart rehabilitation increased. The problem of economic burden, which was one of the factors for underutilizing of CR, was resolved when CR services after IHD started being reimbursed as medical treatment benefits since February 2017. Currently, 111 countries worldwide have implemented CR19.
In Korea, few studies have evaluated the effectiveness of CR using clinical data, and few studies have considered the duration of the event. This study aimed to evaluate the effects of CR on major adverse cardiac events (MACE) caused by myocardial infarction, stroke for 1 year after discharge, using patient data from a tertiary hospital in Seoul. We hypothesize that CR is necessary to prevent recurrence and deterioration of patients with coronary artery disease.
Method
Data
We used data from the electronic medical records (EMR) of a tertiary hospital in Seoul, Korea, from January 2014 to February 2020. The EMR included clinical information of eligible patients, such as demographics, past medical history, vital signs, laboratory findings, diagnosis of acute coronary syndrome (ACS), level of education, performance status, surgery type, and procedure of surgery. The data was encrypted to safeguard personal information.
Participants
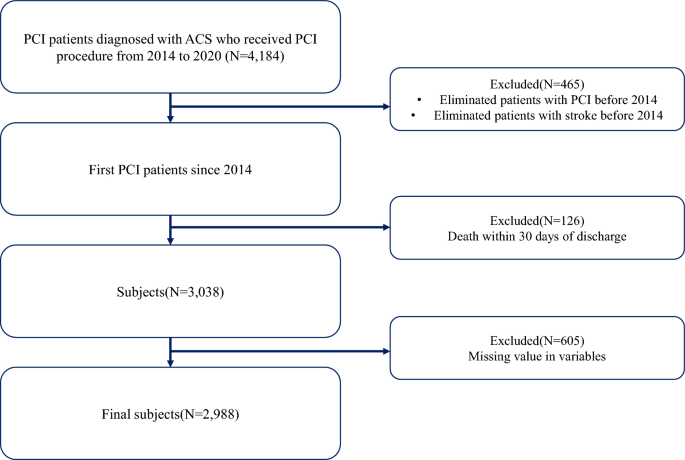
We extracted individuals who had diagnosed acute coronary syndrome (ACS) and undergone PCI procedures from January 2014 to February 2020. Consequently, those who had received PCI procedures before 2014 were excluded, and individuals diagnosed with stroke before 2014 were also excluded to create a homogeneous population. Additionally, individuals covered by medical aid program were excluded due to different healthcare systems in South Korea, and only those with national health insurance were included. Furthermore, individuals who died within 30 days after discharge were also excluded (Fig. 1). Finally, we extracted data pertaining to 2988 patients.
Flow chart of the study.
Utilization of Cardiac rehabilitation
In this study, individuals who engaged in the cardiac rehabilitation (CR) program within 30 days of their discharge following PCI were categorized as CR participants. The CR program comprised three components: education, exercise, and evaluation, and patients’ involvement in any of these aspects was identified by fee codes. However, there was no patients who participated in evaluation program. CR utilization was characterized as a patient’s involvement in one or more of the CR program elements (education, exercise, both) during the initial 30 days following their PCI discharge.
Outcome
The outcome was the incidence of major adverse cardiovascular event (MACE) within 1 year after discharge. Many studies have used MACE for evaluating the effect of CR as an indicator of one result rather than measuring the effect for each result20,21. In our study, MACE is defined as the incidence of myocardial infarction (MI), stroke which are important prognostic factors that may appear in heart disease patients as major heart events. These are indicators commonly identified in various studies to confirm the effect of CR22. We identified participants with a diagnosis of myocardial infarction (MI) using ICD-10 codes I21, I22, I23, I25.2, and I25.5, as well as those with a diagnosis of stroke using codes I60 through I69. The occurrence of MACE after discharge of the study subjects was monitored for 1 year using diagnosis codes and EMR. Patients who were re-hospitalized under the code name of MI and stroke within 1 year were identified by follow-up observation based on the date of initial discharge.
