Infection
Antibiotics that fight deadly infections in babies are losing their power
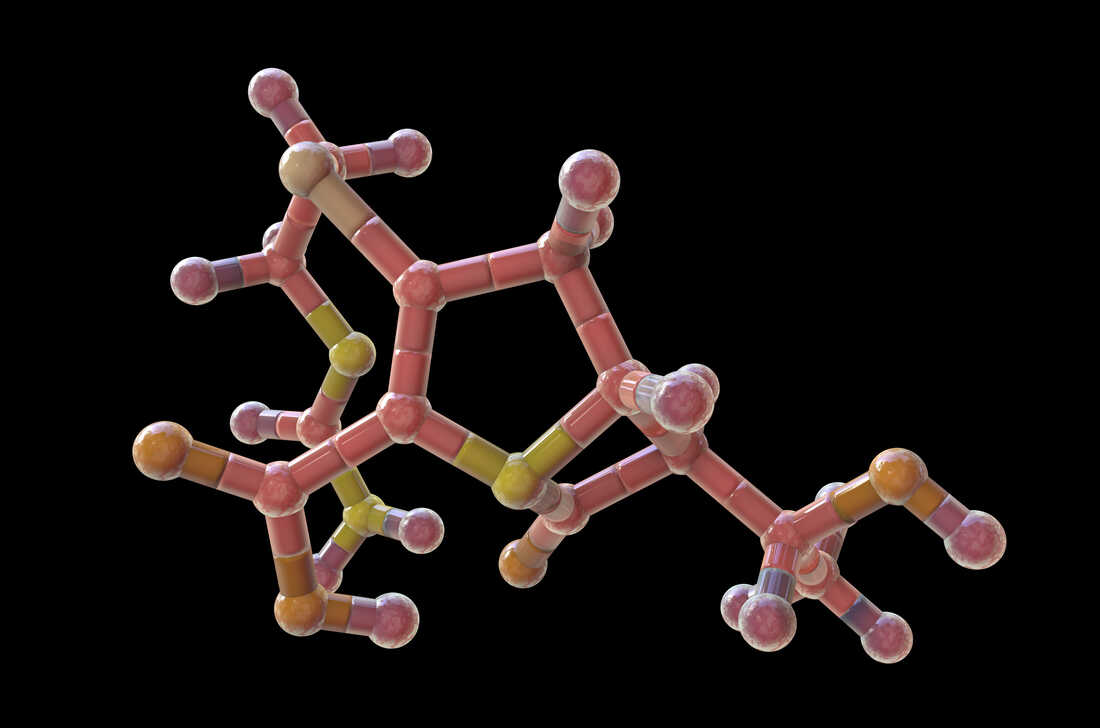
The above illustration depicts a molecular model for a carbapenem drug. The carbapenem group of antibiotics is the last resort for antibiotic-resistant infections and is approved for children. But carbapenems are not widely used because they’re expensive, they’re administered by IV — and doctors are concerned that bacteria could develop resistance to these antibiotics.
Kateryna Kon/Science Photo Library /Getty Images
Kateryna Kon/Science Photo Library /Getty Images
The drugs aren’t working as well as they used to.
That’s the sobering takeaway from new research published in The Lancet Regional Health – Southeast Asia last week: The most commonly prescribed antibiotics in Southeast Asia are now only 50% effective at treating sepsis and meningitis in newborns.
And that’s a serious setback. Sepsis kills 1 in 5 patients. Meningitis is responsible for a quarter of million deaths a year – half among children under the age of 5. Overall, childhood infections are responsible for over 550,000 deaths each year.
Why aren’t the drugs doing their job? It’s because overuse of those drugs has led to the evolution of antimicrobial resistant infections – bacteria and other diseases that are no longer knocked out by treatment.
Dr. Phoebe Williams, a physician and lecturer at the University of Sydney, Australia School of Medicine and lead author of the new research, says that these antimicrobial resistant infections are responsible for “around 5 million deaths each year” of both children and adults.
Roughly 1 million of those deaths each year occur in Southeast Asia.
Babies are especially vulnerable. While an adult’s immune system is often strong enough to fight off these infections, children who haven’t had the chance to build up their immunity suffer the brunt of the consequences.