Variables
We controlled for covariates, such as sociodemographic, socioeconomic, health information, and clinical factors. Sociodemographic factors included sex (male and female), age (less than 60, 60–69, and over 70 years), and education level (elementary or middle school, high school). Socioeconomic factors included difficulty paying medical bills (yes or no). Health information factors included smoking status (current, ex, non), BMI (< 25, ≥ 25), regular exercise (yes or no), and past medical history (hypertension, dyslipidemia, cancer, chronic kidney disease). We considered the five clinical factors; When a patient was initially diagnosed with their first ACS, the diagnosis was categorized as unstable angina (UA, I20.0, I24.0), which was identified by ICD-10 codes, and this was classified separately from MI (I21, I22, I23, I25.2, I25.5). and we divided into individuals based on their use of stents during PCI procedures, categorizing them as “stent operators” if they used stents at least once and as “ballooning operators” if they exclusively performed ballooning procedures. Additionally, a small number of cases involving percutaneous thrombectomy and embolectomy were included in the ballooning procedure category. The corresponding ICD-10 codes were included in the supplementary table. We also included the number of vascular stenosis (1, 2, or 3 or more), the number of stent (0, 1, 2 or more) and target vessel of PCI procedure(left main or left anterior descending artery, others) during PCI procedure according to procedure of surgery note. We intend to use the number of stenosis vessel, stent and target vessel as proxy indicators for severity of health status.
Statistical analysis
The chi-squared test was used to determine the significant differences in variables between participants who died and those who did not. Statistical significance was set at P-value < 0.05. A Cox proportional hazards model was used to evaluate the association between participation in CR and incidence of MACE. The results were reported using hazard ratios (HRs) and 95% confidence intervals (CIs) for the risk of MACE. Each patient’s index date was the discharge date after the first PCI during the study period. And discharge dates and admission dates only include the year and month. Therefore, we assumed an arbitrary day to be the 1st of the month in our dataset. Additionally, the incidence of the event was analyzed by monitoring the index data for 6 months, 2 years, and 3 years. The data were analyzed using SAS 9.4 (SAS Institute Inc; Cary, North Carolina).
Ethics declarations
The Institutional Review Board of Yonsei University Health System approved this study (approval number: 4-2022-0452) and waived the requirement for informed consent as The Korean Vital Statistics database consists of anonymized, and unidentified patient data. And the study was conducted according to the tenets of the 2013 Declaration of Helsinki.
Ethical approval
The requirement for informed consent was waived by Yonsei University Health System institutional review board (4–2022-0452) as The Korean Vital Statistics database consists of anonymized, and unidentified patient data. We assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Results
Table 1 presents the general characteristics of the baseline study participants. A total of 2988 participants were diagnosed ACS and undergone PCI procedures during study period. Among the patients who underwent PCI, 339 (11.3%) had incident MI within 1 year of discharge, 31 (1%) developed stroke within 1 year of dischrge. Out of 2988 participants, 1156 (38.7%) participated in the CR program within 30 days after discharge.
Figure 2 presents the Kaplan–Meier survival curves comparing the incidence of MI and stroke between CR users and non-users. Vertical lines indicate the non-incidence probability of MI and stroke, and horizontal lines indicate the monitoring days. Patients who participated in CR less frequently developed MI and stroke (MI: p < 0.0001, Stroke: p < 0.2982).

Kaplan–Meier survival curves for participants in cardiac rehabilitation in 1-year occurrence of readmission for MI and stroke.
Table 2 reports the findings of Cox proportional hazards regression analysis regarding the association between participation in CR and incidence of MI and stroke after adjusting for the abovementioned covariates. Patients who utilized CR after undergoing PCI were at lower risk of developing MI (HR 0.68, CI 0.53–0.86) compared to CR non-user, and there was no significant association between participation in CR and incidence of stroke (HR 0.74, CI 0.33–1.70).
Subgroup analysis was conducted to evaluate the effect of participation in CR and the characteristics of the clinical procedure on the risk of developing MI and stroke (Table3). Among patients with UA, the risk of MI within 1 year of discharge was lower in CR users than in non-users (HR 0.56, CI 0.39–0.79). Among patients who had more than three stenotic vessels, the risk of developing MI within 1 year of discharge was reduced in CR users compared to non-users (3 or more stenosis vessels: HR 0.55, CI 0.35–0.86). Among patients who used two and more stents during PCI procedures, the risk of developing MI within 1 year of discharge was reduced in CR users compared to non-users (2 and more stents: HR 0.54, CI 0.35–0.85).
Table 4 shows the result of the association between participation in type of CR and incidence of MI and stroke. Patients who participated in the education program in CR had a lower risk of developing MI (HR 0.42, CI 0.31–0.59), and patients who participated in both the education and exercise programs in CR had a reduced risk of MI (HR 0.42, CI 0.27–0.65).
Discussion
In this study, we investigated the association between participation in CR and the incidence of MI and stroke among people diagnosed with ACS and receiving PCI. Few studies have investigated the effectiveness of CR using detailed clinical data on PCI procedures after the patients’ first ACS diagnosis. Participation in CR among patients who underwent a PCI procedure reduced the risk of developing MI within 1 year after discharge, but it was not associated with an increased risk of developing stroke. Also, participation in CR reduced risk of developing MI to a greater extent in patients who have multiple stenotic vessels and numerous stents.
Our results showed that patients who participated in CR within a month of discharge had a 32% lower probability of developing MI than those who did not. Previous studies have demonstrated the association between utilizing CR and MACE, which are generally in similar result to our study23,24,25,26. However, our study could not find evidence that participation in CR reduced the risk of stroke. In the Kaplan–Meier survival curve, there were significant differences between CR users and non-users by log-rank test. However, when we adjusted the covariates, there was no significant difference between CR users and non-users. Other studies have demonstrated an association between participation in cardiac rehabilitation (CR) and a reduced risk of stroke. These studies included participants with a prior history of stroke occurring before ACS events and adjusted their analyses accordingly. In contrast, our study adopted a different approach by excluding individuals with a history of stroke. This deliberate design choice introduces a potential divergence in results between our study and those that encompassed stroke history, warranting consideration when interpreting the findings27,28.
In our study, there was no significant difference in the risk of developing MI within 1 year after discharge among individuals diagnosed with UA or MI who underwent PCI procedures. However, participation in CR among UA patients significantly reduced the risk of MI occurrence within 1 year after discharge. However, participation in CR among MI patients was not associated with the risk of MI occurrence within 1 year after discharge. When individuals were diagnosed with ACS and underwent PCI, a higher number of stenosis vessels was associated with an increased risk of MI occurrence within 1 year after discharge. However, among patients with a higher number of stenosis vessels at the time of PCI, participation in cardiac rehabilitation within one month of discharge was associated with a significant reduction in the risk of MI occurrence within 1 year after discharge. Few studies have evaluated the effectiveness of CR in relation to the severity of patients with heart disease. Ejection fraction (EF) is the most important parameter in evaluating the severity of heart disease, and studies have shown that there is no association between heart rehabilitation and death or other events in patients with heart failure with reduced ejection fraction (HFrEF) or severely reduced EF29,30,31. However, there are still ongoing discussions about eligible participants of CR, and first-class recommendations target people with less than 35–40% EF32. In our study, due to data limitations, we were unable to ascertain the level of EF. However, we were able to assess the characteristics of patients’ ACS, which may provide a basis for determining eligibility for participation in CR.
In recent studies, the effects of cardiac rehabilitation have been studied based on the patients’ conditions, including obesity, hospital-acquired functional impairment, multimorbidity, and more. Among patients who participated in cardiac rehabilitation, patients with higher lean body mass (LBM) and body mass index (BMI) showed an increased risk of major adverse cardiovascular events (MACE), especially in the presence of multimorbidity33,34. Additionally, in the group of patients who experienced post-surgical hospital-acquired functional decline, participation in cardiac rehabilitation present that reducing the risk of MACE34. Our study examined the effectiveness of cardiac rehabilitation based on the disease status of patients at the time of PCI procedure, providing valuable insights into its impact on patient outcomes. Patients exhibiting diverse health conditions might be considered for personalized therapeutic approaches within cardiac rehabilitation.