WHO’s recommended treatments are outdated
In the last 30 years, better health care for mothers and infants has helped cut child mortality in half, according to the World Health Organization; deaths have dropped from 5 million per year in 1990 to 2.4 million in 2020. But infections still pose one of the greatest threats to newborns. And the rise of these antimicrobial resistant infections is a major obstacle for the U.N.’s goal of ending all preventable neonatal deaths by 2030.
Williams’ research shows that in Southeast Asia these infections are increasingly antimicrobial resistant. “One of the units we work with in the Philippines, for example, their mortality rates in neonatal sepsis have gone from being about 20% ten years ago to 75% in the last 2 years,” Williams says.
It’s not just the Philippines. The new research shows that antimicrobial resistance is becoming a bigger problem “across low- and middle-income countries in Southeast Asia and the Pacific,” according to Ramanan Laxminarayan, a senior research scholar at Princeton University who wasn’t involved in the new research.
Among the research findings is the discovery that many of the drugs recommended in the 2013 World Health Organization guidelines for treating childhood infections no longer work.
According to the research, ceftriaxone, one of the recommended drugs, is now only effective at treating 1 in 3 neonatal meningitis cases. Another recommended drug, gentamicin, only cures neonatal sepsis and meningitis half the time.
Laxminarayan says that the WHO guidelines are being revised to recommend more effective treatments. In the meantime, many clinicians in the affected countries are left to figure out the most appropriate course of action themselves.
Overcrowded hospitals and overuse of drugs are responsible
In many places, a lack of health-care resources exacerbates the antimicrobial resistance problem that is growing worldwide. “When you have one nurse looking after 15 to 20 babies, they might not have the time to wash their hands between every baby,” Williams says.
Williams says that in this setting antimicrobial resistant infections can spread “very quickly.” And when the drugs don’t work, there’s little else that can be done.
Williams says that the solution is to take a closer look at both old and new medicines to identify the most effective treatments for children.
She says that using older drugs “is probably one of our strongest bets because those agents are off patent.” So cheaper generic versions are available now that the original patents have expired. And because these medications haven’t been widely used for years, some infections may no longer be resistant to them.
Newer drugs that can fight off these antimicrobial resistant infections have been developed but rarely get approved for use in children. Williams says that “since the year 2000, 40 antibiotics have been licensed for adults and 4 in babies, despite babies having a far bigger burden of AMR.” Williams says that the reason many of these drugs don’t get approved for children is because they require different dosing regimens than adults. Figuring out the correct dose for children is often not a priority when companies first seek approval.
Overprescription of antibiotics to adults and their widespread use in agriculture all contribute to the growing number of antimicrobial resistant infections, notes Williams.
A class of drugs called carbapenems work well … for now
One class of drug that Williams’ research has shown to still be effective and that is approved for children are carbapenems, a collection of powerful antibiotics containing many different drugs that are given by IV and often used as a last resort for treating bad infections. Carbapenems typically aren’t prescribed unless absolutely necessary because they’re expensive, the IV is an invasive element and they’re not widely available in every country.
“They’re not in the WHO guidelines,” Williams says, but “we know many clinicians globally are now going to them as a first-line agent.”
Carbapenems may currently be the most effective antibiotic available, but resistance is growing to them too. Using this ‘last resort’ drug as a first line of defense in the long run will make the antimicrobial resistance problem worse.
Even now the carbapenems don’t always work. “This particular study shows only 81% coverage [from carbapenems] which means that 19% of the time those drugs are not going to work,” Laxminarayan says. “I don’t know about you, but I wouldn’t want to have a child with an infection where 19% of the time the most effective drug that I have doesn’t work and the child is at risk of dying.”
Both Laxminarayan and Williams stress that the paper’s findings are not confined to southeast Asia. “There’s tens of thousands of carbapenem-resistant infections in the U.S. each year,” Williams says. “Bugs don’t respect borders, as we’ve seen with COVID-19.”
It’s a problem Laxminarayan thinks should have been addressed a long time ago. “Unfortunately, the world only responds to crises and now we’re seeing a crisis with newborn survival,” he says.
Max Barnhart is a science journalist and a Ph.D. candidate studying the evolution of heat-stress resistance in sunflowers at the University of Georgia.