In Korea, the government has established and operated a policy to strengthen health insurance coverage since 2005 to mitigate the economic burden of serious diseases (cancer, heart disease, cerebrovascular disease) for reducing out-of-pocket expenditure and converting benefits for non-benefit items. The CR program in Korea has been covered by the National Health Insurance since February 2017. The CR participation rate among cardiac patients in Korea ranged from 0.0 to 6.4% and was also low in hospitals actively delivering CR (14–35%)35,36. Because we studied data from an institution that is one of the largest providers of CR in Korea, the participation rate in CR was 38.7% in our study. Worldwide, only 38.8% of countries have CR programs19,37,38. Despite these benefits and recommendations in clinical practice guidelines, CR was grossly underused compared with other medical treatments for patients with CVD. Various studies and service providing systems are needed to promote CR.
This study has a few limitations. First, it was a retrospective study performed in a single-tertiary university hospital, lacking external validity. However, our study has the strengths of including a patient group with a history of ARS that is a high-risk group for MACE, having detailed long-term follow-up surveillance data, and analyzing detailed PCI procedures and status of ACS, which are related to the incidence of MACE. This can strengthen the accuracy of our findings. However, further studies with larger sample sizes, longer follow-up periods, and more events are needed to validate our findings.
Conclusions
Among people diagnosed with ACS and receiving PCI, patients who participated in CR within one month of discharge reduced risk of developing MI. Our study reinforced the current evidence on the effect of CR among patients receiving PCI and presented the expansion and enhancement of the CR program.
Data availability
The data that support the findings of this study are available on request from the corresponding author.
References
-
Tsao, C. W. et al. Heart disease and stroke statistics—2022 update: A report from the American Heart Association. Circulation 145, e153–e639 (2022).
Google Scholar
-
Gaziano, M. J. Global burden of cardiovascular disease. Braunwald’s Heart Dis. 2008, 1–19 (2008).
-
KOSIS. Major cause of death (2019).
-
Gheorghe, A. et al. The economic burden of cardiovascular disease and hypertension in low-and middle-income countries: A systematic review. BMC Public Health 18, 1–11 (2018).
Google Scholar
-
Hulzebos, E. H., Van Meeteren, N. L., De Bie, R. A., Dagnelie, P. C. & Helders, P. J. Prediction of postoperative pulmonary complications on the basis of preoperative risk factors in patients who had undergone coronary artery bypass graft surgery. Phys. Therapy 83, 8–16 (2003).
Google Scholar
-
Kassie, G. M., Nguyen, T. A., Kalisch Ellett, L. M., Pratt, N. L. & Roughead, E. E. Preoperative medication use and postoperative delirium: A systematic review. BMC Geriatr. 17, 1–10 (2017).
Google Scholar
-
Weymann, A. et al. Baseline and postoperative levels of C-reactive protein and interleukins as inflammatory predictors of atrial fibrillation following cardiac surgery: A systematic review and meta-analysis. Kardiol. Polska (Polish Heart J.) 76, 440–451 (2018).
Google Scholar
-
Odell, A., Grip, L. & Hallberg, L. R. Restenosis after percutaneous coronary intervention (PCI): Experiences from the patients’ perspective. Eur. J. Cardiovasc. Nurs. 5, 150–157 (2006).
Google Scholar
-
Koster, S., Hensens, A. G., Schuurmans, M. J. & van der Palen, J. Consequences of delirium after cardiac operations. Ann. Thorac. Surg. 93, 705–711 (2012).
Google Scholar
-
Iribarne, A. et al. Readmissions after cardiac surgery: Experience of the National Institutes of Health/Canadian Institutes of Health research cardiothoracic surgical trials network. Ann. Thorac. Surg. 98, 1274–1280 (2014).
Google Scholar
-
Hashemzadeh, K., Dehdilani, M. & Dehdilani, M. Postoperative atrial fibrillation following open cardiac surgery: Predisposing factors and complications. J. Cardiovasc. Thorac. Res. 5, 101 (2013).
Google Scholar
-
Findeisen, A. et al. Economic burden of surgical site infections in patients undergoing cardiac surgery. Eur. J. Cardio-Thorac. Surg. 55, 494–500 (2019).
Google Scholar
-
Thomas, R. J. et al. 2018 ACC/AHA clinical performance and quality measures for cardiac rehabilitation: A report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. Circul. Cardiovasc. Qual. Outcomes 11, e000037 (2018).
Google Scholar
-
Cowie, A. et al. Standards and core components for cardiovascular disease prevention and rehabilitation. Heart 105, 510–515 (2019).
Google Scholar
-
Price, K. J., Gordon, B. A., Bird, S. R. & Benson, A. C. A review of guidelines for cardiac rehabilitation exercise programmes: Is there an international consensus?. Eur. J. Prevent. Cardiol. 23, 1715–1733 (2016).
Google Scholar
-
Turk-Adawi, K. I. & Grace, S. L. Narrative review comparing the benefits of and participation in cardiac rehabilitation in high-, middle-and low-income countries. Heart Lung Circ. 24, 510–520 (2015).
Google Scholar
-
Bartels, M. N., Whiteson, J. H., Alba, A. S. & Kim, H. Cardiopulmonary rehabilitation and cancer rehabilitation. 1. Cardiac rehabilitation review. Arch. Phys. Med. Rehabil. 87, 46–56 (2006).
Google Scholar
-
Thomas, R. J. et al. AACVPR/ACCF/AHA 2010 update: Performance measures on cardiac rehabilitation for referral to cardiac rehabilitation/secondary prevention services: A report of the American Association of Cardiovascular and Pulmonary Rehabilitation and the American College of Cardiology Foundation/American Heart Association Task Force on Performance Measures (Writing Committee to Develop Clinical Performance Measures for Cardiac Rehabilitation). Circulation 122, 1342–1350 (2010).
Google Scholar
-
Turk-Adawi, K. et al. Cardiac rehabilitation availability and density around the globe. EClinicalMedicine 13, 31–45 (2019).
Google Scholar
-
West, R. R., Jones, D. A. & Henderson, A. H. Rehabilitation after myocardial infarction trial (RAMIT): Multi-centre randomised controlled trial of comprehensive cardiac rehabilitation in patients following acute myocardial infarction. Heart 98, 637–644 (2012).
Google Scholar
-
Onishi, T. et al. Effects of phase III cardiac rehabilitation on mortality and cardiovascular events in elderly patients with stable coronary artery disease. Circ. J. 74, 709–714 (2010).
Google Scholar
-
Dendale, P. et al. Cardiac rehabilitation reduces the rate of major adverse cardiac events after percutaneous coronary intervention. Eur. J. Cardiovasc. Nurs. 4, 113–116 (2005).
Google Scholar
-
Dunlay, S. M., Pack, Q. R., Thomas, R. J., Killian, J. M. & Roger, V. L. Participation in cardiac rehabilitation, readmissions, and death after acute myocardial infarction. Am. J. Med. 127, 538–546 (2014).
Google Scholar
-
Thomas, E. et al. Effect of cardiac rehabilitation on 24-month all-cause hospital readmissions: A prospective cohort study. Eur. J. Cardiovasc. Nurs. 18, 234–244 (2019).
Google Scholar
-
Kim, C. et al. Do cardiac rehabilitation affect clinical prognoses such as recurrence, readmission, revascularization, and mortality after AMI?: Systematic review and meta-analysis. Ann. Rehabil. Med. 45, 57–70 (2021).
Google Scholar
-
Scalvini, S. et al. Impact of in-hospital cardiac rehabilitation on mortality and readmissions in heart failure: A population study in Lombardy, Italy, from 2005 to 2012. Eur. J. Prevent. Cardiol. 2019(26), 808–817 (2019).
Google Scholar
-
Naami, R. et al. Cardiac rehabilitation performance predicts 1-year major adverse cardiovascular events. Clin. Cardiol. 45, 1036–1043 (2022).
Google Scholar
-
Prior, P. L. et al. Comprehensive cardiac rehabilitation for secondary prevention after transient ischemic attack or mild stroke. J. Cardiopulmon. Rehabil. Prevent. 37, 428–436 (2017).
Google Scholar
-
Reibis, R. et al. Management and outcomes of patients with reduced ejection fraction after acute myocardial infarction in cardiac rehabilitation centers. Curr. Med. Res. Opin. 31, 211–219 (2015).
Google Scholar
-
Long, L. et al. Exercise-based cardiac rehabilitation for adults with heart failure. Cochrane Database Syst. Rev. https://doi.org/10.1002/14651858.CD003331.pub5 (2019).
Google Scholar
-
Bjarnason-Wehrens, B. et al. Exercise-based cardiac rehabilitation in patients with reduced left ventricular ejection fraction: The Cardiac Rehabilitation Outcome Study in Heart Failure (CROS-HF): A systematic review and meta-analysis. Eur. J. Prevent. Cardiol. 27, 929–952 (2020).
Google Scholar
-
Do Simon, M., Do Korn, K., Cho, L. & Do, R. C. Cardiac rehabilitation: A class 1 recommendation. Clev. Clin. J. Med. 85, 551 (2018).
Google Scholar
-
Yan, K., Liang, I., Ravellette, K., Srikanthan, P. & Horwich, T. Association between body composition and major adverse cardiovascular outcomes and all-cause mortality in cardiac rehabilitation patients with coronary artery disease. J. Am. Coll. Cardiol. 81, 1719 (2023).
Google Scholar
-
Jallow, H., Chacin-Suarez, A., Medina-Inojosa, J., Bonikowske, A. & Olson, T. P. Major adverse cardiovascular events in heart failure patients with multimorbidity undergoing cardiac rehabilitation: A community cohort. J. Am. Coll. Cardiol. 79, 1590 (2022).
Google Scholar
-
Kim, S. H., Ro, J. S., Kim, Y., Leigh, J. H. & Kim, W. S. Underutilization of Hospital-based cardiac rehabilitation after acute myocardial infarction in Korea. JKMS 35, e262 (2020).
Google Scholar
-
Im, H. W. et al. Barriers to outpatient hospital-based cardiac rehabilitation in Korean patients with acute coronary syndrome. Ann. Rehabil. Med. 42, 154–165 (2018).
Google Scholar
-
Ades, P. A., Khadanga, S., Savage, P. D. & Gaalema, D. E. Enhancing participation in cardiac rehabilitation: Focus on underserved populations. Progress Cardiovasc. Dis. 70, 102–110 (2022).
Google Scholar
-
Turk-Adawi, K., Sarrafzadegan, N. & Grace, S. L. Global availability of cardiac rehabilitation. Nat. Rev. Cardiol. 11, 586–596 (2014).
Google Scholar
Acknowledgements
We would like to thank the colleagues from the Department of Public Health, Graduate School of Yonsei University for advice on this manuscript.
Author information
Authors and Affiliations
Contributions
I.S.S. conceived of the presented idea. I.S.S. and C.J.L. developed the theory and performed the computations. S.-Y.J., J.M.N. and Y.S.P. verified the analytical methods. E.C.P. and C.J.L. encouraged In S.S. and Y.S.P. to investigate this study and supervised the findings of this work. All authors discussed the results and contributed to the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary Tables.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
Reprints and Permissions
About this article
Cite this article
Song, I.S., Park, Y.s., Jang, SY. et al. Impact of cardiac rehabilitation on cardiovascular event in Korea.
Sci Rep 13, 19146 (2023). https://doi.org/10.1038/s41598-023-46503-3
-
Received: 07 May 2023
-
Accepted: 01 November 2023
-
Published: 06 November 2023
-
DOI: https://doi.org/10.1038/s41598-023-46503-3
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.